- (2011) Volume 12, Issue 6
Everson LA Artifon1, Adriana Vaz Safatle-Ribeiro1, Flávio Coelho Ferreira1, Luiz Poli-de-Figueiredo1, Samir Rasslan1, Francisco Carnevale1, José Pinhata Otoch1, Paulo Sakai1 and Michel Kahaleh2
1University of Sao Paulo. São Paulo, SP, Brazil.
2University of Virginia Health System. Charlottesville, VA, USA
Received September 10th, 2011 - Accepted September 30th, 2011
Context To demonstrate an EUS-guided biliary drainage in patient with gastrointestinal tract modified surgically. Case report An EUS guided access to the left intra hepatic duct, followed by an antegrade passage of a partially self-expandable metal stent that was removed by using an enteroscope, in one patient with hepatico-jejunal anastomosis. There were no early or delayed complications and the procedure was effective in relieving jaundice until the self-expandable metal stent was removed, 3 months later. A cholangiogram was obtained via enteroscopy, after removal of self-expandable metal stent, and found to be normal. The patient had an uneventful evaluation afterwards. Conclusion The indication of these procedures must be made under a multidisciplinary view while sharing information with the patient or legal guardian. EUS-guided biliary drainage is feasible when performed by professionals with expertise in biliopancreatic endoscopy and advanced echo-endoscopy and should be performed currently under rigorous protocol in educational institutions.
Biliary Tract; Drainage; Endoscopy, Gastrointestinal; Endosonography; Jaundice, Obstructive
The standard procedure for biliary drainage is transpapillary drainage during endoscopic retrograde cholangiography. However, endoscopic retrograde cholangiography may not be possible in patients with inaccessible biliary orifice, such as patient with surgically altered anatomy or tumoral stenosis of the duodenum [1]. In these cases, percutaneous transhepatic biliary drainage and surgical intervention can be offered, but are both associated with significant morbidity [2].
A 45-year-old female with post-cholecystectomy biliary stricture underwent a hepaticojejunostomy with Roux-en-Y reconstruction after developing obstructive symptoms. One year later, the patient presented with acute obstructive jaundice. Abdominal CT demonstrated intra- and extra-hepatic biliary dilation. Single balloon enteroscopy with endoscopic retrograde cholangiography was attempted but was not successful, due to the inability to cross the anastomotic stricture with guidewire.
Since the patient declined further surgery or percutaneous drainage, she was offered an EUS guided decompression and was specifically consented for the procedure. Our investigational review committee considered those procedures as extension of currently available endoscopic procedures.
The left intrahepatic duct was visualized using a linear echoendoscope (GF-UCT140AL5, Olympus America, Melville, NY, USA) placed in the remnant stomach. The dilated left intrahepatic duct was punctured, in a transhepatic approach, with a 19-gauge FNA needle (EUSN-19-T, Cook Medical, Bloomington, IN, USA) through the gastric wall after using Doppler to avoid any intervening vessels. Bile was aspirated and contrast was injected to demonstrate biliary opacification. A dilated left intrahepatic duct, with a severe stenosis in the hepatico-jejunal anastomosis was observed (Figure 1).
A 0.035-inch guidewire was passed into the jejunum, through the stenosis. The needle was withdrawn maintaining the position of the guidewire, and a needle knife (Boston Scientific, Natick, MA, USA) was advanced over the guidewire (Figure 1) using minimal cautery, creating a fistula between the stomach and the biliary tree. After EUS-guided puncture of the bile duct it is necessary to perform some sort of dilation to facilitate the self-expandable metal stent’s passage upstream, which can be done by using some accessories such as cystotome, needle-knife catheter or different size of balloon catheter, as reported here.
Contrast was injected to demonstrate the jejunal position of the guidewire, and showing the length of the stenosis (Figure 2). A 6 mm guidewire balloon dilation was performed, followed by the placement of a partially covered self-expandable metallic stent (10x60 mm, Wallflex, Boston Scientific, Natick, MA, USA), across the anastomosis (Figure 3). Adequate contrast drainage was observed (Figure 4).
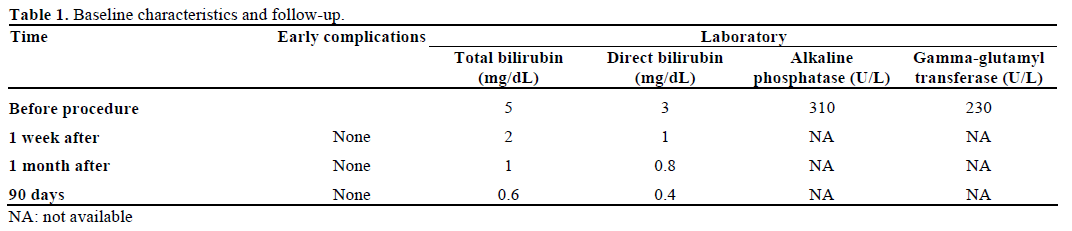
There were no early or delayed complications and the procedure was effective in relieving jaundice at 1 week until 90-day follow-up (Table 1).
After 3 months the covered self-expandable metal stent was removed during a single-balloon enteroscopy using a snare (Figures 5 and 6). A cholangiogram was obtained via enteroscopy and found to be normal.
During follow-up a decrease on bilirubin levels was seen and the patient had a uneventful evaluation.
EUS guided biliary access for minimally invasive approach to biliary obstruction has gained increasing importance in the palliation of biliary diseases but it is still debatable on benign strictures. Temporary placement of self-expandable metal stent offers a potential alternative to surgery or percutaneous transhepatic cholangiography on patients that failed to respond to endoscopic retrograde cholangiopancreatography with plastic stents, with a successful recanalization rate was up to 90% after a median follow-up of 12 months after removal as reported by Kahaleh et al. elsewhere [3]. Percutaneous transhepatic self-expandable metal stent placement was first described by Irving et al. in 1989. It is a well-established technique with technical and clinical success of 90% and 77% to 98%, respectively. However, it has complication rates from 8% to 30%, including biliary fistula, cholangitis, peritonitis, sepsis, hematoma and liver abscesses [4]. EUS-rendezvous to obtain bile duct access was first performed by Mallery et al. in 2004. Transmural drainage includes EUSguided choledochoduodenostomy [1], EUS-guided hepaticogastrostomy [5] and EUS-guided choledochoantrostomy.
Rendezvous attempt should be made when it is possible to access the guidewire passed transpapillary (through EUS guided puncture) by using a duodenoscope. However, if this is not possible, as in cases of altered anatomy such as the one described, there is the option to perform a single-step procedure and achieve biliary drainage through antegrade access with transpapillary passage of the guidewire. EUS-guided transhepatic anterograde self-expandable metal stent placement for biliary obstruction, in a single session, was described by Nguyen-Tang et al. in 2010 [6].
Complications related to the EUS guided biliary drainage such as stent migration, bile leakage, pneumoperitoneum and cholangitis [5, 7] were not seen in this case.
EUS guided biliary drainage is a minimally invasive procedure in expert hands. Studies published by Kahaleh et al. and Maranki et al. showed a technical success rate of 84% to 100%, clinical success on achieving biliary drainage of 83% to 91% with overall complication rate of 16% to 17%, including minor bleeding, bile leak and pneumoperitoneum [2, 8]. This case illustrates a less aggressive and yet interesting alternative for drainage in those patients with gastrointestinal tract modified surgically. Prospective studies to assess feasibility and safety are necessary.
The authors stated that there are no conflicts of interest in this manuscript