Introduction
The first release from the Office for National Statistics
(ONS) on 16 July 2012 of the 2011UKcensus indicates
that in the first decade of the twenty-first century the
population of England and Wales has risen by 3.7
million (from just over 50 million, an increase of
about 7%), and over 50% of this increase consists of
migrants. In general, the term ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âmigrantÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ is associated
with recent arrivals in a foreign country. In the UK,
migrants who have been in the country for a while,
including their descendants, are described as belonging
to ethnic minorities. The trajectory for the future
suggests that, in 20 yearsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ time, the total population of
England and Wales will have risen to 70 million. It is
expected that migrants will account for two-thirds of
this increase. In theUKas a whole, approximately 15%
of the total population will be of migrant origin,
equivalent to about one in six or possibly more. This
is considerably higher than the current figure (about
4%) or any projected figures for the European Union
(EU).
Resources
• Release: 2011 Census, Population and Household
Estimates for England and Wales. www.ons.gov. uk/
ons/guide-method/census/2011/index.html
• United Nations Department of Social Affairs
(2009) United Nations: trends in international migrant
stock. The 2008 revisions. United Nations
database, PDP/DB/MIG/Stock/Rev.2008. New York:
United Nations Department of Social Affairs,
Population Division.
• WHO Regional Office for Europe (1998) The
Tallinn Charter Health System for Health and
Wealth. Copenhagen: WHO Regional Office for
Europe.
Access to healthcare
In the UK there is extensive legislation that imposes a
duty on the NHS to provide all reasonable healthcare
requirements for all of its users. Equality legislation
prohibits direct or indirect discrimination of any kind
on the basis of race, which is defined as a protected
characteristic. Although the right to health is enshrined
in many legal instruments, there are a number of
obstacles to migrant/ethnic minority populations receiving
appropriate healthcare. These include linguistic
barriers, lack of familiarity with the health system,
and cultural or other barriers that may impede access
to services.
Resources
• National Health Service Act 2006
• Equality Act 2010
• Johnson MRD (2003) Ethnic diversity in social
context. In: Kai J (ed.) Ethnicity, Health and Primary
Care. Oxford: Oxford University Press. pp. 3ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â
13.
• Gill P, Kai J, Bhopal RS et al (2002) Black and
minority ethnic groups. In: Stevens A, Raftery J,
Mant J et al (eds) Healthcare Needs Assessment:
epidemiologically based needs assessment reviews,
3rd series. Oxford: Radcliffe Medical Press.
Disease variations and outcomes
Long-term conditions are associated with higher
mortality. Clinical variations in the epidemiology of
conditions such as rheumatoid arthritis and systemic
lupus erythematosus (SLE) have been described in
British South Asians. These patients with SLE have been noted to have much more aggressive disease and
higher mortality rates than their white counterparts.
Resources
• Samanta A, Samanta J, Johnson MRD et al (2005)
Rheumatoid arthritis in minority ethnic groups:
patterns of disease, clinical and sociocultural features
among British South Asians. Diversity in
Health and Social Care 2:99ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â118.
• Samanta A, Feehally J, Roy S et al (1991) High
prevalence of systemic disease and mortality in
Asian subjects with systemic lupus erythematosus.
Annals of the Rheumatic Diseases 50:490ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â2.
• Samanta A, Roy S, Feehally J et al (1992) The prevalence
of diagnosed systemic lupus erythematosus in
whites and Indian Asian immigrants in Leicester
City, UK. British Journal of Rheumatology 31:679ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â
82.
Rheumatoid arthritis
National guidelines champion the principle of early
diagnosis and treatment of rheumatoid arthritis
with specific disease-modifying anti-rheumatic drugs
(DMARDs), ideally within 3 months of the onset of
symptoms. A multicentre audit of rheumatoid arthritis
in minority ethnic groups showed that a high proportion
(62%) exceed the 3-month time interval for
specialist referral, and there is a delay in the initiation
of DMARD therapy of more than 3 months, more
than 6 months and more than 9 months in 8%,1%and
10%, respectively, of South Asian patients.
A significant delay in the time taken for presentation
of South Asian patients with rheumatoid arthritis
to primary care physicians has been reported
from Birmingham. The median time taken for presentation
to primary care was 24 weeks after the onset
of symptoms for South Asians, compared with 12
weeks for non-South Asian patients. A number of
causal and attitudinal factors were identified which
resulted in patients from minority ethnic groups
deploying non-medical self-management strategies
instead of seeking medical advice.
Addressing the needs of black and ethnic minority
groups can be complex, as these communities have a
diverse set of social beliefs, values, languages and
cultural attitudes. There is a generalised belief that
arthritis is completely dependent upon factors such as
ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âgoodÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ and ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âbadÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ foods, or that it is a result of divine
intervention. Rheumatoid arthritis may incur stigma,
and there is a tendency for minority groups to prefer
alternative therapies such as homeopathy, prayer and
meditation. In a retrospective study of ethnic differences in response to DMARDs among patients with inflammatory
arthritis, people of SouthAsian ethnicity stopped
therapy sooner than North Europeans. Possible explanations
for this included problems with effective
communication, cultural differences in expectations
and response to illness. Recent studies have shown
increased pain and disability in South Asian patients
with rheumatoid arthritis compared with their Northern
European counterparts.
Resources
• National Institute for Health and Clinical Excellence
(2009) Rheumatoid Arthritis: the management
of rheumatoid arthritis in adults. NICE Clinical
Guideline CG79. London: National Institute for
Health and Clinical Excellence.
• Panchal S, Moorthy A, Hayat S et al (2012) A
national audit of patients with rheumatoid arthritis
of black and minority ethnic origin. Annals of
Rheumatic Disease 71(Suppl. 3):465.
• Kumar K, Gordon C, Toescu V et al (2008) Beliefs
about medicines in patients with RA and SLE: a
comparison between patients of South Asian and
White British origin. Rheumatology 47:690ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
• Adebajo AO, Blenkinron L and Dieppe P (2004)
Patient education for diverse populations. Rheumatology
43:1321ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â3.
• Samanta A, Shaffu S, Panchal S et al (2012)
Tinkering at the edges or collaborative symbiosis?
Ethnicity and rheumatology: a consensual review
discussion. Diversity and Equality in Health and
Care 9:000ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â000.
• Kett C, Flint J, Openshaw M et al (2010) Selfmanagement
strategies used during flares of rheumatoid
arthritis in an ethnically diverse population.
Musculoskeletal Care 8:204ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â14.
• Odutola J and WardMM(2005) Ethnic and socioeconomic
disparities in health among patients with
rheumatic disease. Current Opinion in Rheumatology
17:147ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â52.
• Helliwell PS and Ibrahim G (2003) Ethnic differences
in response to disease-modifying drugs.
Rheumatology 42:1197ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â201.
• Ghelani A, Mastana S and Samanta A (2011)
Rheumatoid Arthritis among South Asian and
Caucasian Populations of the East Midlands in the
UK: a genetic and bio-demographic analysis.
SaarbruÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâècken, Germany. VDM Verlag Dr. Muller.
• Griffiths B, Situnayake RD, Clark B et al (2000)
Racial origin and its effect on disease progression
and HLA-DRB1 types in patients with rheumatoid
arthritis: a cross-sectional study. Rheumatology 39:
857ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â64.
Psoriatic arthritis
There is a paucity of data on the effects of ethnicity on
psoriatic arthritis. Data from Asia show a prevalence
of 10ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â100 per 100 000 members of the population in
China, and 0.1ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â1 per 100 000 in Japan. In Singapore,
psoriatic arthropathy is more common in the Indian
population than among the Chinese population, and
therefore Indian ethnicity is acknowledged as a risk
factor for arthritis. However, a recent observational
study noted that there is a significant difference in
disease perception (tender joint count) and pain and
health assessment scores among Gujarati patients with
psoriatic arthritis compared with their Caucasian
counterparts.
Resources
• Tam LS, Leung YY and Li EK (2009) Psoriatic
arthritis in Asia. Rheumatology 48:1473ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
• Thumboo J, Tham SN, Tay YK et al (1997) Patterns
of psoriatic arthritis in Orientals. Journal of Rheumatology
24:1949ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
• Malipeddi A and Hassan W (2011) Do Gujarati
Indian Patients Have More Severe Psoriatic Arthritis
Than Caucasian Patients? An outpatient-based study.
ZuÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâèrich: EULAR Congress Abstract Book, European
League Against Rheumatism.
Osteoporosis
Bone mineral density (BMD) has been found to be
lower in the South Asian (Gujarati) population than in
the local white population in Leicestershire. A significant
trend towards vitamin D deficiency in South
Asians appears to be the main causative factor, especially
in view of the fact that vitamin D levels have
been found to have a positive effect on bone mineral
density. There is little information available about
osteoporosis or osteomalacia for minority ethnic
groups. The information on ostemoalacia that is
available is of limited benefit, as its cultural competence
is open to question.
Resources
• Hamson C, Goh L, Sheldon P et al (2003) Comparative
study of bone mineral density, calcium
and vitamin D status in the Gujarati and white
populations of Leicester. Postgraduate Medical
Journal 79:279ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â83.
• Roy D, Berry JL, Pye SR et al (2007) Vitamin D
status and bone mass in UK South Asian women.
Bone 40:200ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â4.
• Samanta A, Johnson MRD, Guo F et al (2009)
Snails in bottles and language cuckoos: an evaluation
of patient information resources for South
Asians with osteomalacia. Rheumatology 48:299ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â
303.
• Johnson MRD, Samanta A, Hudson N et al (2006)
Evaluation of Patient Information Resource on Osteomalacia
in Asian Languages. Seacole Research
Paper 5. Leicester: Mary Seacole Research Centre,
DeMontfort University.
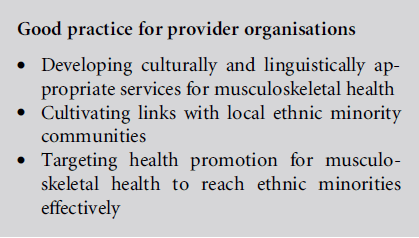
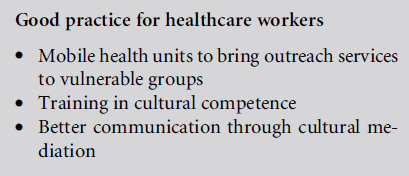
Census and consensus
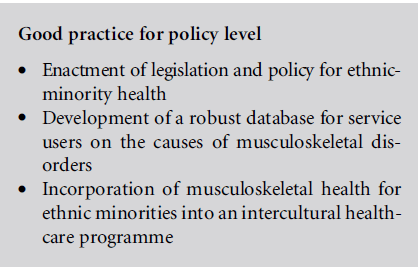
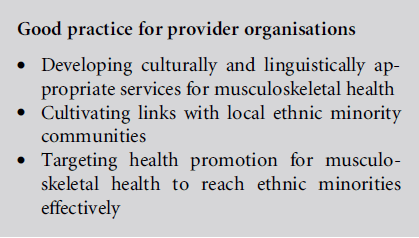
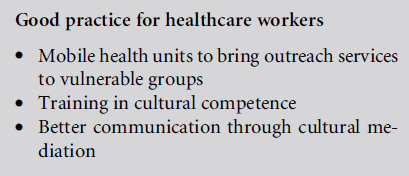
To date, the focus on musculoskeletal health in minority
ethnic groups in the UK has been lamentably
limited. The recent 2011 UK census indicates a rapidly
growing trend towards the UK becoming an even
more pluralistic multi-ethnic society. If musculoskeletal
health is to be truly meaningful for minority
ethnic groups, a consensus on good practice is
required. Good practice needs to seamlessly extend
across the levels of policy, provider organisations and
healthcare workers in order to integrate strategy and
implementation that is culturally competent for ethnic
minority groups.
Resources
• Rachel B, Mladovsky P, Deville W et al (2011)
Migration and Health in the European Union.
Maidenhead: Open University Press.
• Mladovsky P, Ingleby D, McKee M et al (2012)
Good practices in migrant health: the European
experience. Clinical Medicine 12:248ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â52.
• Samanta A, Shaffu S, Panchal S et al (2012)
Tinkering at the edges or collaborative symbiosis?
Ethnicity and rheumatology: a consensual review
discussion. Diversity and Equality in Health and
Care 9:000ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â000.
Summary
• There is a growing ethnic minority population in
the UK, of which South Asians currently represent
the largest group. There is a paucity of data on
musculoskeletal health in this group.
• Members of ethnic minority groups with rheumatoid
arthritis tend to access the healthcare system at
a late stage, and are more inclined to discontinue
their medication for rheumatoid arthritis.
• There are a number of non-medical cultural beliefs
about the causes of arthritis, and alternative approaches
to therapy are preferred to conventional
medicine.
• There is a paucity of culturally competent educational
material related to musculoskeletal conditions.
• Observational studies have shown clinical variations
in rheumatoid arthritis, systemic lupus erythematosus
and psoriatic arthritis in ethnic minorities. There is a
need to understand and address social beliefs, language
and culture in order to achieve optimal healthcare.
• Coordinated good practice at the level of policy
makers, provider organisations and healthcare
workers is required to ensure that ethnic minority
groups have access to healthcare services that are
responsive to their needs.