- (2011) Volume 12, Issue 2
Tamas A Gonda1, Muhammad Wasif Saif2
1Division of Digestive and Liver Disease
2Division of Hematology and Oncology; Department of Medicine, Columbia University Medical Center. New York, NY, USA
Pancreatic cancer presents at an advanced stage in majority of the patients, hence resulting in a very dismal prognosis. Novel and effective methods to detect and screen pancreatic cancer and its precursors are warranted. The U.S. Multi-Society Task Force recommends against routine screening for pancreatic cancer in asymptomatic adults using abdominal palpation, ultrasonography, or serologic markers. Moreover, the screening for persons with hereditary predisposition to develop pancreatic cancer has not been validated. Herein, the authors summarize the data presented at the 2011 American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium in detecting early stage pancreatic cancer (Abstracts #187 and #193).
Early Detection of Cancer; Metabolomics; Methylation; Pancreatic Neoplasms
Despite considerable advances in the management of pancreatic cancer it remains one of the most lethal solid malignancies in adults [1]. One of the reasons for this grim statistic is that the majority of pancreatic cancer is recognized at advanced stages, when curative-intent resection is not feasible and currently available treatment options have limited efficacy [2]. In recent years early genetic and epigenetic changes and precursor lesions have been recognized, as well as at risk populations have been identified [1, 2, 3]. These discoveries are beginning to yield strategies that may allow for early diagnosis and/or screening for pancreatic cancer in select populations.
However, the limited ability of current imaging modalities to reliably identify precursor lesions and the epidemiology of pancreatic cancer make it challenging to identify an effective screening strategy. Although screening for pancreatic cancer is not recommended by society and national practice guidelines in the general population, strategies such as cross sectional imaging (CT or MRI), endoscopic ultrasound and testing for early glucose intolerance or serum markers (CA 19-9, CA 72) are employed in select (higher then average risk) populations [4]. Detection of molecular changes in blood, fecal or urine specimens holds tremendous promise in screening as these specimens are readily available and unlike other strategies are non-invasive and potentially more specific. In this report we summarize some of the exciting developments in the field of non-invasive pancreatic cancer screening presented at the 2011 ASCO GI Cancers Symposium. Fecal DNA analysis and metabolomic methods are summarized and the preliminary results from the presentations are reported.
Power of Fecal DNA Methylation Analysis: Does It Lead to Development of a Noninvasive Screening Tool for Pancreatic Cancer? (Abstract #187) [5]
Fecal DNA testing for screening of gastrointestinal malignancies has been used in research studies for the early diagnosis of esophageal, gastric and colorectal cancer. First generation tests focused on detection of commonly known genetic mutations [6], and subsequent ones included markers of microsatellite instability (MSI) [7], DNA integrity assays [8] and most recently analysis of promoter CpG island methylation changes [9]. The addition of markers other then gene mutations has allowed for an increasing sensitivity for the detection of not just cancers but adenomas as well [10, 11]. Although the panel of DNA level changes continue to evolve and the methods to isolate high quality, human DNA from stool are improving the acceptance of stool DNA testing as a screening modality for colorectal cancer by the American Cancer Society (ACS), U.S. Multi-Society Task Force and the American College of Radiology (ACR) already underscores the potential viability of this strategy [8, 12]. However, non-invasive molecular screening tests for luminal malignancy in the gastrointestinal tract will eventually need to be compared to endoscopy, which offers great sensitivity and a therapeutic intervention (polypectomy). In this regard, the utilization of stool based DNA testing would be much more ideal for screening for cancers where recognition and treatment of precursor’s lesions is not available. Pancreatic cancer fits this profile.
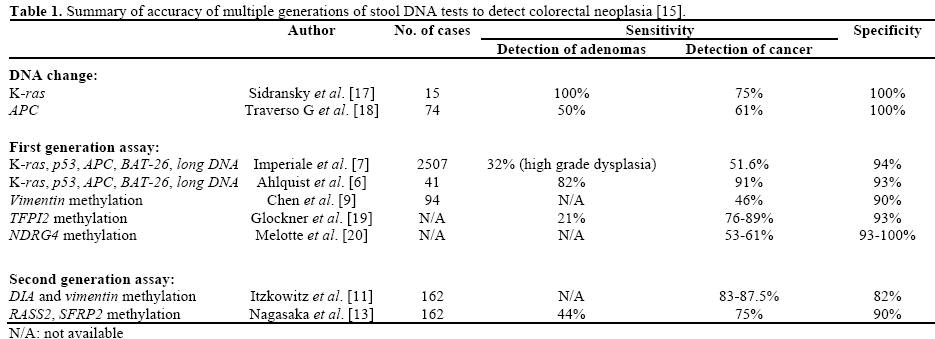
In Table 1, we summarize some of the currently available stool based testing strategies for colorectal cancer. The bulk of research work using fecal DNA has been done in this disease. Although the inclusion of gene methylation in the panel of stool based screening testing was pioneered by Chen et al. [9] with the inclusion of vimentin methylation, recent work by Nagasaka et al. [13] has utilized a two-gene, four promoter region CpG island based methylation assay to test detection of early gastric and colon neoplasia. In this work they showed that methylation of the RASSF2 and SFRP2 gene had comparable sensitivity and specificity as most prior combinations of stool DNA markers. The use of a one step method to isolate and bisulfite convert DNA and subsequently detect methylation after a fluorescence polymerase chain reaction (PCR), allowed improved yield and reduced time to perform the assays. This same group has now presented the results of an expanded 8-gene methylation based assay in the detection of pancreatic cancer. That pancreatic cancer derived DNA can be detected in stool (albeit with lower specificity then in colorectal or gastric cancer) has been demonstrated using the digital melt curve assay [8] but this is the first study to explore the performance of epigenetic changes in stool DNA [5]. The investigators have demonstrated that the expanded assay using methylation differences at 8 sites is capable of identifying not only advanced colorectal cancer or adenomas but pancreatic cancer as well. Further data and studies on the performance of this test and its ability to detect perhaps sub-clinical pancreatic cancer will be very valuable.
1H NMR–Based Metabolic Profiling of Serum for the Detection of Pancreatic Cancer (Abstract #193) [14]
Metabolomics combines advances in multivariate statistical analysis and improved ability to identify the metabolite panel of cellular change. Metabolites comprise the small molecules that are products or intermediates of processes such as protein and carbohydrate synthesis or degradation, gene expression regulation or cellular energy regulation [15]. Metabolomics investigates the change in metabolite levels that is associated with disease state. After the identification of metabolites associated with a disease state, further analysis is performed to validate the association between a particular metabolite signature and the condition tested. Such analysis of the cancer metabolome has shown the ability of metabolite signatures to identify cancer-associated signatures in adjacent normal breast tissue, prostatic fluid samples in prostate cancer and serum samples from individuals with ovarian cancer. A recent publication has shown that serum signatures may distinguish pancreatic malignancy from benign pancreatobiliary processes [16].
In the study by Bathe et al. [16] serum samples from individuals with pancreatic cancer were compared with serum of patients with benign pancreatobiliary processes. They adjusted for significant confounders such as concurrent diabetes, jaundice and were able to validate a metabolic profile with a significant the area under the ROC curve (AUC) of 0.8. The study by Owusu-Sarlfo et al. [14] chose to compare the metabolic profile of pancreatic cancer patients with healthy controls. This strategy most likely reduces the possible confounders associated with metabolically significant alterations noted in diabetes and jaundice. Multivariate logistic regression analysis was performed on a test sample set to identify the metabolite profile with the highest accuracy. When this was validated on a test sample set the sensitivity was 95%, the specificity was 100% and the AUC was greater than 0.98. This is the second study that confirms the role of metabolomics in pancreatic cancer and suggests that larger studies, perhaps concentrating on the ability to distinguish disease states such as chronic pancreatitis and pancreatic cancer, will be forthcoming.
Although biomarkers are not currently recommended for the screening of pancreatic cancer, discoveries in this field are likely to have the greatest immediate impact on pancreatic cancer mortality statistics. A screening test for the general population requires both high sensitivity and specificity. None of the previously tested markers (i.e., MUC1, CEACAM1, CK19 expression, K-ras and pancreatic juice methylation changes) have achieved this level of accuracy. However, it is likely that combination of these markers and fecal DNA changes or metabolomics hold that promise. The increasing accuracy of these markers suggests that in a research setting they may soon be incorporated into a prospective study to evaluate their performance in a higher then average risk population.
The authors have no potential conflict of interest