Key words
discrimination, ethnicity, health outcomes,
multi-methods
Introduction
In population-based health studies, ethnicity is often
treated as an extraneous variable to be statistically
controlled at the time of analysis. When ethnicity is
studied in its own right, there remain conceptual and
analytic tensions. In broad terms, however, the definition
and use of ethnicity in the investigation of
disparities in health and health outcomes falls into
three broad categories: (1) those health effects attributable
to genetic predispositions (Anand, 1999); (2) those
health effects attributable to socio-economic context
and culturally patterned behaviours and beliefs of
the group being studied (Adamson et al, 2003); and
(3) those health effects attributable to the behaviour of
others towards the group being studied (Smedley et al,
2003).
In a clinical setting, the last of these health effects,
resulting from differential treatment by virtue of
ethnicity, remains one of the most disturbing possibilities
because it is indicative of discrimination;
treatment deliberately or unknowingly determined
or influenced by a clinician’s view about a patient’s
personal characteristics such as age, race, gender,
ethnicity and religion, above and beyond their objective
clinical relevance, which results in a worse health
outcome than if the patient had been treated on the
basis of their clinical presentation alone. The difficulty
is that when the clinical encounter is scrutinised,
allowances need to be made for variation in and the
fallibility of clinical judgements (Smedley et al, 2003),
the possible misperception of the patients and an
explicit recognition of socially constructed group
categorisation and perceived stereotypes related to
the group by other social groups (Karlsen andNazroo,
2006).Nonetheless, there is no shortage of small-scale,
targeted studies documenting the perception of racism
and racial discrimination in healthcare settings by
patients from minority ethnic groups (Barnes and
Weiner, 1999; Doescher et al, 2000; Krieger, 2001).
Under these circumstances, particularly when the
interest is not in individual clinicians but in institutionalised
or systemic bias associated with patients’
ethnicity, one of the best strategies for drawing attention
to discrimination in clinical care is in the identification
of statistical irregularities in targeted clinical
outcomes. Differential rates in the access to information,
diagnosis and treatment for a range of conditions
have all been identified as indicative of discrimination
within healthcare, making each a potentially useful
proxy indicator (Anonymous, 1999a,b; Bach et al,
1999; Canto et al, 2000; Britton et al, 2004). Most of
the epidemiological research of this kind reported in
the literature has come out of the US, driven by an
awareness of and recognised need to deal with racial
and ethnic discrimination in healthcare (LaVeist, 2002; National Research Council, 2004). However,
in the US, the exploration of disparate clinical outcomes
patterned by race and ethnicity-related discrimination
is conflated by the nature of health
funding. (The exception to the funding-related bias
is perhaps in the elderly with Medicare Managed Care
and patients in the Veterans hospitals.) Private health
insurance and wealth are both strongly associated with
good clinical outcomes, and because both are strongly
patterned by race and ethnicity, these alter the association
between ethnicity and clinical outcomes.
Research using a similar approach in the analysis of
the relationship between access to healthcare and
ethnicity as proxies for discrimination has been conducted
in the UK. However, the application of the
findings is also restricted by the complexities of the
multidimensionality of ethnicity as a construct and
socio-economic factors (Bhopal, 2004). These limitations
highlight a major challenge in epidemiological
research on discrimination and health. Beyond highlighting
the potential disparities, current approaches
do not explore the underlying service-related and other
factors that could flag potential discrimination. The
Institutes of Medicine in the US suggest factors that
include institutional practices, stereotyping and provider
bias. However, the systematic investigation of
these factors remains poor (Krieger, 2001; Smedley
et al, 2003) and the methods underdeveloped.
The aim of the current research was primarily to
explore quality of care-related clinical outcomes across
ethnic groups within the context of a universal healthcare
coverage system, thus minimising the bias faced
by researchers in countries like the US that have
differential access to health insurance. The analysis
was expected to provide preliminary data for the
development of methods for further research into
discrimination and quality of care. The underlying
assumption was that systematic discrimination would
lead to poorer outcomes for ethnic minority patients
where the outcomes rely on the quality of care. For
discrimination to occur there need to be markers of
exclusion (Reidpath et al, 2005) such as skin colour
(Comstock et al, 2004) or overt cultural or religious
practice; institutional and/or healthcare staff attitudes
that would be exclusionary or which would reflect
concerns about social distance; and patients who
would report a perception of discrimination.
Australia provides a useful setting to explore the
relationship between clinical health outcomes and
ethnicity, because of the federally funded universal
health insurance scheme. The Medicare Scheme in
Australia guarantees free or subsidised primary care
and most specialist referrals, free treatment in public
hospitals and subsidised pharmaceuticals to Australian
and New Zealand citizens, or holders of, or applicants
for, permanent migration visas. While many of the
US studies control statistically for the confounding introduced by the commercial nature of clinical care,
Australia provides a setting where technically, access is
not an issue.
Notwithstanding the availability of universal healthcare
in Australia, largely qualitative research into the
experiences of migrant groups has reported significant
negative experiences with health services (Manderson
and Allotey, 2003a). Racism is cited by ethnic minorities
as a reason for frustration with health services,
and ultimately explains their withdrawal from the
services in spite of an ongoing need for care (Allotey
et al, 2002). To date however, with the exception of
some research on the health outcomes of indigenous
Australians, there is almost no population-based
epidemiological research into clinical health outcomes
associated with patients’ ethnicity. This paper
reports an analysis investigating the relationship between
patient ethnicity and care-related clinical outcomes,
and discusses the implications for future
research into discrimination and health.
Methods
The study was based on the secondary analysis of an
existing data set described below. All analyses were
conducted using SAS 8.2 (SAS Institute Inc, 1999).
Approval for these analyses was obtained from the
Victorian Department of Human Services and its
institutional ethics committee.
Data source
The analysis was undertaken using hospital discharge
abstracts for the state of Victoria on the Eastern
seaboard of Australia. Victoria is the second largest
state in Australia (population �5 million (Australian
Bureau of Statistics, 2001) ) with high ethnic diversity.
One-quarter of the population is overseas born, with
72% from non-English-speaking regions including
Asia, Africa, Middle East, the Pacific, Eastern Europe
and South America. The Victorian Admitted Episodes
Dataset (VAED) is maintained by the Victorian State
Department of Human Services, and is based on
statutorily required data compiled by individual private
and public hospitals (Acute Health Division, 2000).
The data include demographic and clinical information
on each episode of patient care, with clinical
information coded in the format of the International
Classification of Disease-10 (ICD-10) (Australian
Modification) from July 1 1998 and the ICD-9 (Clinical
Modification) prior to that.
Ethnicity classification
Unlike in the UK, there is no administrative requirement
to collect data on ethnicity in Australia. The
approach adopted by the Australian Institute for Health
and Welfare in the reporting of immigrant health is
geographical with four categories that include: (1) UK
and Ireland; (2) other Europe; (3) Asia; and (4) an
‘other’ category which includes Africa, the Americas,
Middle East, New Zealand and the Pacific Islands
(Australian Institute of Health and Welfare, 2004).
These categories supply large enough groups to provide
sufficient statistical power in analyses; however
their merit ends there, because the extent of heterogeneity
of the countries in the groups precludes any
meaningful, theoretical, cultural or ethnic discussions.
Given the conditions required for discrimination to
occur (Reidpath et al, 2005), country of birth data
were used to recategorise patients according to perceptible
ethnic markers of exclusion. The principal
markers were English language proficiency and ‘visibility’
or visible physical difference based on likely
phenotypic physical variation from the Anglo-Celtic
Caucasian. The approach is consistent with the race
discrimination literature and serves as a more useful
conceptualisation than simple physical geography
(country of birth) (Physicians for Human Rights,
2003; Smedley et al, 2003; National Research Council,
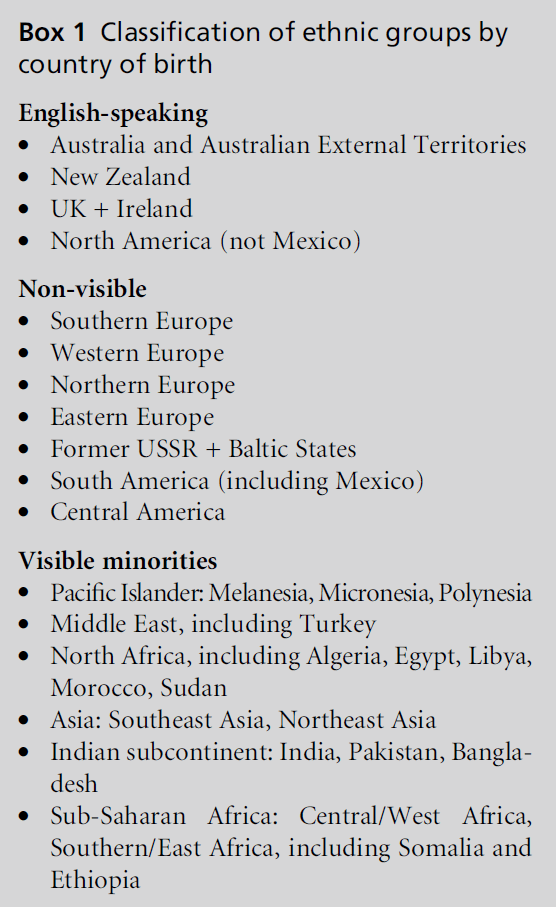
2004). There were, therefore, three major categories
(see Box 1):
1 Australian-born or overseas-born patients from
English-speaking, predominantly white countries
(e.g. Australia, New Zealand, UK, and Ireland)
2 non-visible minorities: overseas-born patients from
non-English-speaking, predominantly white countries
(e.g. Italy, Greece, and the former Yugoslavia)
3 visible minorities: overseas-born patients from
countries with largely non-white populations
and/or predominantly Islamic countries (e.g.
Afghanistan, Vietnam, and Sudan).
It is important to note here that there is an ad hoc
collection of data on Australian aboriginality, but
patients falling into this category were excluded for
two reasons. First, identification ofAboriginal patients is
often incomplete and inaccurate. Second, the antecedents
of social disadvantage of Australia’s indigenous
population preclude them being categorised with
the majority of (white) Australian-born patients.
Clinical outcomes data
The quality of care given within an institutional
setting has important implications for the clinical outcomes of any admissions episode. Given our definition
of discrimination, the conditions for the preliminary
analysis had to relate to quality of care. The
three conditions examined were attendance at cardiovascular
rehabilitation after a cardiac event or procedure,
postpartum haemorrhage and general sepsis.
Box 1: Classification of ethnic groups by
country of birth
The first indicator, attendance at cardiac rehabilitation,
was chosen primarily because cardiovascularrelated
treatments demonstrate the strongest and
most consistent evidence of ethnic disparities in the
US (Smedley et al, 2003). Among other things, cardiac
rehabilitation indicates the capacity of physicians,
surgeons, nurses and hospital physiotherapists to communicate
the importance of risk factor modification
to patients who have recently undergone a major
cardiac event in a way that motivates patients to attend
outpatient preventive services. Data were aggregated
from 66 outpatient cardiac rehabilitation programmes
in Victoria from January to December 1998, and linked
to all cases of acute myocardial infarction, coronary
artery bypass grafting and percutaneous transluminal
coronary angioplasty from the 1998 VAED. The attendance
rate was based on the number of cardiac
cases from the VAED sample linked to the rehabilitation
dataset.
We selected post-partum haemorrhage for a number
of reasons. Qualitative findings of discrimination have related largely to women’s engagement with
reproductive health services (Manderson and Allotey,
2003a); the choice of a childbirth-related condition
provided the opportunity to explore quantitative
methods of triangulation of the qualitative data. Risk
of post-partum haemorrhage also provides insight
into the quality of care for younger women, a specific
demographic group well represented in the newer
migrant groups. Post-partum hemorrhage is defined
in the Australian ICD-10-AM coding guidelines as
blood loss within 24 hours of delivery, either a 500 ml
blood loss after a vaginal delivery, or 1000 ml blood
loss after a caesarean section (National Centre for
Classification in Health, 1998, 2000). All deliveries
from 1 July 2000 to 30 June 2003 were considered for
analysis.
Sepsis exemplifies a common severe illness, which
demands high-level hospital care, often with the requirement
for intensive care services. The complexity of
its pathogenesis and treatment is often difficult to
communicate. It therefore provides a good proxy for
quality of care in hospital settings. For this analysis we
examined both differences in access to intensive care
following sepsis, and hospital mortality. Sepsis was
defined using the ICD-10-AM codes for Gram-positive,
Gram-negative, fungal, tuberculous, anaerobic and
microbiologically undefined sepsis section (National
Centre for Classification in Health, 1998, 2000). The
analysis period extended four years, from 1 July 1999
to 30 June 2003.
Data analysis
Multivariable logistic regression was used to examine
the relationship between ethnicity (visibility) and
healthcare/outcome. The covariates in the adjusted
models included socio-economic status, proximity to
services, co-morbidities, and type of hospital: public
hospitals funded through Medicare versus private
hospitals covered by private health insurance. Private
insurance carriers can elect to be hospitalised at a
public hospital.
The socio-economic status of individual patients
was estimated using the Australian Bureau of Statistics
Socio-Economic Indicator for Advantage, SEIFA
(Australian Bureau of Statistics, 2003). Based on
previous work, a dichotomous variable was generated
reflecting those in the lowest quartile on index of
economic resources in comparison to the top three
quartiles (Australian Bureau of Statistics, 2003). Proximity
to services was estimated using the Accessibility/
Remoteness Index of Australia (ARIA) (Commonwealth
Department of Health and Aged Care, 2001),
which marks the proximity of a patient’s residence to a
wide range of goods and services, including medical
services (Commonwealth Department of Health and Aged Care, 2001). A dichotomous classification was
generated distinguishing patients residing in areas
classified as highly accessible, with no physical restriction
on access to most goods and services, from the
rest. Co-morbidities were measured using an ICD-10-
AMversion of the Charlson co-morbidity index in the
cardiac analysis (Sundararajan et al, 2004). The type of
hospital in which the patient was treated was classified
as public, private, or other. Less than 10% received their
care as private patients at public hospitals; other
indicated patients such as veterans who were funded
under a different Commonwealth government health
insurance scheme from Medicare, but nonetheless
received care in public hospitals.
Results
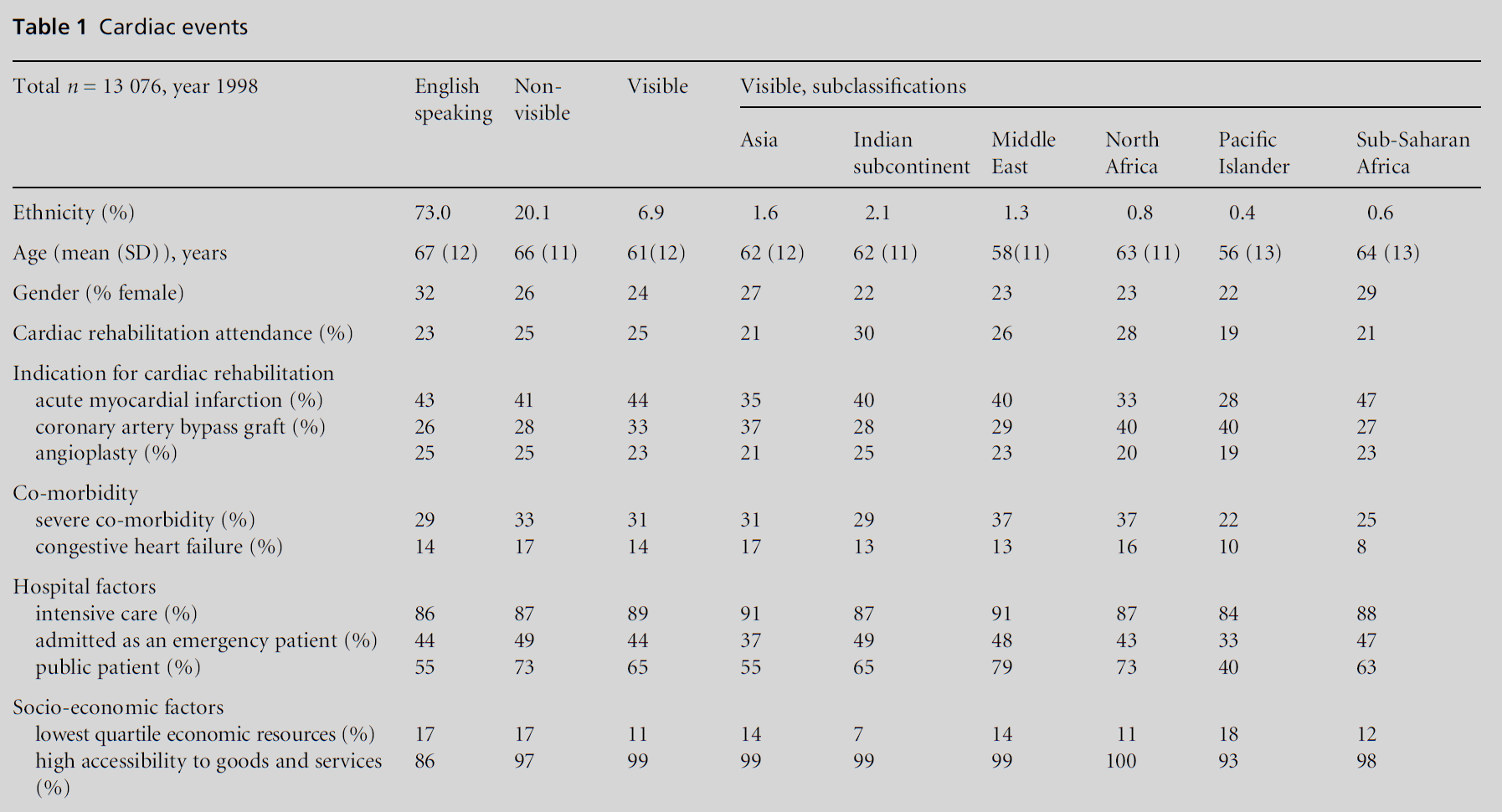
Access to cardiac rehabilitation
In 1998, 13 076 patients were hospitalised for a myocardial
infarction, coronary artery bypass graft or an
angioplasty. Their mean age was 66 years with a
standard deviation of 12. Thirty percent were women,
and 73% were English speaking (see Table 1). Overall,
23.7% of cardiac patients attended rehabilitation,
whereas 23.0% of English-speaking cardiac patients
attended rehabilitation.
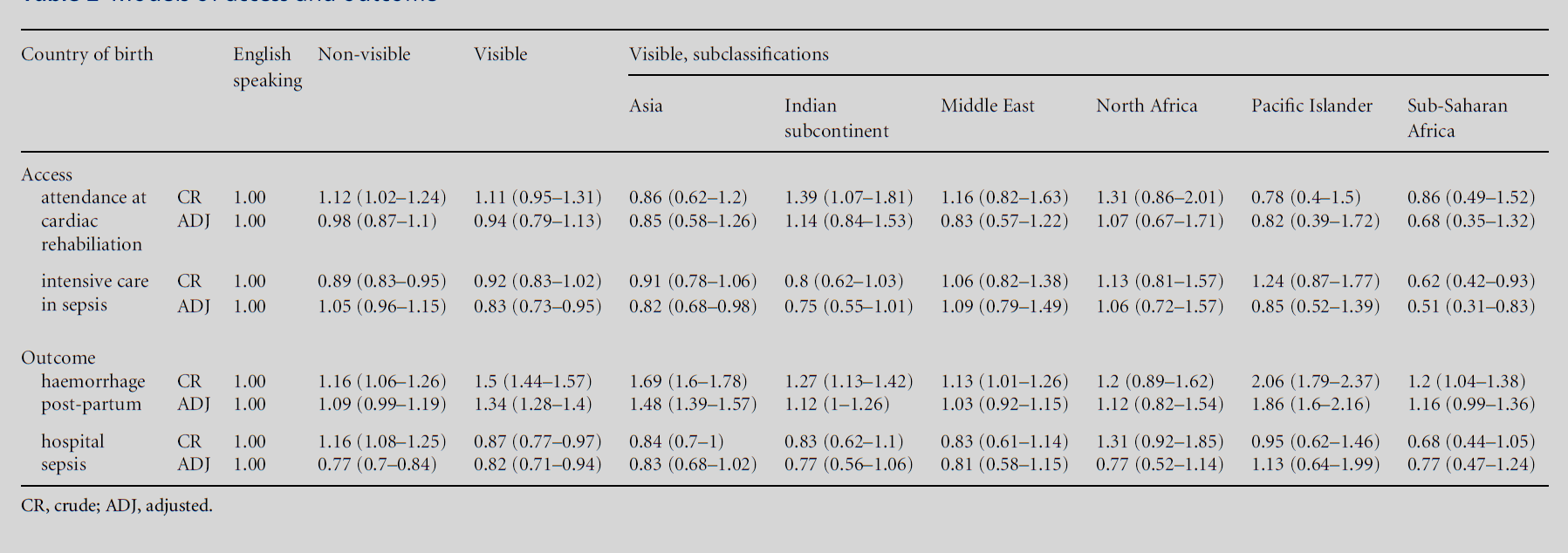
In a crude logistic regression model, with the
English-speaking group as the reference, the odds of
attending rehabilitation were higher for patients from
the Indian subcontinent in the visible ethnic minority
category (odds ratio and 95% confidence interval, 1.39
(1.07, 1.81)) and from non-visible countries (1.12
(1.02, 1.24)) (see Table 2). In the fully adjusted model,
covariates with higher odds of attending rehabilitation
included male gender, younger age, cardiac bypass as
the cardiac event, lower co-morbidity, intensive care
during admission, admission as an emergency patient,
private patient type, living in an area classified as being
in the highest quartile of economic resources, and
having high accessibility to goods and services. Ethnicity
did not relate to attendance at cardiac rehabilitation,
with the two groups showing higher odds of
attendance in the crude analysis no longer significantly
different from the English-speaking group.
Post-partum haemorrhage
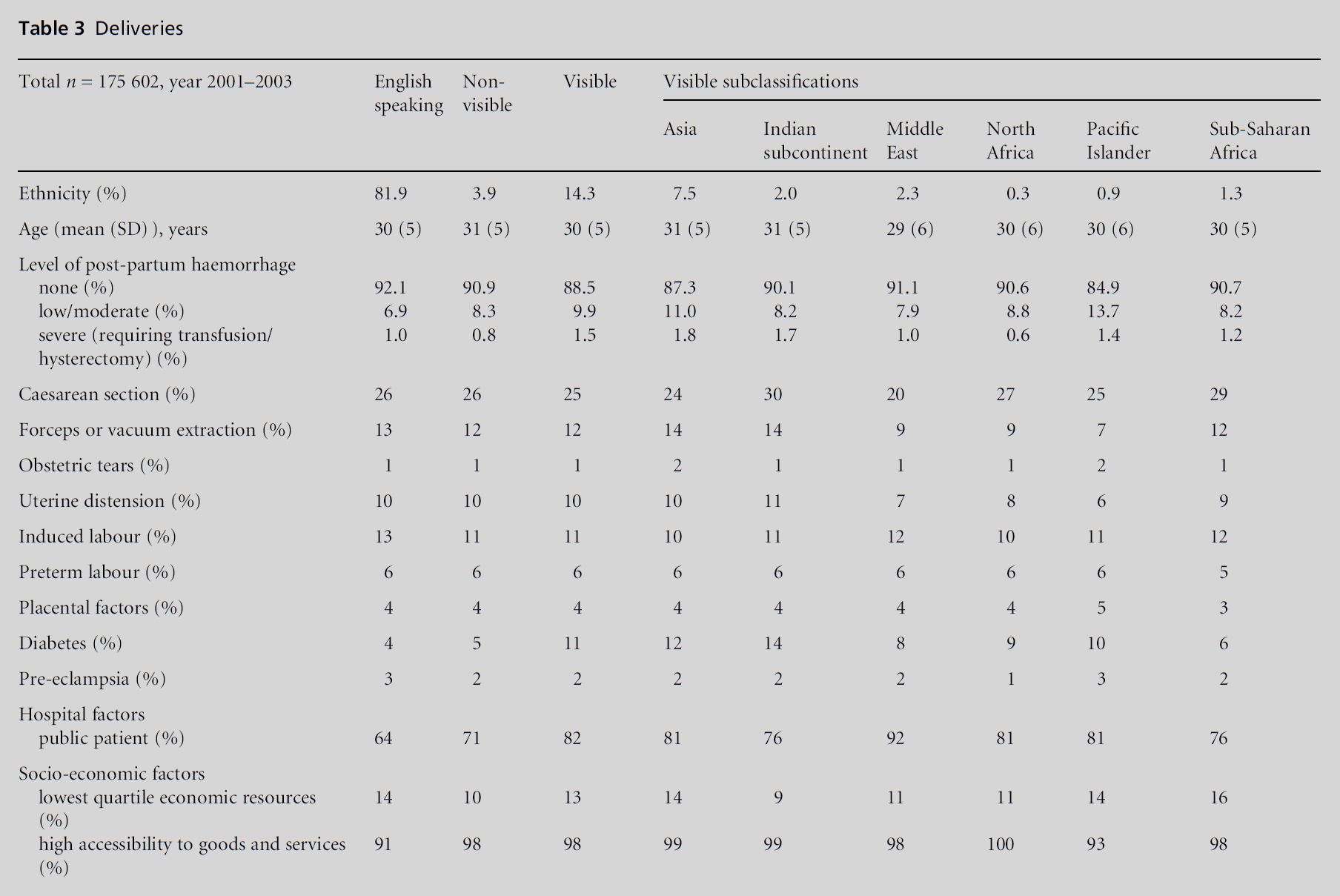
Overall 8.5% of deliveries from both minority categories
were complicated by post-partum haemorrhage,
in comparison to a rate of 7.9% of women born
in English-speaking countries (see Table 3). In the
crude model, women from visible and non-visible
minority groups all had an elevated chance of postpartum
haemorrhage (Table 2). The adjusted model for the odds of post-partum haemorrhage after delivery
included other risk factors which may have the
potential to alter the relationship between ethnicity
and the risk of post-partum haemorrhage. In addition
to age, patient type, that is public, private, other, area of
residence in the lowest quartile of economic resources,
area of residence with high accessibility to goods and
services, these included processes which increase uterine
atony such as uterine distension, induction of
labour, preterm labour, rapid labour, and prolonged
labour; placental factors; chorioamnionitis; genital
tract trauma; coagulopathies; type of delivery such
as spontaneous vertex, caesarean section, forceps,
vacuum, breech; and other factors such as diabetes
in pregnancy, gestational and otherwise, and preeclampsia.
The risk was higher in visible minorities,
although in a fully adjusted model, only women from
Asia and the Pacific Islands appeared to have a higher
risk. Women who delivered at private hospitals had a
lower risk compared to those delivering at public
hospitals (data not shown).
Transfer to an intensive care bed in
sepsis
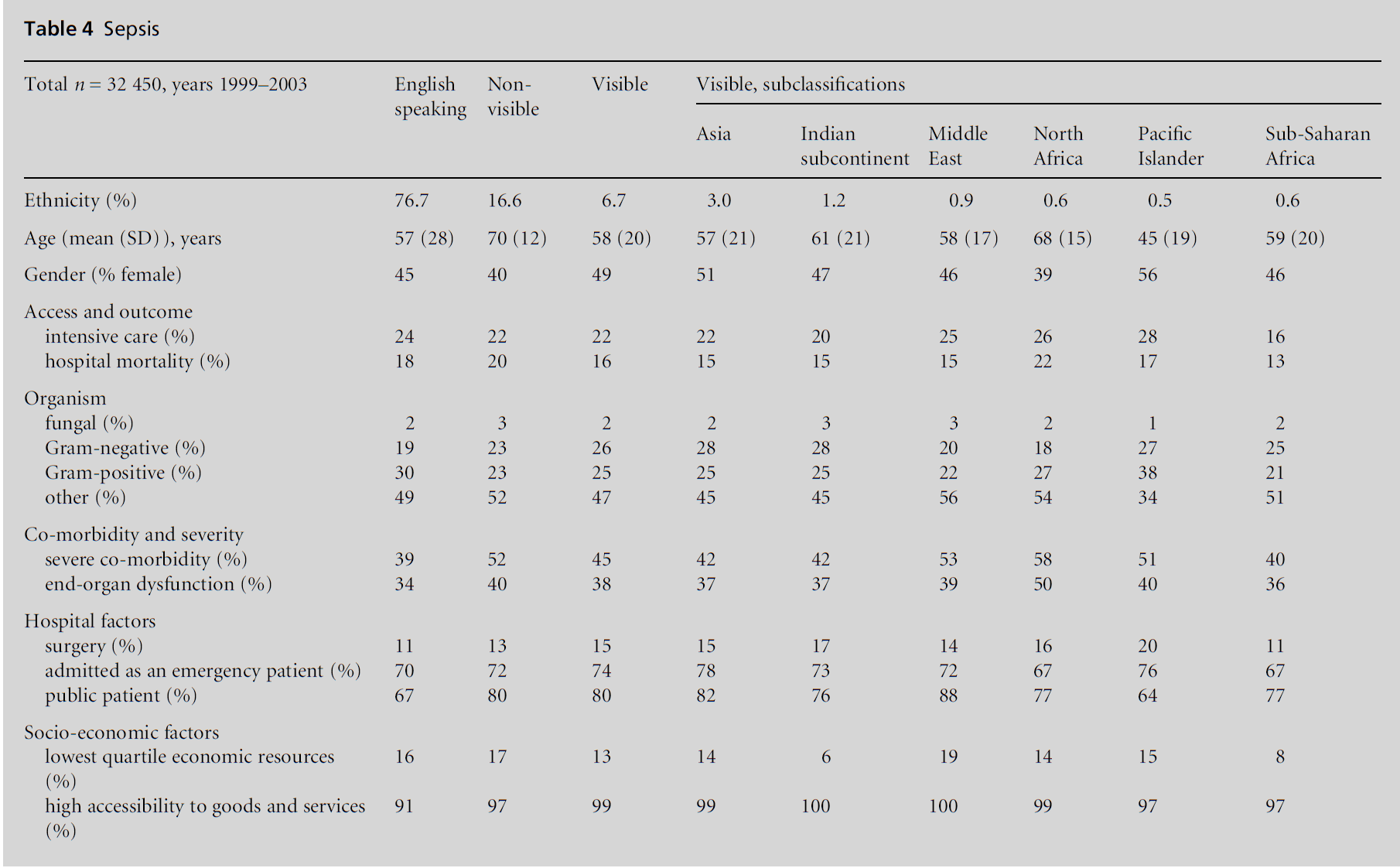
Overall, 23.3% of sepsis patients transferred to intensive
care during hospitalisation, very similar to the
figure of 23.7% of English-speaking patients who were
transferred (see Table 4). In the crude model, sepsis
patients from non-visible countries of birth were less
likely to go to intensive care (0.89 (0.83, 0.95)) as were
patients from sub-Saharan Africa (0.62 (0.42, 0.93; see Table 2)). In the fully adjusted model, male gender,
younger age, lack of co-morbidity, surgery during the
admission, end-organ dysfunction during the admission,
microbiological nature of sepsis, residence
in an area with high accessibility to goods and services
were all associated with higher odds of intensive care
use. Notably, the SEIFA economic index did not relate
to intensive care use. Patients in the visible ethnic
category, particularly from Asia and sub-Saharan
Africa, had lower odds of receiving intensive care.
Hospital mortality in sepsis
Eighteen percent of patients with sepsis died in hospital
(see Table 4). In the crude model, patients from
non-visible and visible countries of birth had higher
odds of hospital mortality. After adjustment, patients
from non-visible countries of birth had lower odds of
death in hospital, with patients from other ethnic
groups having a similar risk of death as those from
English-speaking countries. Other factors associated
with an increased risk of mortality included female
gender, age, requirement for intensive care, comorbidity,
end-organ dysfunction, patients in public hospitals, patients with Gram-positive and fungal
sepsis (in comparison to Gram-negative sepsis).
Table 2 :Models of access and outcome.
In summary, patients from Asia and sub-Saharan
Africa had lower odds of receiving intensive care in
comparison to those born in an English-speaking
country; however, this decreased access did not translate
to worse outcomes in these two groups.
The purpose of the above analysis has been to explore a
classification based on the use of a routinely available
variable in hospital discharge abstracts, country of birth,
to describe variation in access and outcomes in
healthcare delivered to ethnic groups in a universal
healthcare system. The classification was based on a
theoretically informed approach that distinguished
ethnically visible and invisible groups from the background
population of Australia.
The findings on access to cardiac care show no
associations. These results are in sharp contrast to US
studies that show clear disparities, with the greatest
burden falling on the more visible African American
and Hispanic populations (Weitzman et al, 1997;
Petersen et al, 2002; Gonzalez et al, 2003). However,
the existence in Australia of a universal, public, health
insurance scheme in the formof Medicare may indeed
demonstrate that, regardless of attitudes held by staff,
universal healthcare coverage may be the critical factor
in ensuring optimal outcomes, regardless of ethnicity.
In other words in the application of treatment and care
regimens in Australian hospital settings, the system is
colour blind with respect to clinically, although not
necessarily personally and emotionally, important
outcomes. This is not to say that discrimination based
on race and ethnicity does not occur, nor does it
diminish the importance of perceived discrimination.
It does, however open up an important line of inquiry
and the potential for cross-country comparisons in
the examination of experiences of discrimination and
the mitigation of this experience by universal access.
Some association is shown with post-partum haemorrhage,
which could suggest poorer management and
late identification of excessive bleeding (Bouvier-Colle
et al, 2001). The identified associations merely provide
a small but critical piece to a complex puzzle, the rest
of which could be provided by the other methods of
research.
In sepsis, patients from Asia and sub-Saharan Africa
had lower odds of receiving intensive care in comparison
to those born in an English-speaking country;
however, this decreased access did not translate to
worse outcomes in these two groups.
There are some clear limitations in the analysis,
which point to areas requiring further work. Due to the lack of a predefined variable on ethnicity, a surrogate
measure based on country of birth was developed.
The potential for misclassification is highest for two
groups: (1) individuals born in Australia to parents
born in countries within the visible and non-visible
groups; and (2) individuals within the visible ethnic
category who are from countries where English is
either the lingua franca or the medium of instruction.
There is a clear need for the development of
methods that identify and monitor discrimination in
the quality of care received by ethnic minorities
(Smedley et al, 2003; National Research Council,
2004). This will become increasingly important for
two main reasons. Current migration trends are from
poor countries with black majority populations
towards high-income countries that have traditionally
operated as mono-cultural. Secondly, economic policies
are generally moving away from the protections
given by the welfare state. The full implications of
these two trends will need to be demonstrated with a
systematic research agenda.
A complete theoretical and hypothesis-driven approach
to the investigation of ethnicity, discrimination
and health outcomes is needed to understand
how health systems and the culture of medical practice
can improve care for all ethnic groups. The assumption
is that health outcomes and quality of care rely on
the ability of health systems to be sensitive to the needs
of particular patients, while maintaining equitable
access regardless of culture and ethnicity. These assumptions
focus the specific research questions and
approach, which necessarily would require the use of a
multi-method protocol. A five-step protocol would
potentially consist of:
1 the identification of disparities in clinical outcomes: the analysis of clinical outcome/quality of care data
by ethnicity, categorised according to markers of
exclusion. The covariates in the analysis will need to
take into account the various clinical and contextual
associations with poorer health outcomes for
the given condition
2 a policy analysis of institutional and clinical procedures: while policies may not necessarily be
overtly discriminatory in intent, they may have the
effect of discriminating against particular groups
who as a result of particular characteristics are
unable to comply with set guidelines. Protocols
for policy analysis have been proposed for compliance
with human rights frameworks in health
(Hunt, 2004)
3 investigation of discriminatory practice: discrimination
in practice may be the result of an omission,
intentional or unconscious, that results in the
disadvantage to individuals or groups based on
particular characteristics. Tools for the analysis of
discrimination in practice have been implemented, for instance in the investigation of HIV-related
discrimination (UNAIDS, 2000)
4 staff attitudes: despite policy and practice guidelines,
negative attitudes of individual staff towards
ethnic minorities may be reflected in their practice.
While overt racism is not often documented, the
evolution to subtler but no less prejudicial attitudes
has been documented in service provision settings.
There is considerable political opposition to confronting
racial attitudes (Krieger, 2001; Smedley
et al, 2003; National Research Council, 2004).
Nonetheless, there is an urgent need for a measure
and ongoing monitoring of markers of social distance
(Bogardus, 1925) in general and racial attitudes
in particular
5 patient perceptions and experiences of discrimination: discrimination has been reported in a number of
studies. Without a more systematic comparative
case studies design into the experiences, it is difficult
to determine if experiences reflect a general
substandard quality of care, or if the perception of
discrimination is indeed a result of ethnic markers
(Manderson and Allotey, 2003a, 2003b).
The Agency for Healthcare Research and Quality in
the US suggests that the indicators for quality of care
likely to identify discrimination include effectiveness,
patient safety, timelines and patient centredness (Agency
for Healthcare Research and Quality, 2005). These,
however, require that the relevant data are systematically
collected. Existing data on ethnicity vary widely
in quality, mode of collection and definition. Data sets
in the UK, for instance, rely on self-definition or health
staff definition (Anonymous, 1996; McAuley et al, 1996;
McKenzie and Crowcroft, 1996; Karlsen and Nazroo,
2006),with ongoing debates about the relevance of the
categories. Australia relies on country of birth and the
US on broad categories based on origins. While there
is some merit to redesigning data collection systems to
address the definitional problems, some use can be
made of existing data by linking the operationalisation
of ethnicity to the central hypothesis of the research
question. Furthermore, multi-method studies that
explore both objective and subjective experiences
and outcomes of discrimination are critical to exploring
and addressing the effect on health and healthcare.
Our proposed multi-method protocol provides a
range of data to enable triangulation for the assessment
of discrimination.
Acknowledgment
The opinions expressed are those of the authors and
do not necessarily represent the views of the Victorian
Department of Human Services. The authors would
like to thank Associate Professor Helen McBurney and Dr Steven Bunker for the use of their cardiac rehabilitation
data.
CONFLICTS OF INTEREST
None.
References
- Acute Health Division (2000) The Victorian Admitted Episodes Dataset: an Overview April 2000. Melbourne: Acute Health Division, Victorian Government Department of Human Services.
- Adamson J, Ben-Shlomo Y, Chaturvedi N and Donovan J (2003) Ethnicity, socio-economic position and gender – do they affect reported health-care seeking behaviour? Social Science and Medicine 57:895–904.
- Agency for Healthcare Research and Quality (2005) 2004 National Healthcare Disparities Report. AHRQ Publication No 05–0014. Rockville, MD: US Department of Health and Human Services.
- Allotey P, Manderson L and Reidpath D (2002) Addressing cultural diversity in Australian health services. Health Promotion Journal of Australia 13:31–5.
- Anand S (1999) Using ethnicity as a classification variable in health research: perpetuating the myth of biological determinism, servicing socio-political agendas, or making valuable contributions to medical sciences. Ethnicity and Health 4:241–4.
- Anonymous (1999a) Editor’s choice: error and institutionalised racism. BMJ 318:612.
- Anonymous (1999b) Institutionalised racism in health care [editorial]. The Lancet 353:765.
- Anonymous (1996) Style matters: ethnicity, race, and culture: guidelines for research, audit, and publication. BMJ 312:1094.
- Australian Bureau of Statistics (2001) 2001 Census of Population and Housing. Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics (2003) Census of Population and Housing: socio-economic indices for areas, Australia 2001. Canberra: Australian Bureau of Statistics.
- Australian Institute of Health and Welfare (2004) Australia’s Health 2004. The ninth biennial report of the Australian Institute of Health and Welfare. Canberra: Australian Institute of Health and Welfare.
- Bach PB, Cramer LD, Warren JL and Begg CB (1999) Racial differences in the treatment of early-stage lung cancer. New England Journal of Medicine 341:1198–205.
- Barnes M and Weiner W (1999) Evidence of race based discrimination triggers new legal and ethical scrutiny. 8 BNA Health Law Reporter 8: 1984.
- Bhopal R (2004) Glossary of terms relating to ethnicity and race: for reflection and debate. Journal of Epidemiology and Community Health 58:441–5.
- Bogardus E (1925) Measuring social distances. Journal of Applied Sociology 1:216–26.
- Bouvier-Colle M, Ould EJD, Varnoux N et al (2001) Evaluation of the quality of care for severe obstetrical haemorrhage in three French regions. British Journal of Obstetrics and Gynaecology 108:898–903.
- Britton A, Shipley M, MarmotMand Hemingway H (2004) Does access to cardiac investigation and treatment contribute to social and ethnic differences in coronary heart 32 V Sundararajan, DD Reidpath and P Allotey disease? Whitehall II prospective cohort study. BMJ 329:318.
- Canto JG, Allison JJ, Kiefe CI et al (2000) Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. New England Journal of Medicine 342:1094–100.
- Commonwealth Department of Health and Aged Care (2001)Measuring Remoteness: Accessibility/Remoteness Index of Australia (ARIA), revised edition. Canberra: ACT, Commonwealth of Australia.
- Comstock R, Castillo E and Lindsay S (2004) Four year review of the use of race and ethnicity in epidemiologic and public health research. American Journal of Epidemiology 159:611–19.
- Doescher M, Saver B, Franks P and Fiscella K (2000) Racial and ethnic disparities in perceptions of physician style and trust. Archives of Family Medicine 9:1156–63.
- Gonzalez PC, Gauvreau K, Demone JA, Piercey GE and Jenkins KJ (2003) Regional racial and ethnic differences in mortality for congenital heart surgery in children may reflect unequal access to care. Pediatric Cardiology 24: 103–8.
- Hunt P (2004) The Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health. Report of the Special Rapporteur E/CN.4/2004/49. Geneva: United National General Assembly.
- Karlsen S and Nazroo JY (2006) Defining and measuring ethnicity and race: theoretical and conceptual issues for health and social care research. In: Nazroo JY (ed) Health and Social Research in Multiethnic Societies. London: Routledge, pp. 20–38.
- Krieger N (2001) The ostrich, the albatross, and public health: an ecosocial perspective–or why an explicit focus on health consequences of discrimination and deprivation is vital for good science and public health practice. Public Health Reports 116:419–23.
- LaVeist TA (ed) (2002) Race, Ethnicity and Health: a public health reader. San Francisco: John Wiley and Sons.
- Manderson L and Allotey P (2003a) Cultural politics and clinical competence in Australian health services. Anthropology in Medicine 10:71–85.
- Manderson L and Allotey P (2003b) Story telling, marginality and community in Australia: how immigrants position their difference in health care settings. Medical Anthropology 22:1–22.
- McAuley J, de Souza L, Sharma V et al (1996) Describing race, ethnicity, and culture in medical research. Self defined ethnicity is unhelpful. BMJ 313:425–6.
- McKenzie K and Crowcroft NS (1996) Describing race, ethnicity, and culture in medical research. BMJ 312:1054.
- National Centre for Classification in Health (1998) The International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Australian Modification, ICD-10-AM Australian Coding Standards First Edition 1 July 1998.
- National Centre for Classification in Health. Sydney: Faculty of Health Sciences, University of Sydney.
- National Centre for Classification in Health (2000) The International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Australian Modification (ICD-10-AM), Volume 5 ICD-10-AM Australian Coding Standards Second Edition 1 July 2000. National Centre for Classification in Health. Sydney: Faculty of Health Sciences, University of Sydney.
- National Research Council (2004) Measuring Racial Discrimination. Washington DC: National Academies Press.
- Petersen LA, Wright SM, Peterson ED and Daley J (2002) Impact of race on cardiac care and outcomes in veterans with acute myocardial infarction. Medical Care 40:I86–96.
- Physicians for Human Rights (2003) Identifying disparities and discrimination and developing plans to address them. In: Physicians for Human Rights (ed) The Right to Equal Treatment. Washington DC: Physicians for Human Rights, pp. 25–30.
- Reidpath D, Chen K, Giffird S and Allotey P (2005) ‘He hath the French pox’: stigma, social value, and social exclusion. Sociology of Health and Illness 27:468–89.
- SAS Institute Inc (1999) SAS. 8.2 ed. Cary, North Carolina: SAS Institute Inc. Smedley BD, Stith AY and Nelson AR (eds) (2003) Unequal Treatment: confronting racial and ethnic disparities in health care. Washington DC: National Academies Press.
- Sundararajan V, Henderson T, Perry C et al (2004) New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. Journal of Clinical Epidemiology 57:1288–94.
- UNAIDS (2000) Protocol for the Identification of Discrimination against People Living with HIV – UNAIDS Best Practice Collection. Geneva: UNAIDS.
- Weitzman S, Cooper L and Chambless L (1997) Gender, racial and geographical distances in the performance of cardiac diagnostic and therapeutic processes for hospitalized acute myocardial infarction in four states. American Journal of Cardiology 79:722–6.