Keywords
Patellofemoral pain syndrome; Chondromalacia; Pain; PRP therapy; Ozone therapy; Quality of life
Introduction
Chondromalacia patellae is defined as a cartilaginous softening and fibrillation of patellar bone cartilage, which constitutes pathologic changes of articular cartilage, and it is one of several causes of Patellofemoral Pain Syndrome (PFPS) [1,2]. Sometimes, Chondromalacia is a word used to define PFPS [2]. PFPS is a common overuse disorder that involves the patellofemoral region, and it is referred as knee pain and accounts for 10 to 25% of all visits seen in physical therapy clinics [1]. PFPS is the most common cause of complaint seen by general practitioners, traumatology, rheumatology, rehabilitation and sports medicine specialists [3,4].
PFPS produces pain in the patella and retinaculum once intra articular and per articular pathology is discarded [5]. In that context, clinical diagnosis is demanding, because consensus about the pathophysiology is unclear and the treatment remains a difficult task. Then, PFPS is the sum of complex symptoms and mainly a diagnosis of exclusion; while Chondromalacia patellae, is a pathologic diagnosis [6]. Moreover, some authors consider Chondromalacia as a pre-stage of Osteoarthritis (OA) [6]. PFPS is very common in active individuals in up to 25 to 40% with knee pain; although, the true incidence is unspecified [7]. Although multifactorial, PFPS is the result of intrinsic and extrinsic factors. Some causative factors include overuse, malalignment and trauma [8]. Abnormal tissue homeostasis represented by inflamed synovial lining and fat pad tissues, retinacular neuromas, increased intraosseous pressure and increased osseous metabolic activity of the patella, are all related to pain and dysfunction [9]. From those observations; it is expected that inflammation plays a major role in Chondromalacia/PFPS pathogenesis.
To diagnose PFPS, a good clinical history, a thorough examination and the exclusion of alternative pathologies are needed [10]. No pathognomonic sign or symptom is been described on PFPS; however, the sum of pain with resisted quadriceps contraction and pain while squatting are the signs with more diagnostic validity [11]. For initial management, plain radiographies are unnecessary. They are useful to rule out some other sources of anterior knee pain, as bipartite patellae, knee arthrosis, loose osteophytes and unobserved fractures [12]. In PFPS, the goals of treatment are to ameliorate pain on the acute phase; and to enhance alignment and patellofemoral tracking; and to return the patient to as optimal a level of function as feasible, on the recovery phase. Physical therapy is aimed on enhancing strength and flexibility on lower extremities and core muscles, including hip adductors and quadriceps [13-17]. NSAIDs (non-steroidal anti-inflammatory drugs) are useful just for short term relief (2 to 3 weeks) [18]. Regarding physical therapies, ice applied to the anterior knee ameliorates pain associated to PFPS. There is no medicine-based evidence to support the use of ultrasound, iontophoresis, phonophoresis or electrical stimulation on PFPS treatment [18-21]. Surgical interventions for PFPS are the last option; recommended after all previous therapies have failed. It is a last resort treatment; then conservative therapy should be performed for 6 to 12 months prior to considering surgical modalities [4].
Since Chondromalacia and PFPS constitute a kind of articular cartilage pathology, and articular cartilage has poor inherent healing capacity, its treatment remains a challenge [22]. Recent advances in Regenerative Medicine postulate Platelet Rich Plasma (PRP) as a promising treatment option. Autologous PRP releases cytokines and Growth Factors that activate the healing of bone and soft tissues, as in the case of Chondromalacia [22]. In fact, Kon et al. [23] have stated promising outcomes from intra articular PRP in early degenerative cartilage lesions, a common feature of Chondromalacia. On the other hand, Fernández-Cuadros [24,25] stated that inflammation, a common feature of Chondromalacia, pain and poor function could be reverted by Ozone treatment, if infiltrated intra articularly. Therefore, despite the paucity of studies on Ozone treatment, and the growing studies on PRP treatments, to the best of our knowledge, there is no report that compares PRP to Ozone infiltrations in the management of PFPS and Chondromalacia.
The aim of this study is to evaluate the efficiency of PRP compared to Ozone infiltrations in the treatment of PFPS and Chondromalacia, since both treatments could be considered to be valid conservative options in the management of such entities.
Material and Methods
Trial design
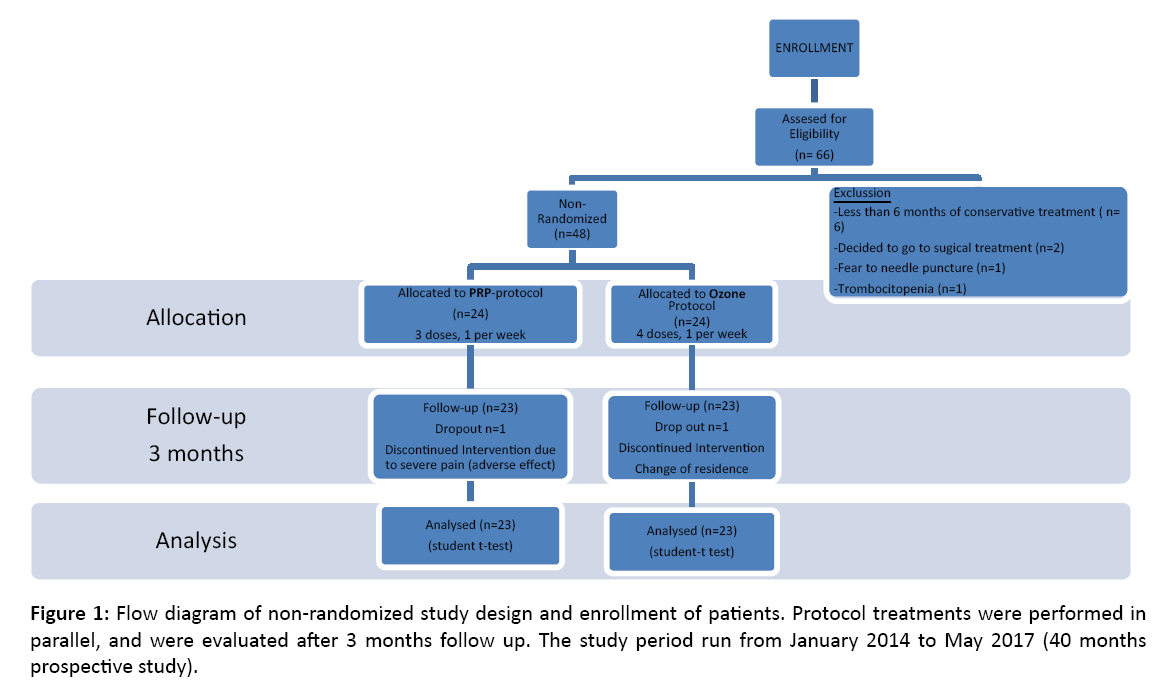
This was a prospective non-randomized controlled trial, which compared two treatment protocols in a parallel design, conducted in a tertiary outpatient Rehabilitation Department at Santa Cristina University Hospital. Measurements were performed at baseline and at 3 months follow-up period, after protocol treatments were finished (Figure 1). The study was conducted in accordance with the Declaration of Helsinki principles [26].
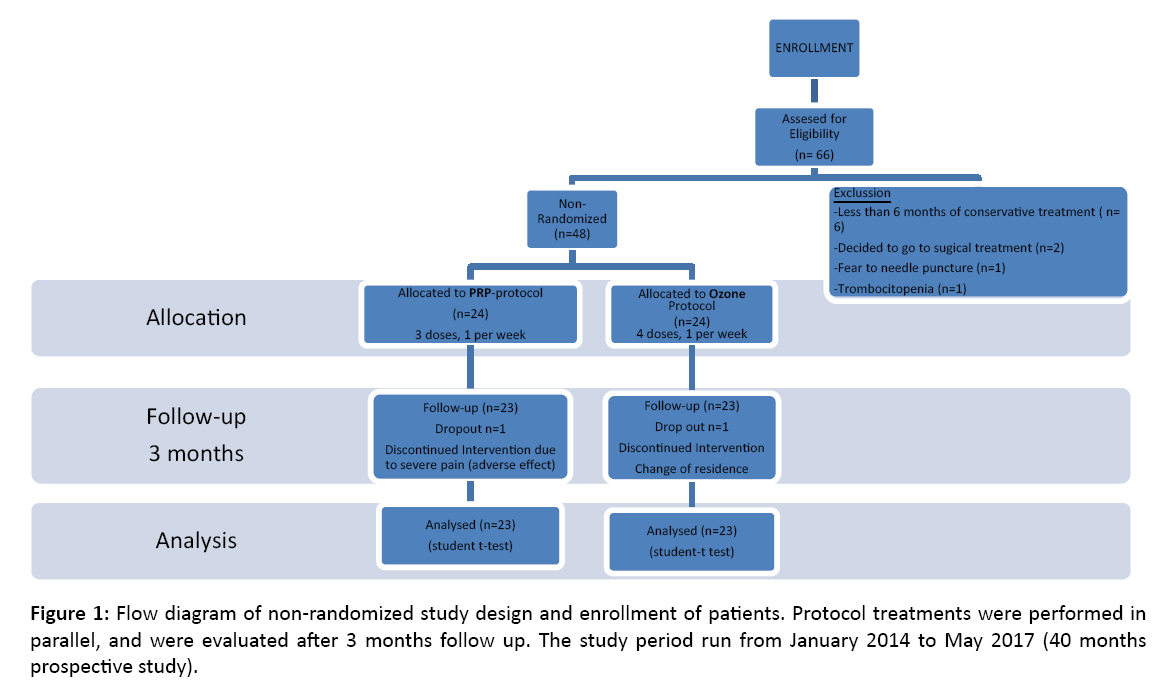
Figure 1: Flow diagram of non-randomized study design and enrollment of patients. Protocol treatments were performed in parallel, and were evaluated after 3 months follow up. The study period run from January 2014 to May 2017 (40 months prospective study).
Participants
Patients were recruited from January 2014 to May 2017, through regular referral by general health practitioners, rheumatologist, rehabilitation physicians and orthopedic surgeons. Eligibility for inclusion on the study was the compliment of inclusion and/or exclusion criteria and at least 6 months of conservative treatment without success.
Inclusion criteria
a) Patients with PFPS/Chondromalacia diagnosed by MRI, grade 2 or more.
b) With pain superior to 3 on Visual Analogical Scale (VAS).
c) Older than 18 years of age.
d) Who failed any other non-surgical treatment (analgesic, non-steroidal anti-inflammatory drugs, steroidal/ hyaluronic acid injections, visco-supplementation and/ or physical medicine.
e) Unwilling or not candidate for surgical treatment (drilling/mosaicoplasty or autologous chondrocyte transplantation).
Exclusion criteria
a) Any severe coagulopathy and/or thrombocytopenia.
b) Cardiovascular instability or any other severe disease.
c) In the case of Ozone treatment: deficit of glucose-6- phosphate dehydrogenase, pregnancy, hyperthyroidism, treatment on angiotensin converting enzyme inhibitors, or allergy to Ozone.
d) Absence of written informed consent.
e) Patients who by any reason failed to compliment any of the scores applied (VAS and or Western Ontario and Mc Master Index for Osteoarthritis (WOMAC)).
f) Patients who failed to finish the whole protocol (3 doses in case of PRP, 4 doses in case of Ozone therapy).
Baseline evaluation and treatment allocation
At baseline, demographic data such as age, comorbidities, occupation and other were recorded. Complete information of the existing treatment protocols with indication and adverse effects were explained. Informed consent was signed and VAS and WOMAC scores were filled prior to treatment. Patients were not-randomly assigned to PRP and/or Ozone (by physician/patient convenience), and parallel groups were followed comparing both treatment protocols at baseline and at 3 months follow-up.
PRP protocol
The proposed PRP-protocol consisted of an intra-articular infiltration of 3 ml of autologous blood, composed mainly on platelet-rich plasma, and a total of 3-sessions (1 session/week). To obtain the PRP, Accelerate Concentration System Device® from EXACTECH, EmCyte Anticoagulant Sodium Citrate Solution USP and Drucker Centrifuge (Series Performance) were used. Blood draw, blood processing and blood infiltration were main steps in PRP preparation.
The Accelerate II Platelet concentrating System PRP-S 30 ml® is a concentrating System manufactured by EmCyte Corporation and distributed by EXACTECH Inc. This kit permits the rapid preparation of platelet-rich plasma from 30 ml of the patient’s whole blood drawn at the time of treatment. This device is for one single use only, not to mention that standard aseptic techniques must be kept during the whole procedure.
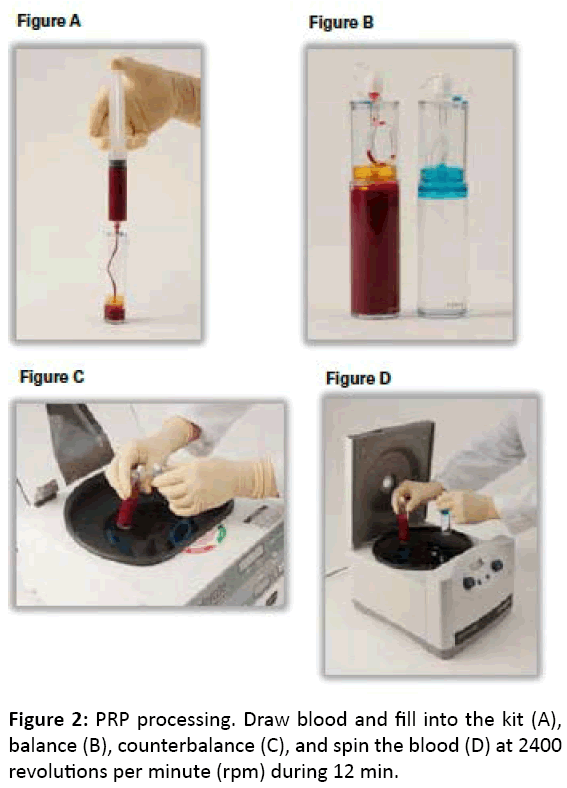
For whole blood draw procedure: draw 3ml of Anticoagulant Sodium Citrate Solution USP into the 30 ml syringe. Attach a syringe to the apheresis needle and prime the needle with the anticoagulant. Slowly draw 27 ml of blood from the patient (by venipuncture) filling the syringe to 30 ml. Smoothly and thoroughly mix the blood and anticoagulant upon collection to prevent coagulation (Figure 2).
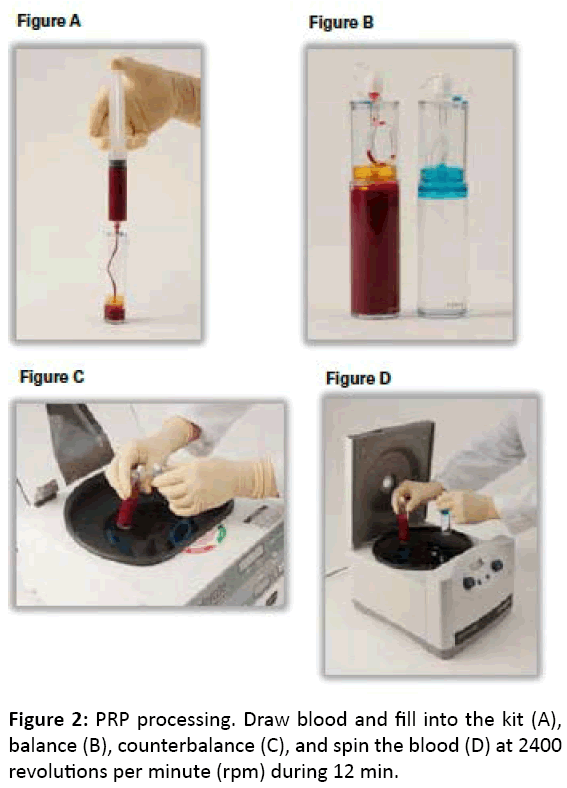
Figure 2: PRP processing. Draw blood and fill into the kit (A), balance (B), counterbalance (C), and spin the blood (D) at 2400 revolutions per minute (rpm) during 12 min.
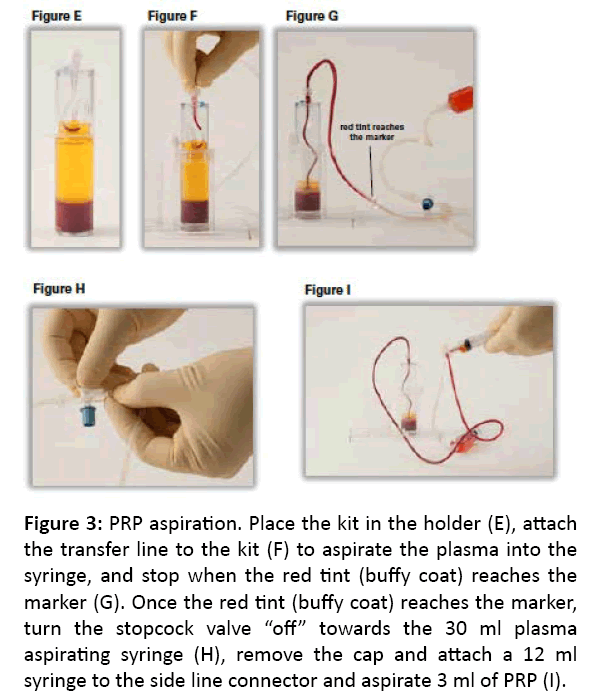
For blood processing, load, balance, spin and PRP-extraction maneuvers must be performed. To load, using the concentrating device, unscrew the cup and slowly add the 30 ml of anticoagulated whole blood into the concentrating kit. Screw the cap onto the device and load into the Drucker Centrifuge (Series Performance). To balance, counterbalance the concentrating kit. Place the counterbalance and Concentrating Device directly opposite to each other in the centrifuge rotor and make sure they contain the same volume. To spin, close the centrifuge lid. Set RPM (revolutions per minute) to 2400 and the time to 12 min Press the start bottom. Once the centrifuge processing is complete, open centrifuge, remove the Concentrating Device. To extract PRP, unscrew the cap from the Port (Figure 2). Using the aspirating accessory, aspirate the plasma into the 30 ml syringe until the disc touches the red cell interface, trapping the platelet buffy coat. Open the stopcock to the 12 ml syringe and aspirate 3 ml of PRP. Dilute the PRP with plasma to adjust the platelet concentrations. Remove sterile syringe and apply sterile cap (Figure 3).
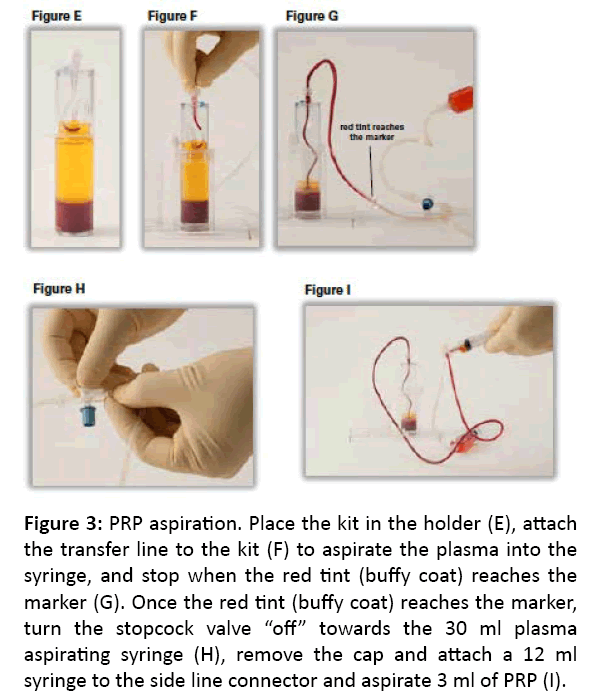
Figure 3: PRP aspiration. Place the kit in the holder (E), attach the transfer line to the kit (F) to aspirate the plasma into the syringe, and stop when the red tint (buffy coat) reaches the marker (G). Once the red tint (buffy coat) reaches the marker, turn the stopcock valve “off” towards the 30 ml plasma aspirating syringe (H), remove the cap and attach a 12 ml syringe to the side line connector and aspirate 3 ml of PRP (I).
For blood infiltration, 3 ml of PRP obtained from previous processing was injected into the lateral aspect of the knee joint. To infiltrate the knee joint, the patient lies on supine position, with mild flexion of the knee and slight external displacement of the patella to expose the articular joint space. To clean the skin, 1% antiseptic chlorhexidine solution was used previous to infiltration.
Ozone protocol
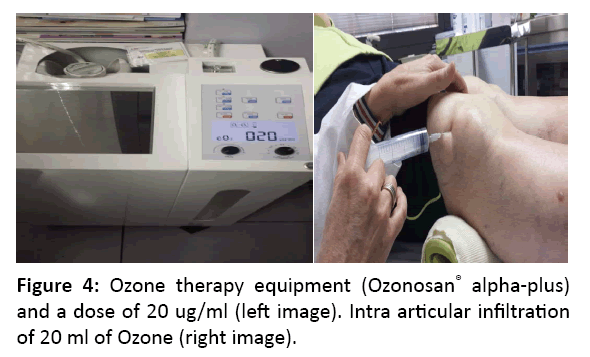
The Ozone protocol consisted of 4 sessions (1 session/week) of a medical mixture of Oxygen-Ozone (95%-5%) at a 20 μg/ml concentration was infiltrated intra-articularly. Ozonosan α-Plus® was the Medical Ozone generator device used. To deliver Ozone into the joint, a 27G, 4 cm Quincke needle was used. The skin was previously cleaned with 1% Chlorhexidine, and the area was anesthetized using a cold spray solution of ethyl chloride (100 g) dispensed as needed. Ozone was slowly infiltrated on the lateral aspect of the knee next to the patella, with the knee semi-flexed and mild patella subluxation, in order to expose the articular joint space. After infiltration, the knee was flexed and extended several times with the intention to distribute the Oxygen-Ozone mixture all over the articulation and the lateral recesses, and to confirm that the infiltration was delivered into the articulation, by listening a crepitus noise (Pérez-Moro Maneuver) (Figure 4). If erythema and excessive pain showed up during the infiltration, those signs indicated that infiltration was performed in periarticular manner; however, this discomfort usually disappears afterwards, in 10-15 min.
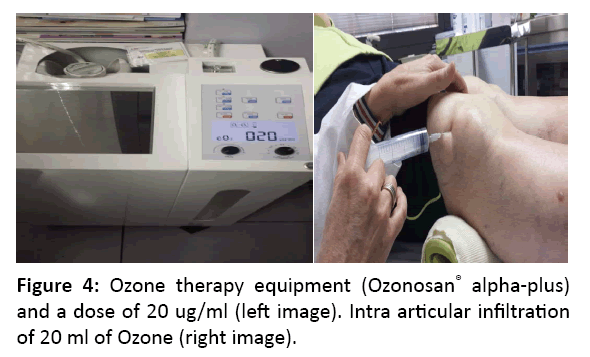
Figure 4: Ozone therapy equipment (Ozonosan® alpha-plus) and a dose of 20 ug/ml (left image). Intra articular infiltration of 20 ml of Ozone (right image).
Outcome measures
The symptoms severity represented by pain, function, stiffness and quality of life were rated by the VAS and WOMAC scores. VAS is a pain scale of Likert type graded from 0 to 10, where greater the value greater the pain. The WOMAC Index contains 24 questions in a total of three sub-scales; those are pain, stiffness and function [27-29]. Each sub-scale has five response options (none, mild, moderate, severe and extreme), and subtotal scores for pain (five Items), stiffness (two Items) and function (17 Items) range from 0-20, 0-8 and 0-68, respectively [27-30].
Chondromalacia was classified by Outerbridge in the following grades: Grade 0, no Chondromalacia features; Grade 1, softening and edema of cartilage; Grade 2, fibrillation and fissure lower than 1 cm; Grade 3, fibrillation and fissure between 1-2 cm; and Grade 4, fibrillation greater than 2 cm and subchondral bone exposure [31,32].
A difference greater than 6% of the maximum scores of the WOMAC Index is considered as clinically important. For the WOMAC scores: pain=1.2 points; stiffness=0.5 points; function=4.1 points [33].
Sample size and statistical analysis
The a priori power calculation was based on the WOMAC physical function subscale, with an expected effect size of 0.4 between both groups of treatment at 8 weeks follow-up (and on WOMAC pain subscale effect size of 0.2), 2 timepoint of measurement (pretest-posttest evaluation), expected autocorrelation between the repetitions of 0.5, a level of significance of 0.05 and a desired power of 0.80. Given these parameters a total size of 48 patients was needed, allowing for a dropout rate of 20% during the study, we aimed to include 58 patients (29 patients in each group). However, due to a low dropout rate of only 4% during the study, the sample size was adjusted to the previous calculated size, that is 48 patients, 24 patients in each group (Figure 1) [34].
The statistical analysis was achieved using SPSS (version 20.0), with α-error of 0.05 (95% confidence interval) and a desired power of 80% (β-error of 0.2). Initially, the Wilcoxon Test was carried out to assess normality between groups. In the descriptive analysis, mean and standard deviation for quantitative variables, and frequencies and percentages for qualitative variables, were performed. Considering the normal distribution and homogeneity of variances, the Student T-Test (for different treatment protocols) and the paired T-test (for similar treatment protocols) were used to evaluate quantitative variables. For qualitative variables, if needed, x2 test was used to compare both treatment groups.
Results
A total of 48 patients were evaluated in the study (24 allocated in each group) (Figure 1).
At baseline, age, sex, ratio male to female, clinical chondromalacia grades and symptom severity such as pain, stiffness and function were similar between groups of treatment (Table 1). Then, comparison between groups is suitable.
| Demographic |
PRP |
Ozone |
| Age, years |
40.37 ± 9.54 |
45.87 ± 9.88 |
| Female, n (%) |
9 (37.5%) |
15 (62.5%) |
| Male, n (%) |
15 (62.5%) |
9 (37.5%) |
| Ratio female:male |
0.6:1 |
1:0.6 |
| Clinical |
|
|
| Chondromalacia 2º (n, %) |
11 (41.8%) |
12 (50.0%) |
| Chondromalacia 3º (n, %) |
9 (37.6%) |
8 (33.4%) |
| Chondromalacia 4º (n, %) |
4 (16.6%) |
4 (16.6%) |
| Outcome variables |
|
|
| VAS pain (0-10) mean ± SD |
7.87 ± 1,03 |
7.25 ± 1.62 |
| WOMAC pain subscale (0-20) mean ± SD |
15.2 ± 2.8 |
14.7 ± 2.86 |
| WOMAC stiffness subscale (0-8) mean ± SD |
1.95 ± 2.47 |
2.16 ± 2.20 |
| WOMAC pain subscale (0-68) mean ± SD |
39.75 ± 16.18 |
41.0 ± 17.12 |
WOMAC: Western Ontario and Mc Master Universities Index for Osteoarthritis; VAS: Visual Analogical Scale
Table 1: Baseline characteristics of patients enrolled on the study.
In both groups, the most common grade of chondromalacia was 2º grade (41.8% in PRP, 50% in Ozone), followed by 3º (37.6% in PRP, 33.4% in Ozone) and 4º (16.6% in both PRP and Ozone) (Table 1).
When we analyze both treatment protocols separately, both PRP and Ozone were capable to produce pain relief (measured by VAS and WOMAC pain subscale) and improvement in function and rigidity (measured by WOMAC subscales), with a significant statistical level (p<0.05) (Table 2).
| Variable |
PRP before |
PRP after |
P |
O3 before |
O3 after |
P |
| PAIN (0-10) |
7.87 ± 1.03 |
3.04 ± 1.6 |
0.0000 |
7.25 ± 1.62 |
1.58 ± 1.5 |
0.0000 |
| WOMAC PAIN (0-20) |
15.12 ± 2.8 |
5.95 ± 3.2 |
0.0000 |
14.7 ± 2.86 |
3.0 ± 2.93 |
0.0000 |
| WOMAC RIGIDITY(0-8) |
1.95 ± 2.47 |
0.5 ± 0.88 |
0.0009 |
2.16 ± 2.2 |
0.25 ± 0.6 |
0.0001 |
| WOMAC FUNCTION (0-68) |
39.75 ± 16.18 |
16.37 ± 11.42 |
0.0000 |
41.0 ± 17.12 |
13.41 ± 8.55 |
0.0000 |
P=one-sample T-test analysis
WOMAC: Western Ontario and Mc Master Universities Index for Osteoarthritis
Table 2: Effectiveness of PRP and Ozone (O3) on Chondromalacia in a before-and-after individualized analysis (one-sample T-test analysis).
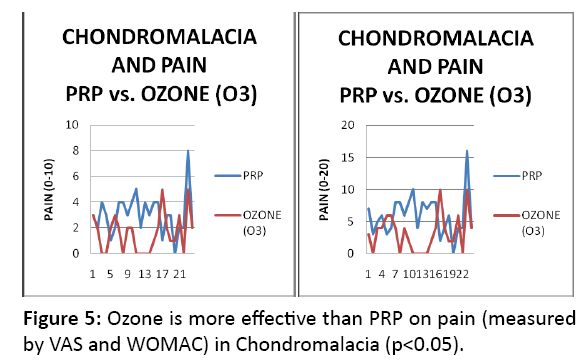
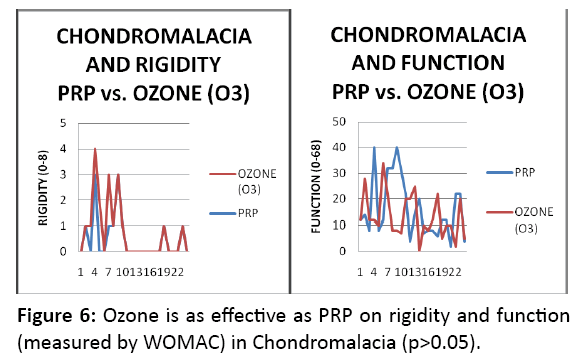
Moreover, if we compare clinical outcomes between treatment groups, Ozone produces even greater pain relief with respect to PRP (1.46 points on VAS scale and 2.95 points on WOMAC pain subscale) (p<0.05). On the contrary, both treatment protocols produce improvements in stiffness and function, but, without statistical significant difference (p<0.05) (Table 3 and Figures 5 and 6).
| Variable |
PRP before |
O3 before |
P |
PRP after |
O3 after |
P |
| PAIN (0-10) |
7.87 ± 1.03 |
7.25 ± 1.62 |
0.1183 |
3.04 ± 1.6 |
1.58 ± 1.5 |
0.0021 |
| WOMAC PAIN (0-20) |
15.12 ± 2.8 |
14.7 ± 2.86 |
0.6130 |
5.95 ± 3.2 |
3.0 ± 2.93 |
0.0033 |
| WOMAC RIGIDITY (0-8) |
1.95 ± 2.47 |
2.16 ± 2.2 |
0.7594 |
0.5 ± 0.88 |
0.25 ± 0.6 |
0.2598 |
| WOMAC FUNCTION (0-68) |
39.75 ± 16.18 |
41.0 ± 17.12 |
0.7961 |
16.37 ± 11.42 |
13.41 ± 8.55 |
0.3151 |
P=paired T-test analysis
WOMAC: Western Ontario and Mc Master Universities Index for Osteoarthritis
Table 3: Effectiveness of PRP compared to Ozone (O3) on Chondromalacia comparing both groups in a matched sample analysis (paired T-test analysis).
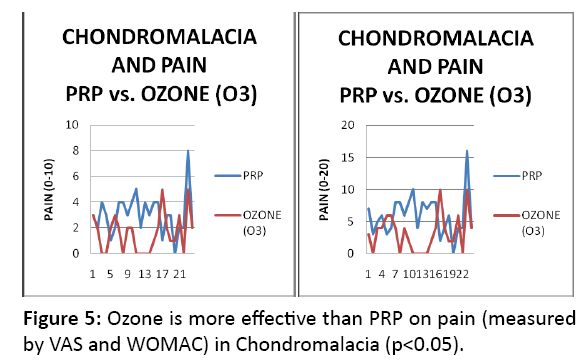
Figure 5: Ozone is more effective than PRP on pain (measured by VAS and WOMAC) in Chondromalacia (p<0.05).
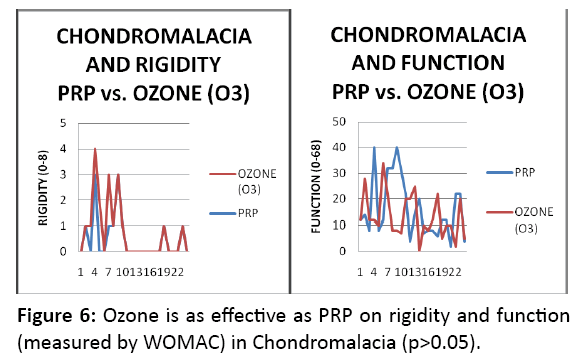
Figure 6: Ozone is as effective as PRP on rigidity and function (measured by WOMAC) in Chondromalacia (p>0.05).
Discussion
This is the first experimental study which compares the efficiency of PRP compared to Ozone infiltrations in the management of PFPS/Chondromalacia, using standardized treatment protocols. PFPS and Chondromalacia are considered part of the broad spectrum of anterior knee pain, with an important impact on the quality of life of patients, because of lost function and pain severity. These entities are frequent in young active patients and the natural history if untreated could progress to symptomatic OA [22]. There subsides the importance and the novelty of the study.
Articular cartilage is by nature avascular and a lymphatic and it has poor healing properties. The inflammatory and reparative processes do not repair properly injured cartilage at synovial joint. Chondrocytes located on the extracellular matrix do not migrate to the injured area. Even in the case that injuries affect subchondral bone, the underlying marrow cells stimulated would produce fibrocartilage, mainly of type I collage, which is biomechanical inferior [22]. This would explain the limited healing capacity of cartilage.
The conservative treatment includes NSAIDs and Physical Therapy and the surgical treatment implies different approaches such as micro fracture, autologous chondrocytes transplantation and autograft and/or allograft osteochondral transplantation [35]. However, the reported results from these procedures are variable, and they do not guarantee to prevent to progress to OA of the knee [22]. That was the main reason that made us to look up for new novel techniques such as PRP and Ozone.
In the case of PRP, there are few studies related osteochondral defects. To be more precise, only two studies were related to knee osteochondral defects (Scilari’s and Dolander’s studies) and one related to ankle osteochondral defects (Mae-Dan’s study) [36-38]. In the case of Ozone, there is only one study Fernández-Cuadros [25] that supports its treatment on PFPS/ Chondromalacia. Despite the paucity of studies, the previous promising clinical results obtained by the cited authors encouraged us to evaluate its efficacy in a non-randomized controlled trial. In our study, no differences were found between PRP and Ozone protocols. PRP is as effective as Ozone in the management of symptoms such as pain relief, function recovery and quality of life improvement. Besides, if we take a closer look at pain relief, Ozone diminishes pain even more than PRP (1.46 points on VAS scale and 2.95 points on WOMAC pain subscale) and with statistical difference. This is then the first human experimental report of successful reduction of pain and improvement on function, rigidity and quality of life secondary to Chondromalacia and/or anterior knee pain (PFPS), since there is neither conservative nor surgical therapy available, the current treatment strategies are not effective and there is no definite cure for these pathologies [35].
On PFPS/Chondromalacia, the etiology, diagnosis and treatment are difficult and its management constitutes a problem [39]. Fernandez-Cuadros and Perez-Moro argues that mechanical factors release proteolytic enzymes, mainly catepsines, to date one, which produce fibrillation and degradation of cartilage [25]. In the histological study of Chondromalacia patients, the synovial membrane shows some hyperemia and proliferation in almost all cases [40]. These histological observations suggest that inflammation subsides under this pathology [39]. PRP releases growth factors and cytokines that reduce inflammation, and stimulate cartilage regeneration [41]. Ozone could act on inflammation, modulate it and act on many other targets such as growth factors, stem cells, inflammatory cytokines, all of them could stimulate chondrocyte growth and cartilage repair [24]. All these reasons made us postulate PRP and Ozone as alternative promising options in the management of anterior knee pain secondary to PFPS or Chondromalacia, and issue that has been confirmed by our present study.
Recent studies state that PRP is capable to enhance the repair of tissues with poor healing ability as in the case of cartilage tissue [42]. Platelets play an important role in wound healing and hemostasis. Treatment with PRP delivers high concentration of platelets and growth factors directly to the wound site, which initiates and enhances wound healing. However, the effect of PRP is a function of many variables, including platelet concentration, procedures for concentration, platelet activation and the number of infiltrations, to date some of them [43]. The use of a standardized protocol for PRP elaboration is a great strength of our study.
Several cytokines produced by chondrocytes are implicated in the breakdown of extracellular cartilage matrix such as IL-1, IL-6, IL-17, LIF, TNF-α and IFN-Υ. All these cytokines produce cartilage destruction [24]. In the case of PRP treatment, PRP delivers high concentration of growth factors (TGF-β, ILGF, PDGF, BFGF, EGF, VEGF) and bioactive proteins; all of them stimulate angiogenesis and stem cells, inhibit inflammation and catabolic enzymes/cytokines, in order to repair cartilage injuries Figure 5: Ozone is more effective than PRP on pain (measured by VAS and WOMAC) in Chondromalacia (p<0.05). Figure 6: Ozone is as effective as PRP on rigidity and function (measured by WOMAC) in Chondromalacia (p>0.05). [44]. In the case of Ozone, Fernández-Cuadros have recently stated that Ozone acts on several targets that are implicated in the degradation cartilage and bone [24]. Specifically, Ozone inhibits MMP, NO synthesis, PGE2, IL-1, TNF-α, IFN-Υ, IFN-β; Ozone stimulates IL-4, IL-6. IL-10, IL-13, TGF-β, IGF-1, stem cells and chondrocytes [24]. All these assumptions made us considerer both treatment options as available for the management of anterior knee pain secondary to PFPS or Chondromalacia. Therefore, PRP and Ozone are both effective in decreasing pain and recovering stiffness and function, from the light of our results.
The age of our groups was 40.37 years for PRP and 45.87 years for Ozone. Several authors support that this pathology is common in young populations, as it is inferred from our results [24,39].
As far as we know, there is no study which compares PRP to Ozone in the management of anterior knee pain due to PFPS or Chondromalacia. However, Duymus et al. used a similar protocol (3 PRP infiltrations and 4 Ozone infiltrations) in the management of knee Osteoarthritis; then this was the only experimental study which compared both treatment options [45]. From his observations, it was established that PRP was more effective than Ozone in pain relief and function recovery. Those findings are very relevant because some researchers consider Chondromalacia as a precursor of OA [6]. On the contrary, from the results seen in our study, PRP is as effective as Ozone in pain relief, function recovery and quality of life improvement. Besides, Ozone is even more effective than PRP in pain relief. This is a slight but statistically significant difference that must be referred. From our observations, and with medicine-based evidence, we highly recommend PRP and Ozone for the conservative management of anterior knee pain secondary to PFPS or Chondromalacia.
Study limitations
There is paucity of studies that supports the use of PRP and/ or Ozone in the management of knee pain. More studies are necessary to confirm our promising results.
The placebo effect in the treatment of knee OA is relevant in terms of pain relief and function recovery, based on self-reported scores [46]. Novel interventions or those administered through needles produce larger placebo effect [47]. Future randomized controlled trials should be designed in a blind fashion, to minimize this placebo effect; better if the double-blinding, to patients and evaluators [48].
Conclusion
PRP and Ozone produce pain relief, function recovery and quality of life improvement in PFPS and Chondromalacia, measured by VAS and WOMAC scales. In the case of pain severity, Ozone produces even greater pain relief. PRP and Ozone are safe and effective modalities for the management of PFPS and Chondromalacia.
References
- Brody LT, Thein JM (1998) Nonoperative treatment for patellofemoral pain. J Orthop Sports Phys Ther. 28:336-344.
- Cutbill JW, Ladly KO, Bray RC, Thorne P, Verhoef M (1997) Anterior knee pain: A review. Clin J Sports Med.7:40-45.
- Thomeé R, Augustsson J, Karlsson J (1999) Patellofemoral pain syndrome. Sports Med. 28:245-262.
- Dixit S, Difiori JP, Burton M, Mines B (2007) Management of patellofemoral pain syndrome. Am Fam Physician. 75:194-202.
- O'Connor FG, Mulvaney SW (2016) Patellofemoral pain syndrome. USA: Up-to-date. Inc.
- Wiles P, Andrews PS, Devas MB (1956) Chondromalacia of the patella. Bone Joint J.38:95-113.
- Witvrouw E, Callaghan MJ, Stefanik JJ, Noehren B, Bazett-Jones, et al. (2014) Patellofemoral pain: consensus statement from the 3rd International Patellofemoral Pain Research Retreat held in Vancouver, September 2013. BJSM. 48:411-414.
- Fulkerson JP (2002) Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med.30:447-456.
- Dye SF (2005) The pathophysiology of patellofemoral pain: A tissue homeostasis perspective. Clin Orthop Relat Res. 436:100-110.
- Post WR (1999) Current concepts clinical evaluation of patients with patellofemoral disorders. AANA 15:841-851.
- Cook C, Hegedus E, Hawkins R, Scovell F, Wyland D (2010). Diagnostic accuracy and association to disability of clinical test findings associated with patellofemoral pain syndrome. Physiother Can.62:17-24.
- Haim A, Yaniv M, Dekel S, Amir H (2006). Patellofemoral pain syndrome: Validity of clinical and radiological features. Clin Orthop Relat Res.451:223-228.
- Bizzini M, Childs JD, Piva SR, Delitto A (2003) Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 33:4-20.
- van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma?Zeinstra S, van Middelkoop M (2015) Exercise for treating patell of emoral pain syndrome. Cochrane Library.
- Crossley K, Bennell K, Green S, McConnell J (2001) A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sports Med. 11:103-110.
- Oliveira VC, Henschke N (2012) Multimodal physiotherapy is effective for anterior knee pain relief. BJSM. 2012.
- Crossley KM, van Middelkoop M, Callaghan MJ, Collins NJ, Rathleff MS, et al. (2016) Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: Recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions). BJSM. 2016.
- Heintjes EM, Berger M, Bierma?Zeinstra S, Bernsen R, Verhaar JA, et al. (2004) Pharmacotherapy for patellofemoral pain syndrome. Cochrane Library.
- van der Windt DA, van der Heijden GJ, van den Berg SG, terRiet G, de Winter AF, et al. (1999) Ultrasound therapy for musculoskeletal disorders: A systematicreview. Pain. 81:257-271.
- Bolin D (2003) Transdermal approaches to pain in sports injury management. ACSM.
- Shanks P, Curran M, Fletcher P, Thompson R (2010) The effectiveness of therapeutic ultrasound for musculoskeletal conditions of the lower limb: A literature review. Foot. 20:133-139.
- Dold AP, Zywiel MG, Taylor DW, Dwyer T, Theodoropoulos J, et al. (2014) Platelet-rich plasma in the management of articular cartilage pathology: A systematic review. Clin J Sports Med.24:31-43.
- Kon E, Mandelbaum B, Buda R, Filardo G, Delcogliano M, et al. (2011) Platelet-rich plasma intra-articular injection versus hyaluronic acid visco-supplementation as treatments for cartilage pathology: From early degeneration to osteoarthritis. AANA. 27:1490-1501.
- Fernandez-Cuadros ME (2016) Could ozone be used as a feasible future treatment in osteoarthritis of the knee? DEHC. 13:232-239.
- Fernandez-Cuadros ME, Perez-Moro OS, Albaladejo-Florin MJ (2016) Patellofemoral pain syndrome and chondromalacia: The effect of ozone on pain, function and quality of life: A non-randomized controlled trial. JSM Phys Med Rehabil. 1:1002.
- Handbook for good clinical research practice of the World Health Organization and Declaration of Helsinki Principles (2016).
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW, et al. (1988) Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Clin Rheumatol.15:1833-1840.
- Wright RW(2009) Knee injury outcomes measures. J Am Acad Orthop Surg.17:31-39.
- Cho HJ, Chang CB, Yoo JH, Kim SJ, Kim TK, et al. (2010) Gender differences in the correlation between symptom and radiographic severity in patients with knee osteoarthritis. Clin Orthop Relat Res.468:1749-1758.
- Spector TD, Hart D J (1992) How serious is knee osteoarthritis? Ann Rheum Dis. 51:1105-1106.
- Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br. 43:752-757.
- Helms CA (1992) Fundamentos de radiología del esqueleto. Editorial Marban, España.
- Angst F, Aeschlimann A, Stucki G (2001) Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF?36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Care Res. 45:384-391.
- de Rooij M, van der Leeden M, Cheung J, van der Esch M, Häkkinen A, et al. (2017) Efficacy of tailored exercise therapy on physical functioning in patients with knee osteoarthritis and comorbidity: Za randomized controlled trial. Arthritis Care Res. 69:807-816.
- Pak J, Lee JH, Lee SH (2013) A novel biological approach to treat chondromalacia patellae. PLoS ONE. 8:e645-69.
- Siclari A, Mascaro G, Gentili C, Cancedda R, Boux E, et al. (2012) A cell-free scaffold-based cartilage repair provides improved function hyaline-like repair at one year. Clin Orthop Relat Res.470:910-919.
- Dhollander AA, De Neve F, Almqvist KF, Verdonk R, Lambrecht S, et al. (2011) Autologous matrix-induced chondrogenesis combined with platelet-rich plasma gel: technical description and a five pilot patients report. ESSKA. 19:536-542.
- Mei-Dan O, Carmont MR, Laver L, Mann G, Maffulli N, et al. (2012) Platelet-rich plasma or hyaluronate in the management of osteochondral lesions of the talus. Am J Sports Med. 40:534-541.
- Perez-Moro O, Albaladejo-Florin M, Entrambasaguas-Estepa B, Fernández-Cuadros M (2017) Effectiveness of PRP on pain, function and quality of life in chondromalacia and patellofemoral pain syndrome: A pre-test-pos-test analysis. Nov Tech Arthritis Bone Res. 1:55555.
- wales P, Andrews PS, Devas MB (1956) Chondromalacia of the patella. Bone Joint J. 38:95-113.
- Chahla J, Piuzzi NS, Mitchell JJ, Dean CS, Pascual-Garrido C, et al. (2016) Intra-articular cellular therapy for osteoarthritis and focal cartilage defects of the knee: A systematic review of the literature and study quality analysis. JBJS. 98:1511-1521.
- Wu PI, Diaz R, Borg-Stein J (2016) Platelet-rich plasma. Phys Med Rehabil Clin N Am. 27:825-853.
- Mochizuki T, Yano K, Ikari K, Hiroshima R, Kawakami K, et al. (2016) Platelet-rich plasma for the reduction of blood loss after total knee arthroplasty: A clinical trial. Eur J Orthop Surg Traumatol.26:901-905.
- Dai WL, Zhou AG, Zhang H, Zhang J (2017) Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. AANA. 33:659-670.
- Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Kesiktas FN (2017) Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. ESSKA. 25:485-492.
- Zhang W, Robertson J, Jones AC, Dieppe PA, Doherty M (2008) The placebo effect and its determinants in osteoarthritis: Meta-analysis of randomised controlled trials. Ann Rheum Dis.67:1716-1723.
- Doherty M, Dieppe P (2009) The “placebo” response in osteoarthritis and its implications for clinical practice. Osteoarthr Cartil.17:1255-1262.
- Shen L, Yuan T, Chen S, Xie X, Zhang C, et al. (2017) The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: Systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res.12:16.