Case Report - (2025) Volume 33, Issue 1
Received: 06-Feb-2024, Manuscript No. IPQPC-24-19028; Editor assigned: 08-Feb-2024, Pre QC No. IPQPC-24-19028 (PQ); Reviewed: 23-Feb-2024, QC No. IPQPC-24-19028; Revised: 06-Feb-2025, Manuscript No. IPQPC-24-19028 (R); Published: 13-Feb-2025, DOI: 10.36648/1479-1064.33.1.45
Background: There is more evidence that COVID-19 infection affects the glucose metabolism. Diabetic Ketoacidosis (DKA) is a life-threatening medical emergency requiring urgent treatment. There are few case reports of Euglycemic DKA (EDKA) occurring in pregnant patients with pre-existing either type 1, type 2 Diabetes Mellitus (DM) and Gestational Diabetes Mellitus (GDM). However, this is a case report of patient developing EDKA without any previous history or risk factors for developing GDM in pregnancy and who developed GDM following COVID-19 infection in pregnancy.
Case presentation: We describe a case report of 29 year old Gravida 2+0 patient without previous history of DM complicated with EDKA at 28 weeks of pregnancy following COVID 19 infection. EDKA needs a higher level of suspicion for diagnosis and is associated with increased fetal morbidity and mortality, if left undiagnosed and untreated.
Conclusion: We discussed the possible causes, differential diagnosis, and a multidisciplinary management plan for euglycemic diabetic ketoacidosis.
COVID-19; Diabetic ketoacidosis; Euglycemic DKA; Pregnancy
MDT: Multi-Disciplinary Team, GDM: Gestational Diabetes Mellitus, DKA: Diabetic Keto Acidosis, BMI: Body Mass Index, CTPA: Computer Tomography Pulmonary Angiography, OGTT: Oral Glucose Tolerance Test, EDKA: Diabetic Ketoacidosis, DM: Diabetic Mellitus
COVID-19 can precipitate ketosis and ketoacidosis without diabetes mellitus. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus that causes Covid-19, binds to Angiotensin-Converting Enzyme 2 (ACE2) receptors, which are expressed in key metabolic organs and tissues, including pancreatic beta cells, adipose tissue, the small intestine, and the kidneys. Thus, it is plausible that SARSCoV- 2 may cause pleiotropic alterations of glucose metabolism that could complicate the pathophysiology of preexisting diabetes or lead to new mechanisms of disease. Diabetic Ketoacidosis (DKA) is a life-threatening medical emergency requiring urgent treatment. There are few case reports of Euglycemic DKA (EDKA) occurring in pregnant patients with pre-existing either type 1, type 2 Diabetes Mellitus (DM) and Gestational Diabetes Mellitus (GDM). However this complication occurring in patient without any previous history of Diabetes Mellitus or risk factors for developing GDM in pregnancy seems to be rare.
A 29 year old, Gravida 2+0 with a BMI of 25.5 were admitted to hospital at 28 weeks of gestation due to feeling unwell, sick and vomiting. She reported to have been tested positive for SARS CoV-2 infection 6 days earlier. However, she did not complain of chest symptoms. Fetal movements were reported as normal. She had no significant past medical history and no personal or family history of diabetes mellitus.
On admission she was unwell, tachycardic and tachypneic, saturating 98% on room air initially, then required 4L of oxygen. There was evidence of ketonuria and ketoacidosis. Initial ABG was suggestive of metabolic acidosis (pH 7.29, pCO2 3.1 kpa, HCO3 10.9, BE -13.7 mmol/L, lactate <1, CRP 108, blood ketones 4.7 mmol/L, HbA1c 39, blood glucose 4 mmol/L.
COVID 19 prognosticators showed a ferritin level of 224 and lymphopenia. CTPA revealed extensive bilateral peripheral and broncho vascular patchy lung consolidation in keeping with COVID pneumonia. There was no evidence of pulmonary embolism. CTG was normal.
In view of the clinical findings, the differential diagnoses included worsening COVID pneumonia, metabolic ketoacidosis and starvation induced ketoacidosis.
As evident from the Table 1, we noticed that she had tachypnea and tachycardia at presentation, as depicted by blood gas and with increase in blood ketone levels. The blood glucose levels were normal in the beginning. We tried to correct the acidosis with fluid therapy initially while regularly monitored her blood gases and ketones. In the next stage the blood gases and ketone levels normalized, but we noticed the progressive increase in blood glucose levels. We started her on sliding scale therapy with insulin and her blood glucose normalized subsequently.
|
|
Day of Admission |
|||
|
0 |
2 |
3 |
5 |
|
|
pH |
7.29 |
7.33 |
7.36 |
7.44 |
|
HCO3 |
10.9 |
11.1 |
14.3 |
20.6 |
|
BE |
-13.9 |
-12.3 |
-9.8 |
-2.4 |
|
Na/K |
138/2.94 |
136.6/3.65 |
139.9/3.6 |
140/3.5 |
|
pO2 |
10.9 |
11.5 |
12.5 |
7.3 |
|
pCO2 |
3.1 |
2.8 |
3.5 |
4.1 |
|
Ketones |
4.7 |
2.9 |
2.8 |
0.5 |
|
Glucose |
5 |
12.9 |
6.4 |
10.7 |
|
Respiratory rate |
34 |
26 |
19 |
17 |
|
Pulse |
126 |
99 |
104 |
90 |
|
Sp02 |
96 |
97 |
96 |
97 |
Table 1: Patient's biochemical parameters on admission to MICU and afterwards.
She was followed up with serial growth scans and OGTT 2weeks later and was diagnosed as GDM. MDT opinion was sought including obstetrician, medical team, anesthetic and critical cares out-reach team. She was cared in a high dependency unit with close monitoring of her fluid balance. She was commenced on intravenous antibiotics, thromboprophylaxis and steroid prophylaxis for fetal lung maturity. Ketoacidosis was corrected with Intravenous fluids and electrolyte replacement. The clinical parameters such as the respiratory rate and the heart rate normalized first, followed by the improvement of the biochemical parameters such as ketonaemia and even later the HCO3, K, pH and anion gap as shown in the table below. An interesting finding of note was a light increase in blood glucose and lactate levels which led to suspicion of developing GDM. Hence, she was then started on sliding scale with insulin therapy. Following this there was marked improvement in both clinical and biochemical parameters. She had no further episodes of vomiting and tolerated the solid foods well and was discharged home on full recovery. She was followed up with serial scans and OGTT, 2 weeks later and was diagnosed as GDM.
The early diagnosis of EKA helped correcting ketoacidosis with fluid management, electrolyte replacement and sliding scale therapy to normalize the ketones and glucose levels (Table 2).
| Stage | Glucose levels | Ketones | Acidosis | Lactate | Oxygen saturation (%) | Pulse rate | Respiratory rate |
| 1 | Normal | Increased | Increased | Normal | 93 | Increased | Increased |
| 2 | Stable | Increased | Increased | 96 | Increased | Increased | |
| 3 | Increased | Stable | Stable | Increased | 98 | Decreased | Decreased |
| 4 | On Insulin | Stable | Stable | Stable | 98 | Decreased | Decreased |
Table 2: Data of a patient showed clinical improvement in staged phase as per the treatment.
Stage 1: In stage 1, the patient had ketoacidosis and the treatment was based as per protocol and MDT discussion. She underwent COVID investigations and treatment in form of steroids, antibiotics, steroid prophylaxis and oxygen therapy.
Stage 2: In stage 2 the patient showed signs of clinical improvement with gradual improvement in bicarbonate, potassium and base excess. Lactate levels showed an incremental value. Her oxygen saturation improved by this period and her oxygen requirement plummeted to 0-1 litre/ minute.
Stage 3: We initiated sliding scale when both pre and post prandial blood glucose levels were raised repeatedly.
We realized the similarities in clinical progression of this patient with EDKA inspite of the absence of previous diabetic history.
Stage 4: There was improvement seen clinically and biochemical markers normalized. She was discharged home.
Munro et al first described Euglycemic DKA in 1973 among type 1 DM [1,2]. Common causes of EDKA mentioned in literature currently are as low caloric intake, fasting or starvation, pregnancy, pancreatitis, cocaine intoxication, prolonged vomiting or diarrhea, insulin pump use and of late use of SGLT2 inhibitors like empagliflozin and canagliflozin [3].
Recently, there had been 2 case reports of patients developing euglycaemic DKA during pregnancy that can be associated with fetal morbidity and mortality if left untreated and undiagnosed. Both these pregnant women were reported positive for SARS-CoV-2 and only one of these pregnant women had previous history of DM [4].
The pregnancy is a diabetogenic state. As depicted in Figure 1, the production of certain hormones (prolactin, human placental lactogen, progesterone and cortisol) promotes insulin resistance and increases the risk of gestational diabetes mellitus. The development of GDM is based on certain pre pregnancy risk factors such as raised BMI, ethnicity, previous history of GDM, previous history of macrosomia. COVID infection during pregnancy leads to transient Beta cell dysfunction and development of GDM. In addition, normal blood glucose levels can also be associated with ketoacidosis.
Several mechanisms may contribute to this phenomenon. During pregnancy, glycogenolysis, lipolysis and ketogenesis are all increased during fasting. Increased starvation can lead to these changes. The diabetic ketoacidosis develops more quickly and at lower of blood glucose levels than in nonpregnant women. Starvation ketoacidosis is caused by short periods of fasting and may be precipitated by stressful conditions, such as a viral infection (Figure 1) [5].
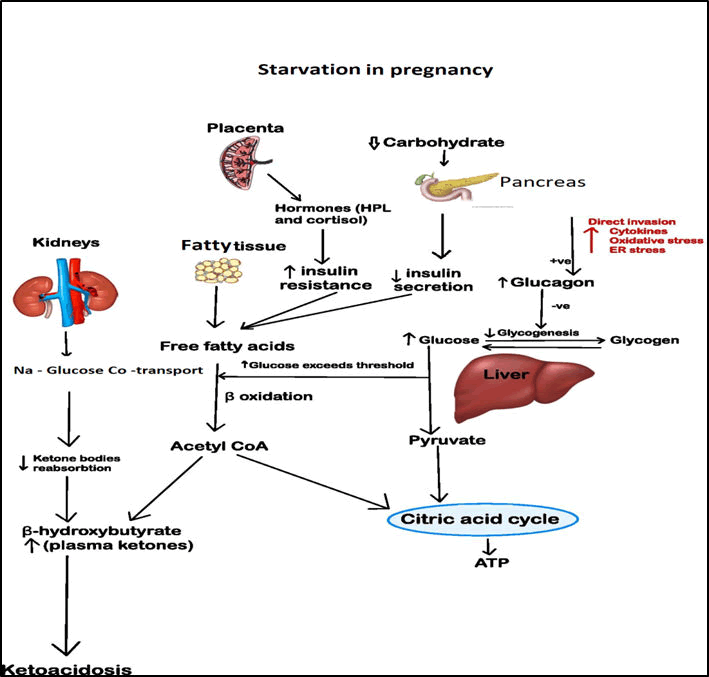
Figure 1: Demonstrates changes in ATP production pathway under stress and fasting condition in pregnancy leading to ketosis.
Ketones are produced in the liver from free fatty acids. When the ketone production exceeds its consumption, it results in ketosis, which can be clinically evident by raised blood levels of ketone bodies (β-hydroxybutyrate, acetoacetate and acetone). Ketoacidosis is a severe metabolic disorder characterized by the accumulation of ketone bodies and acidosis, is mostly seen in people with diabetes and is rarely induced by other pathological conditions. COVID-19 might accelerate fat beta-oxidation and induce ketosis, with further development of ketoacidosis.
There seems to be a direct link between COVID-19 and T2DM. In the pancreas, the SARS coronavirus (SARS-CoV, which causes SARS) binds to its receptor, the ACE2. This damages the islets and reduces insulin release. As the human endocrine pancreas expresses ACE2, the coronavirus might enter islets and cause acute β-cell dysfunction, leading to acute hyperglycemia and transient T2DM [6]. There has been increasing concern that treatment with ACE-inhibitors might facilitate over-expression of virus entry gate in target tissues. This could lead to increased risk of morbidity and mortality in patients with SARS-CoV-2 infection as shown in Figure 2 [7]. This phenomenon may well explain the development of ketoacidosis in this pregnant woman in our case report, who did not have any previous diabetic history.
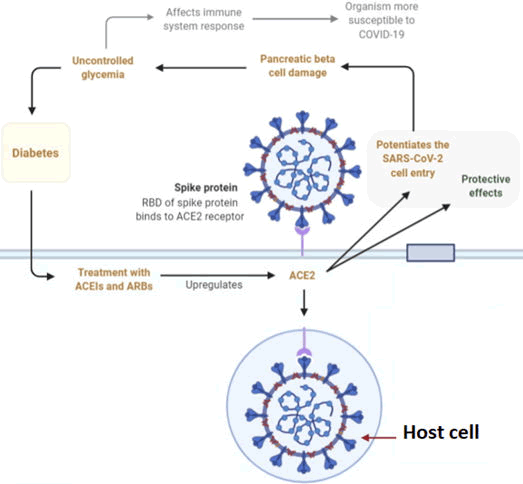
Figure 2: Demonstrates ACE2 mediated entry of SARSCoV- 2 causing pancreatic cell damage.
EDKA needs to be strategically managed and may need to be escalated to ITU, as there would be need for repeated hemodynamic monitoring and blood gas analysis. Initial focus is required on treating dehydration with initial administration of 1 to 1.5 L/hr of Hartmann’s solution as per American diabetic association recommendation [8]. In contrast to diabetic ketoacidosis, blood glucose levels are normal in EDKA, hence 5% Dextrose infusion reduces ketosis effectively combined with insulin infusion. IV supplementation of potassium would be necessary to serum levels higher than 3.5 mmol/L. Serum bicarbonate level ≥ 15 mmol/L, an anion gap ≤ 12 mmol/L, or a venous pH >7.3 would suggest correction of EDKA [9].
Schneider et al. has reported that 2-9% of all diabetic pregnancies get complicated with diabetic ketoacidosis and it would lead to fetal mortality rate of 90% [10]. Since the initial serum glucose remains normal, early diagnosis remains restricted [11]. Fetal abnormalities are proven to normalize with correction of acidosis [12]. Emergent cesarean delivery would be necessitated if the maternal condition worsens, but this is associated with high maternal morbidity and mortality. Covid-19 infection itself could be related to array of respiratory and cardiovascular derangement and management would need to be individualized.
EDKA must be considered even in non-diabetic pregnant women. It is a high risk complication, particularly when associated with other stress factors such as an infectious disease. Ketone testing should be performed systematically in cases of vomiting pregnant to quickly establish the correct diagnosis and provide the appropriate treatment. The COVID-19 infection can worsen the glucose metabolism and one should be aware of the potential to development of euglycaemic ketoacidosis during pregnancy. Therefore, we should pay attention to COVID-19 patients with ketoacidosis especially those with diabetes, to reduce the associated mortality from complications of COVID-19. Notably, the mechanism of COVID-19-induced DKA needs further research.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Taruna A, Janos D (2025) Euglycemic Ketoacidosis and Development of GDM Following COVID-19 Infection in Pregnancy: A Case Report. Qual Prim Care. 33.45.
Copyright: © 2025 Taruna A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.