Introduction
In the last few years, patient accessible electronic health records have been used more extensively in the United States, as well as other first world countries, as a promising solution to encourage patient involvement and shared decision making. The purpose of this was to improve compliance and outcomes in chronically ill patients, especially those who are prescribed multiple medications. Providing patient-oriented care is the foundation of ensuring patient involvement and active engagement that will result in positive outcomes. The physician-patient relationship has been given more focus recently, in efforts of optimizing the patient’s experience. Better communication between the two tends to show an increase in satisfaction, lessen the number of lawsuits against the physician, and have positive clinical outcomes. “Evidence has shown patient-provider communication is the most salient part of a medical visit” [1]. Better communication has also shown to have an effect on decreasing psychological symptoms, such as stress and fear.Chronically ill patients, such as those with diabetes mellitus type 2 and long-standing hypertension, show greater improvements after building a better relationship and communication pathway, with “improved drug treatment intensification, monitoring, and physiologic control among patients with diabetes, with great improvements amongst patients with worse control and less testing necessary”[2]. Therefore, it is best for society and the medical community, to emphasize and encourage a form of constant communication, such as electronic health records.
Electronic health records are a database where medical practitioners can document patient information, quality of care, medical billing and combined decision making is rendered possible. Another goal is to create a system where patients have access to normal lab values and use this to predict their health status and prevent uncontrolled disease or disability. The database is meant to be formatted as an easy and fast system that allows for tracking information and inputting information at a faster pace, while increasing face-to-face interaction time. Tracking patient utilization of tests, visits, and care in a hospital allows for managing of budgets and resources in different parts of the country. These statistics and financial data can improve out of -pocket costs for patients and healthcare facilities.
During the use of physical health records, transferring information between health care providers was deemed a hassle. A patient was responsible for having their medical history and charts forwarded to the new doctor. This leads to extra work for the staff, as they have to make copies of a file that could be thick in the case of a chronically ill patient. This takes out time from helping other patients. In the case of a hospital, the hospital will not give up those charts, so a patient would have incomplete medical history paperwork to provide the next physician.
Proper coding and billing of the encounter is essential for insurance companies to reimburse the physician. This means that all required information must be asked during the visit, which can be missed in an emergency or hasty situation. With electronic health records, the systemallows for accurate coding and recognizes errors. This prevents fines for fraud for billing without appropriate information.
In the medical field, patient confidentiality is a priority. HIPAA requires all medical providers to ensure patient information security or face harsh penalties. Electronic health records are safe in that they have deep security systems developed into them which prevents unauthorized access to a patient’s record. Some methods of security are personalized passcodes, biometrics, and firewall security. There is still a debate about whether physical or electronic records are deemed safer but electronic records do show who accessed health records at which time and from which IP address. Paper records would fall short of being able to do that.
With the utilization of electronic health records, physicians are able to consolidate all of a patient’s information into one portal, where both parties have access at all times. This also decreases the number of medical errors made in the medical setting, whereas handwritten patient information can be misinterpreted. Overall, it is believed that electronic health records increase “disease management, educating and empowerment of patients to improve their health status, and improving effectiveness of the medical visit” [1]. However, electronic health records have also faced a great amount of resistance from society.
Patient care was the main goal of many discussions in the studies reviewed. It is considered that patient care serves as a basis for the successes and weaknesses of the electronic health records used in medical settings. Electronic medical records can be utilized to improve communication between primary care physicians and their team members. Charts, notes, and prescriptions are in clear, concise format and legible. This reduces medical errors and allows easy access to scheduled appointments as well. On the other hand, the patient has a portal as well, where they are able to manage their own care and review information provided at their previous appointments.
As the usage of electronic health records is increasing, the consequences have followed. Some of the barriers found were limitations of standardization, attitudinal and organizational constraints, behavior of both physician and patient, and resistance to the change. Additionally, improper use of the electronic health records can cause serious endangerment of patient’s information as well as their medical regimen. Some patients do report that their in-patient visits have been shortened by this method and have become depersonalized as everything is based on inputting information into a screen, where the physician is not making direct eye contact with the patient. It is approximated that a physician spends around 35% of their time documenting information instead of communicating with the patient, where they were “taking extra time to use the electronic health records and not being compensated for taking a lighter load”[3]. This shows lack of attention to the patient and their physical behavior or other noteworthy details. Physicians believe that electronic health records are helpful because it allows them to see more patients, and search for information in a patients file with a click of a button instead of sorting through a file of papers.
Initially, electronic health records were formed for billing purposes, and not for improvement of patient care and communication. Therefore, the purpose was to increase and improve accuracy and performance of billing and physician activity.
Although there are multiple studies looking at the changes related to electronic health records, it is not certain that electronic health records are associated with “improved patient outcomes in comparison with individuals who did not use electronic health record tools frequently”[4]. The purpose of this paper is to determine whether patients, especially those with chronic health conditions, are showing improvements in their outcomes and physician-patient communication with the use of electronic health records.
Methods
The purpose of researching the articles utilized in this review paper was to acknowledge the pros and cons of electronic health records on patient care and health improvement. Furthermore, another goal was to identify why physicians deemed electronic health records a positive addition to their work environment. Search engines such as Google Scholar and PubMed were utilized to obtain articles related to the hypothesis. The articles were helpful in understanding whether the hypothesis should be accepted or nullified.
Once a relevant article was found, the abstract was read. If the article’s abstract was similar to another article’s, the latter article was not included in this review paper. Additionally, if an article was related to electronic medical records in the emergency setting, the article was not utilized. In efforts of narrowing the search results and finding articles suitable for representing the purpose of this review, certain search terms were utilized. These search terms were “electronic medical records”, “chronic patients”, “blood reports”, “online medical information”, :physician-patient relationship”, “patient perspectives”, “patient portals”, “patient-centered care”, “telemedicine”, “eHealth”, “decision support systems”, “health information technology” and “information and communication technology.”
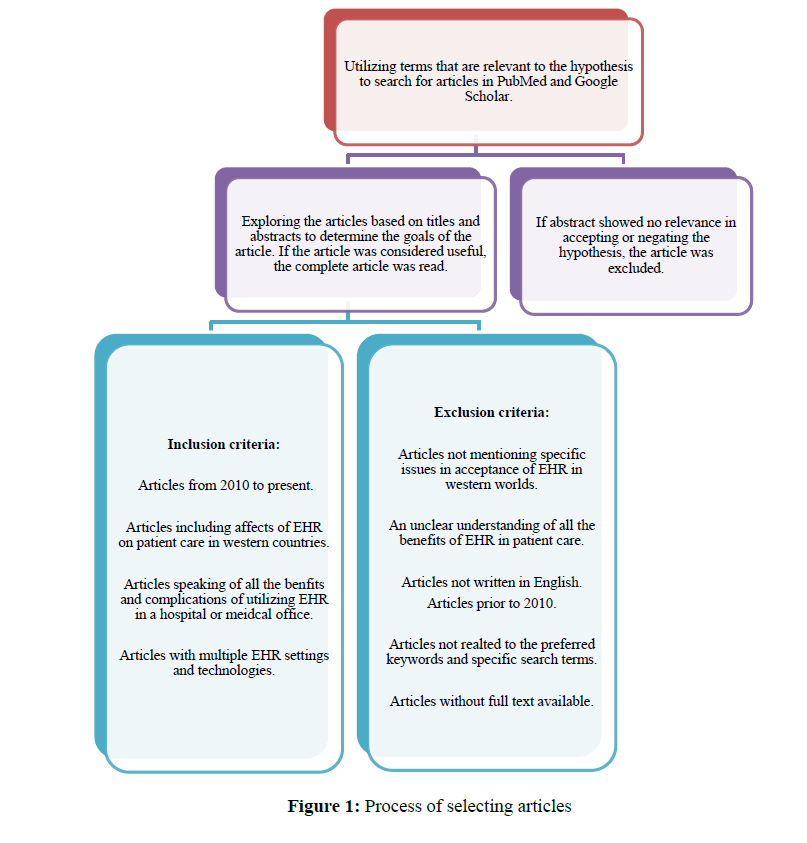
Alongside search terms that were used to find articles, an inclusion and exclusion criteria was also utilized. Figure 1 clarifies how each appropriate article was selected to be a component of this review paper. Exclusion criterions were articles written prior to 2010, which allowed for a ten-year time frame, research centered articles, and articles that are correlated with the hypothesis that were not solely focused on one patient group or one location in the world. Furthermore, the inclusion criteria required articles to be related to the hypothesis, and articles with a conclusion that assists in deciding whether electronic health records have improved the health care environment as a whole or not (Figure 1).
Figure 1: Process of selecting articles
In order to find the most reliable information, many articles were reviewed for this paper. In order to make sure that the information was pertaining to the hypothesis of this review paper, a total of 11 articles were used for analysis. The list can be located in Table 1. It is important to note that the articles found in Table 1 were utilized in both the results and discussions section. If an article was only utilized in the results or only for the discussion section, it was cited in the references, but is not found in table 1. Moreover, to additionally simplify this information, table 2 shows a summary of how many articles of each study design were used for this review paper (Table 2).
| First Author |
Year of Publication |
Type of Study |
Level of Evidence |
Outcome/Results |
| Lavallee, D. |
2016 |
Observational Study |
IV |
New policies, funding, reform, and efforts to improve health care have created an environment suitable for the successful implementation of patient reported outcome measures in clinical practice. |
| Grabenbauer, L. |
2011 |
Qualitative Study |
VI |
Physicians are optimistic about EHR’s potential for data collection to improve patient care, but are not completely comfortable with the existing interface yet. |
| Seymour, T. |
2014 |
Systematic Review |
IV |
The healtcare industry is going through revolutionary changes. EHR is transforming healthcare for the better and increasing quality of patient care. |
| Yanamadala, S. |
2016 |
Observvationl Study |
IV |
EHRs are associated with decrease in measures of inpatient mortality, readmissions, and increasing patient safety. |
| Atasoy, H. |
2018 |
Systematic Review |
VI |
By combining information from thousands of patinets and trials, these systems will be able to create new medical data that will decrease costs and provide guaranteed treatment options for chronically ill patients. |
| Manca, D. |
2015 |
Observational Study |
IV |
We are just starting to reach our potential of using EHR for beenfiting the patient and we will soon see much more progress. |
| Rothman, B. |
2012 |
Case Series |
IV |
EHR allow data-mining opportunities which improve all the preferred aspects in the healthcare setting. It has potentional to reduce costs and improve quality of patient care. |
| Migdal, C. |
2014 |
Retrospective Cohort |
III |
EHR’s may improve communication between doctor and patient. Future research is needed to validate this improvement. |
| Zarcadoolas, C. |
2013 |
Qualitative Study |
VI |
Patients were excited to utilize portals and found them of value. Findings suggeested that the portal should be easy to read and manuver, engage consumers, and be user friendly. |
| Neves, A.L. |
2018 |
Systematic Review |
VI |
Assess the risks and benefits of interventions using electronic health records. Asses the contribution of this to short-term and long-term frames. |
| Campanella, P. |
2015 |
Meta Analysis |
IV |
EHR systems can improve the quality of healthcare and should be implemented in healthcare settings. |
Table 1: Evidence table of review articles.
| Study Design |
Number of Studies Reviewed |
| Observational Studies |
3 |
| Retrospective Cohort |
1 |
| Systematic Review |
3 |
| Meta Analysis |
1 |
| Case Series |
1 |
| Qualitative Studies |
2 |
Table 2: Summary of study designs reviewed.
Results
Stakeholders have gained interest in capturing patient reported outcomes for better patient care. In the U.S.A., the 2009 Health Information Technology for Economic and Clinical Health Act was passed to devote billions of dollars to assist in adopting the use of electronic health records amongst clinicians and hospitals. The purpose of that is to improve quality of care, encourage collection of data electronically, and shared decision making. Online consumer communities are also assisting in the progression of patient involvement in electronic health records. For example, one social media platform that is used often is called “PatientLikeMe” which allows for patients with similar illnesses to connect and discuss their experience and influence each other to use newer technologies [5].
While analyzing multiple studies, there were multiple components of quality that were pinpointed. These components were physician-patient communication, efficiency, effectiveness, equity, timeliness, safety and security,technologies patients prefer, and transitioning into the new technological world.
Physician-patient communication
Patients felt that having eye contact with their physician was an essential component of their visit and helped communicate better. They took eye contact to be a form of understanding and a sign that the physician was focusing on them. Better eye contact allowed for a more personal connection between the patient and physician [6].
Patients understand that physicians have to enter data in the electronic health records, but when a physician was able to balance that better the patient felt more comfortable and felt their needs were still being prioritized [7].
Patients also felt that when physicians were explaining what they were doing throughout the visit and what they were putting into their electronic health records, they were on the same page with the physician. Patients believed that when the physician had their back turned to them to type on their computer, patients saw this as a form of neglect or lack of communication.
The best set up for a relatively positive physician-patient communication stream is to have the patient sitting next to them at the desk, where the patient is aware of what is being noted in the electronic medical records. This also allows for a constant state of communication and lessens the sense of being ignored. Patients also appreciated when the physician discussed the patients’ current situation and current management of their illness prior to directing their attention to the computer screen to look at the patient’s history and further discussing the situation. Additionally, the patients appreciated being involved in the documentation process as well as discussing test results that are found in the electronic health records. All of these changes allowed for a constant route of communication and comfort between the doctor and patient [7].
Efficiency
The purpose of having efficient healthcare is to make sure that there are not financial or human resources being wasted. Electronic health records are a tremendous help as they reduce excessive test orders and can reduce the amount of time and effort spent on nonpatient care related tasks such as documentation and searching for previous paperwork. According to Yanamadala’ s study, there were “significant differences in rates of mortality, readmission, and complication in patients staying in the hospital with full electronic health records or partial electronic health records compared to hospitals with no electronic health records” [8]. Overall, studies showed a decrease in the number of lab tests orders and a decrease in provider costs as well saving time with each patient encounter since more time was utilized in communicating with the patient. Sharing required medical information and lab work between two providers via the “health information exchange has reduced the number of duplicate tests and procedures” patients needed to get done [9]. There is a very wide range of efficiency outcomes but overall, the use of electronic health records has allowed for an easy way to retrieve available data [8].
Effectiveness
Effective healthcare delivery is done in harmony with scientific information. Electronic health records increase effectiveness by setting guidelines and providing practice material available at the point of care. Many studies have analyzed whether physician computer usage increases their adherence to guidelines or if the standard of healthcare still varies amongst physicians. These studies showed improvements and increase in clinician and patient responsiveness to electronic health record reminders. Overall, electronic health records are a benefit to the healthcare system but have room for improvement [10].
Patient-centeredness
Providing patient centered health care is essential in assuring that the patient is comfortable and will comply with the medical advice provided to them. This would acknowledge the patients preferences and values, such as religion and culture. This can also include patient accessible personal health records or disease management tools that allow patients and their health care providers to communicate and share information outside of the hospital or clinic setting. This allows for “data in real-time” which holds the patient accountable for their illness and the physician is aware of everything that is going on as well [11]. Studies show that patients are enthusiastic about the use of electronic health records. They enjoy having access to information about their health, opening up doors for furthering their knowledge and improving the quality of their health care [12].
Equity
In order for a physician to perform at their best, they must understand that every patient is equal regardless of their characteristics. Electronic health records and other medical technological advancements are improving patient equity by ensuring that the patient has access to information on free website portals and allowing for underserved populations to receive better care. These improvements depend on the appropriate use of electronic health records who serve these populations. Electronic health records have also been found to be more common in the urban communities and less common in health care providers who serve the minorities. Therefore, these communities were less educated and had less personal access. “By providing increase increased access to health support, it may help ameliorate disparities in the disadvantaged groups”[13]. In order improve equity in low-income communities, it is important to ensure there are no disparities in technology adoption in those serving them and understand and diminish the barriers set in society [10].
Timeliness
Timely healthcare is necessary for achieving the best results. Elimination of long wait times or delayed access to health care can decrease a number of potential health consequences. Technologies such as telemedicine can connect the physician to the patient, which was used in 2020 during the COVID-19 pandemic. This allowed for patients to resume their appointments with physicians without having to go to the office. This access can allow for disabled and elderly patients to access healthcare easier and potentially increase their lifespan. It is also shown that the use of electronic health records allows for “quick medication and procedure turnaround times” since physicians forward medication prescriptions to the pharmacy or specialists directly [14].
Electronic health records patients prefer
Patients believe that the utilization of electronic health records allowed for more time with their physicians, enhancing the overall quality of the visit. They noticed that with patient data already available inthe database, physicians felt less of a need to re-ask questions that were asked in previous visits. Overall, patients felt the communication with their physician was not impaired with the addition of electronic medical records; it actually built a better rapport between the physician and patient. The patients felt the length of the visit was not rushed even though there was previous data available, and note taking was quicker. There was more time to communicate and speak about how the patient felt, rather than focus on the diagnosis [10].
Patientsstated that the majority of their satisfaction with electronic medical records was due to the improvement in their communication with the physician. They also note that this method of data storage allows for medical practitioners to share a patient’s medical information and coordinate patient care and management with other providers via electronic medical records. Another huge benefit from prior was receiving test results quicker. Paper results take a longertime to be processed and reported to the physician, who then communicates with the patient. With electronic medical records, physicians were able to search through results quicker to look for specific lab findings and save time, and shorter screen time during the appointment.
One method that physicians used with patients to establish a better understanding of their long-term health and management was the usage of data trend charting. For example, patients with diabetes mellitus were shown their blood sugar levels on a chart and the change self-management showed on the chart, which encouraged patients to abide by their treatment. Patients did not have a full understanding of what A1c was, describing it as a “some silly numbers,” but once they saw the data on the computer, they had clarity of what it is they were trying to change and how the medication and change in daily habits helped accomplish that [7].
Patients admit that the thickness of a physical medical records file was traumatic for their mental health, as it was a reminded of their chronic illness. It made them feel like they were not normal and was not able to handle the burden of their illness. Overall, majority patients showed greater satisfaction with electronic medical records.
Patient safety andinformation security
Patient safety refers to the specific care the patient gets, which is free of medical errors. Electronic health records can be effective in checking for errors in prescription orders and proper administration or medication. It requires hospitals and clinics to abide by the established guidelinesand have high quality documentation. Nonetheless, findings have shown benefits of electronic health records on infection control and decreased infant mortality.
Many information security issues were brought to light during this review. Physical health records tend to get misplaced, files become unorganized, and pages can rip out. Patients complained of their physician taking extensive amount of time to go through the file to find previous vitals, height and weight measurements, or previous reports to use as a comparison. In some cases, physicians could lose the patients lab report and would require their patient to repeat testing which became a hassle. With electronic health records, information was sorted and always in its respective place in each patients file, and less time is wasted [7].
In situations where a patient’s prior notes were not located, physicians would attempt to ask patients for a summary of their previous visit, which results in decreased confidence and reliability in the physician. Patients did not feel comfortable with having a physician be irresponsible with their personal information, and this strained their relationship with their physician. Patients found having to remind physicians of their illness as a “turn off” [7]. These issues have been resolved with the use of electronic health records. The medical records were more accessible and chronologically accurate. Patients list of prescriptions were concise and listed in order and were easily shared with other physicians if need be. Patients also found that illegible handwriting in physical medical records was a source of miscommunication between two physicians, the pharmacist, or the patient themselves. This barrier no longer exists [7].
Patients are informed about electronic health records and know that the spell check feature helps fix any errors made and both generic and brand names are available on their list of prescribed medicine. Physicians are able to type up notes and read back information to confirm from patients, increasing the patient’s confidence in their physician’s data. Easier and faster access to this data and lab work was a huge relief for patients as it lessened the fear of their personal information being scattered and misplaced. Overall, patients found their information to be more secure in the electronic medical records. Patients found physical health records to be a short-term form of information storage as paper and ink are fragile and will not last forever, whereas data saved on a database can be secured and last longer with many more benefits [14].
Transitioning to the new technological world
Electronic health records first came around in the medical setting in 2008. In those times, the patients noticed that the learning and adjusting process was frustrating for most physicians and medical workers. Documentation and functions of electronic health records were difficult. Patients found the electronic health records to be a barrier between their communications with their physician due to physicians giving more attention to learning how to utilize the system.
Patients claimed that their physicians computer skills such as typing without having to look was one main reason why eye contact was decreased, and more attention was put into how to maneuver through the system. Patients were fearful that information would not be stored correctly, and they would be misdiagnosed, or lack of attention would lead to poor management [15].
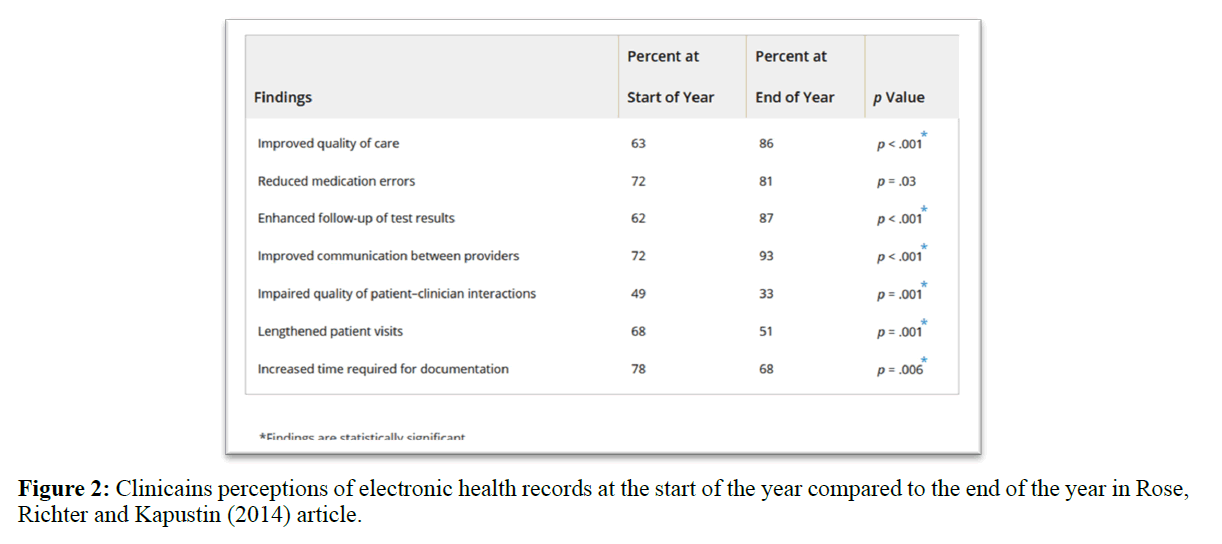
Overall, the results of this review paper show that there is significant improvement in patient care once hospitals and clinics have access to electronic health records. Patient engagement and enthusiasm increases which in return leads to better compliance. As Figure 2 shows, between the start and end of the year, patients have confirmed better quality of care, decreased errors and prolonged visits, improved communication and results. The combined findings of all the studies show that like everything else, there is room for growth, but with the utilization of electronic health records, the medical community can progress tremendously (Figure 2).
Figure 2: Clinicains perceptions of electronic health records at the start of the year compared to the end of the year in Rose, Richter and Kapustin (2014) article.
Discussion
The benefits of implementing a protected electronic health records system are tremendous as shown in Figure 2. Some of these are increased productivity, efficiency, accuracy and providing health records at a timely manner which collectively improves the quality of health care [8]. The use of electronic health records enables patients to get involved and be informed as often as possible, giving them control of the future of their healthcare. Majority of the patients interviewed claimed they have used “computers, the internet and mobile devices”while others from lower socioeconomic status did not use communication technology prior to the study but were eager to learn how to access their information. According to Zarcadoolas study, “younger patients were more comfortable with eHealth tools and saw it as a hassle-free mode of communication [13]”. Vulnerable populations normally receive low quality healthcare, and some say, the usage of electronic health records and portals would help decrease those disparities in disadvantaged groups. Studies showed this population showed interest in accessing their medical records, so they could do what they can afford to do. Overall, patients felt many of the physician’s communication techniques were an effective method in upholding communication while using electronic health records.“Physicians are optimistic about electronic health record for systematic data collection to improve patient care”[6]. Physicians were able to establish and maintain rapport with patients by asking patients how they were feeling, what brought them in, how to manage their disease, keeping constant eye contact, and alternating between typing notes into the database and keeping the conversation going. As a physician was typing, they were also explaining what they were doing which allowed for patients to be informed and comfortable. When a physician turned their back to the patient during notetaking, it seemed to come off as a form of barrier in communication. As a whole, most patients did not believe that physicians spent more time looking at the computer and did spend an appropriate amount of time paying attention to the patient [15].
With the change from physical health records to electronic health records, patients were able to notice multiple changes. In addition to clinical care benefits, Atasoy states, “electronic health records can automate existing processes, improve management of medical practices and chronic care, and facilitate integration and communication within health care organizations [9].” One of the most helpful changes was that documentation took less time with electronic health records and allowed for more time to discuss the medical issue at hand and discuss management and long-term treatment or goals. Patients noticed that physicians were asking previous questions less often which decreased the frustration of repeating the same thing over and over at each visit. Patients also noticed that electronic health records allowed for obtaining lab reports back much quicker than previously. This decreased the hassle of sharing information between the physician and patient. With access to a patient portal that is connected to the physician’s electronic medical records, the consumers take control of their health and change the standards of doctor-patient communication. “Electronic medical records provide treatment goals and alerts to remind patients and healthcare providers” when certain lab levels are out of range and preventative medication is due [10]. These patients also noticed that electronic health records allowed for a variety of medical care providers to communicate with each other much quicker and collaborate on treatment plans. With the utilization of electronic health records, patients left the office with less negative emotions and claimed they were greatly satisfied with their overall care. Studies also showed that patients were engaging in their health and listening to physician’s requests for screening exams and adherence to preventative measures for chronic illnesses. As stated in Campanella’s study, “electronic health records reduced the costs associated with medical errors, adverse drug effects, and time inefficiency.”Patients believed that there were more medical errors in physical health records and their care was safer with the use of electronic health records [15].
Patients were able to vividly remember the implementation of electronic health records and the learning process. The patients were aware that the physicians were adjusting to a new system and their learning process was slow, and the communication between the physician and patient was affected until the physician was comfortable with the system and how to use all the functions. The increasing applications and complex tasks physicians can perform using electronic health records alongside the pressure to adapt to the new systems rapidly open up room for patient safety hazards. The transition period for the medical providers was very uncomfortable for patients and left them feeling vulnerable to data errors and lack of attention [11].
When new physicians and medical practitioners are learning the ways of electronic medical records, it is important for them to acknowledge the importance of eye contact with patients and ensure there is no barrier of communication. It is also important to talk to the patient, face to face, before turning away to type into the computer, which is where a physician should also explain what they are putting into the system to allow for the patient to feel involved in their care. Interspacing taking patient notes and conversation with the patient is highly important for the maintenance of a stream of communication. Migdal stated that one of the methods of increasing communication between the physician and patient in the hospital setting was to “provide patients with an interactive tablet that details their care” to improve patient comfort [12]. This can also be substituted with a patient portal login to utilize on their own devices. The personal connection between a patient and physician allows for the physician to learn more and the patient to open up about their true diagnosis more.
One of the greatest blessings that patients found in the electronic health records was that medical practitioners were able to show how proper medication usage would affect the patients prognosis, how changes in lifestyle could assist in prolonging lifespan as well as decreasing the rate at which the patients’ health declines, and lastly, how to manage their health and behavior via their electronic health records, to decrease the extent of their illness. Having access to electronic health records provided “continuity of care and patient convenience for the patient” which was found to be convenient for the patient [14]. Exam rooms were also designed in a way so that communication is constantly facilitated, and the patient is involved as much as possible. Another benefit was the use of capturing patient-reported outcomes regarding symptoms and the severity of it, which allowed for a larger scaled view of which medications caused side effects, possible correlations to other comorbidities, and future prevention. For example, Lavallee explained that “the oncology care unit collected patient reported symptoms to via electronic health records, reported from the patients device wherever they were, to help clinicians discuss the impact of chemotherapy drugs” [5]. Such real-time data allows for a better understanding of why certain adverse events take place in patients and helps researchers find out how to prevent future incidences.
As Seymour stated, “the healthcare industry is at the threshold of one of the biggest revolutionary changes in healthcare practice in modern times,” and embracing the changes and learning how to use them for everyone’s benefit while also making them accessible and easy to utilize is the goal [7]. This expansion in healthcare will open more doors to management, treatment, and patient care and information as a whole.
Future Directions
The future of electronic health records is positive, and the technologies being used in the medical setting are constantly evolving. This will allow for all health care providers to utilize the system to improve care and allow more timely communication and diagnosis of patients with multiple health care providers. The possibility of decreasing health care costs can become a reality with the use of data mining which allows for physicians to track which chronic diseases are more common in certain areas of the world, allowing for better equipped offices and hospitals, leading to better management. One of the main goals of electronic health records is to analyze how a variety of medical treatments affect the outcome of chronic illnesses. Seeing positive or negative trends helps decide which medications result in best outcomes and deserve the funding. With the assistance of electronic health records, interoperability will rise, and patient health data can be shared across the healthcare field.
Newer technologies come with new ways to increase efficiency and help improve workflow. Bar coding is a form of electronic health records that has been used vastly in the Western world. It is most common in the hospital setting as patient wrist bands, specimen collecting contains, blood collection containers, and supplies. This helps verify patients and track the patient as a whole for all their medications and past visits. Sometimes this can show a pattern of a disease or it can show factitious disease behavior. Another electronic health records system that has been brought into the healthcare world is RFID, radio-frequency identification, which allows for managing of patient safety, tracking of surgical instruments, and automatically refilling orders for more instruments and billing payments. It also manages sterilization quality. RFID also tracks patients in large hospital settings, so physicians and other health workers are able to check where the patient is at that moment. The most important reason for using RFID is to ensure that you are communicating with the correct patient, providing the correct procedure at the appropriate time.
One of the newer technologies that are used are speech recognition technology that allows for dictation of notes which is a much quicker process of note taking. It is a system that is very accurate and able to adapt to phrases and accents.
Patient portals linked to a physician’s electronic medical records will help engage people with their medical health, improve preventative behavior, and manage chronic conditions. Users have found value in the patient portals, including patients with mental health and substance abuse related issues. HIV patients are also taking advantage of the new technology to track charting of their CD4 count after each visit. The portal has increased curiosity, improved patient knowledge of their illness, empowered them to monitor and learn more, and most importantly increase self-care, whether it is lifestyle changes or medical compliance.
In order to do more research and confidently confirm that electronic health records are beneficial to patient care, it is important to examine waiting times and consultation times in a variety of cities and different hospital settings. Some of the other factors that need to be identified are the reason for each individual’s visit, the number of staff available, and how many patients are incoming in the different settings. Although electronic health records are deemed cost-effective, the equipment, its maintenance and repair can become an immense cost to the hospital. Smaller hospitals in rural cities cannot afford such luxuries. Laggings software or poor internet speeds can lead to prolonged wait times and negative experiences. A crash in the system would require a backup system, which is another cost. Security as mentioned before is very vital in the medical community and electronic systems are prone to hackers who take over systems for a ransom. This does not always happen, but any hospital can become a target. Medical identity theft would also be an issue. Knowing all this, we weigh the benefits with the risks and acknowledge that having knowledge and control of your health is what is most important. Although there are plenty of risks, being able interpret one’s health from information provided and track progress, a patient is more likely to comply with their medication routine and lifestyle recommendations.
Limitations of Research
The qualitative studies were limited to patients in the United States and urban cities. As with any other research groups, patients can change their responses based on the study being done, opinion, the way the questions are being asked and their personal opinion of technology. Patients can also change their viewpoints based on what other patients stated, and their mental state at the time of interview. Participating patient’s opinion could also have been swayed by empathy for the physicians learning process of electronic health records. Another limitation that can be a factor to the patients experience is how well the physician understands the format of the system and the constant evolvement of the system and its effect on communication. Moreover, information about the technology that shapes the software was not included in most studies that were reviewed.Lastly, patients education level, or racial and ethnic minority can cause for a swayed opinion. These limitations should be considered in the future of studies related to electronic health records.
Conclusion
The healthcare industry is facing its greatest revolutionary changes in the past decade. As hypothesized, if the appropriate software and IT are utilized, the industry will grow tremendouslyallowing for positive health outcomes. It can help decrease the national cost of healthcare, especially in the United States. Most patients were enthusiastic about patient portals ad electronic health records and found it to be of great value to their health management. Patients felt more empowered through their own access as way of retaining more information from their doctor’s visit. Patient portals were most effective for consumers when they were easy to read, colorful and engaging, have easy-to-use navigation. Patients overall found online medical records to be useful in communication with health care providers. As hypothesized, implementation of patient engagement and increased workflow were helpful for allowing a better understanding between the patient and physician leading to improvement in medical outcomes in chronically ill patients. Cumulatively, the studies showed that improvements were made in quality of health care received, increased efficiency was noted, and reduced errors were found. In today’s era, electronic health records have become a lifesaver as the pandemic has caused multiple nations to shut down. Patients were able to maintain their health care via telehealth, where they had face to face calls and lab reports were uploaded onto an app. In times like these, telehealth and electronic medical records and resources have more pros than cons. Therefore, electronic health records should be implemented in medical offices and hospitals. Lastly, the future of healthcare depends on the ventures of successful technologies that are being founded and allowing for management and communication at a larger scale, while also making health care affordable.
References
- Dale Rose, Louiseann T Richter, Jane Kapustin (2014) Patient experiences with electronic medical records: Lessons learned. J Am Assoc Nurse Pract 26(12): 674-80.
- Mary Reed, Jie Huang, Ilana Graetz, Richard Brand, John Hsu, et al. (2012) Outpatient Electronic Health Records and the Clinical Care and Outcomes of Patients with Diabetes Mellitus. Ann Intern Med 157(7):482-9.
- SimaAjami 1, Tayyebe Bagheri-Tadi (2013) Barriers for Adopting Electronic Health Records (EHRs) by Physicians. Acta Inform Med 21(2):129-34.
- Karla Lancaster, Aseel Abuzour, Manmeet Khaira, Annalise Mathers, April Chan, et al. (2018) The Use and Effects of Electronic Health Tools for Patient Self-Monitoring and Reporting of Outcomes Following Medication Use: Systematic Review. J Med Internet Res 20(12):e294.
- Danielle C Lavallee, Kate E Chenok, Rebecca M Love, Carolyn Petersen, Erin Holve, et al. Incorporating Patient-Reported Outcomes into Health Care to Engage Patients and Enhance Care. Health Aff (Millwood) 35(4):575-82.
- L Grabenbauer, A Skinner, J Windle(2011) Electronic Health Record Adoption - Maybe It's not about the Money: Physician Super-Users, Electronic Health Records and Patient Care. Appl Clin Inform 2(4):460-71.
- Tom Joseph Seymour, Dean Frantsvog, Tod Graeber (2014) Electronic Health Records (EHR). Am J Health Sci (AJHS) 3(3): 201-10.
- Swati Yanamadala, Doug Morrison, Catherine Curtin, Kathryn McDonald, Tina Hernandez-Boussard (2016) Electronic Health Records and Quality of Care: An Observational Study Modeling Impact on Mortality, Readmissions, and Complications. Medicine (Baltimore) 95(19):e3332.
- Hilal Atasoy, Brad N Greenwood, Jeffrey Scott Mc Cullough (2018) The Digitization of Patient Care: A Review of the Effects of Electronic Health Records on Health Care Quality and Utilization. Annu Rev Public Health 40:487-500.
- Donna P Manca (2015) Do electronic medical records improve quality of care? Yes. Can Fam Physician 61(10): 846-7.
- Brian Rothman, Joan C Leonard, Michael M Vigoda (2012) Future of Electronic Health Records: Implications for Decision Support.Mt Sinai J Med 79(6):757-68.
- Christopher W Migdal, Aram A Namavar, Virgie N Mosley, NasimAfsar-manesh (2014) Impact of Electronic Health Records on The Patient Experience in a Hospital Setting. J Hosp Med 9(10):627-33.
- Christina Zarcadoolas, Wendy L Vaughon, Sara J Czaja, Joslyn Levy, Maxine L Rockoff (2013) Consumers' Perceptions of Patient-Accessible Electronic Medical Records. J Med Internet Res 15(8): e168.
- Ana Luisa Neves, Alexander W Carter, Lisa Freise, Liliana Laranjo, Ara Darzi, et al. (2018) Impact of sharing electronic health records with patients on the quality and safety of care: A systematic review and narrative synthesis protocol. BMJ Open 8(8): e020387.
- Paolo Campanella, EmanuelaLovato, Claudio Marone, Lucia Fallacara, Agostino Mancuso, et al. (2015). Impact of electronic health records on healthcare quality: A systematic review and meta-analysis. Eur J Public Health 26(1):60-4.