Original Article - (2020) Volume 21, Issue 4
Division of Gastroenterology and Hepatology, Loma Linda University Health, Loma Linda, CA, USA
Received Date: May 18th, 2020; Accepted Date: July 13th, 2020
Background The diagnostic yield of performing endoscopic ultrasound in hospitalized patients with acute pancreatitis is controversial. Aims To evaluate and compare the diagnostic yield, safety, and completeness of performing endoscopic ultrasound during or after hospitalization following acute pancreatitis. Methods Consecutive patients who underwent endoscopic ultrasound following an episode of acute pancreatitis (2007-20014) were searched from an internal endoscopy database. Endoscopic ultrasound findings and clinical course were reviewed. Telephone interview was conducted to verify the final etiology of acute pancreatitis. Results Of 61 patients (mean age=50 ± 19 years), 29 (48%) had focal pancreatic lesions identified on cross-sectional imaging. Mean days to EUS from presentation was reduced in 29 (47%) patients receiving endoscopic ultrasound during (9.0 ± 7.9 vs. 69.6 ± 75.5; mean difference=60.6 days, 95%CI 33.0-89.4) compared to 32 (53%) after hospitalization. Among patients receiving EUS during hospitalization, fine-needle aspiration was performed in 14 (50%) and a new cause was identified in 4 (14%) (Pancreatic adenocarcinoma in 3, choledocholithiasis in 1). No difference in diagnostic yield, proportion of incomplete procedure, or adverse events was observed among the groups receiving endoscopic ultrasound during or after hospitalization. During follow-up (4.6 ± 3.5 years), one patient was later diagnosed with pancreatic adenocarcinoma after receiving an incomplete endoscopic ultrasound during hospitalization. Conclusions In patients receiving endoscopic ultrasound following acute pancreatitis, nearly half had focal pancreatic lesions detected on cross-sectional imaging and tenth were diagnosed with pancreatic neoplasms. Endoscopic ultrasound performed during hospitalization led to a more rapid diagnosis, without difference in diagnostic yield or adverse events, compared to endoscopic ultrasound performed after hospitalization.
Endoscopic ultrasound; Acute Pancreatitis;Pancreatic cancer; Neoplasm
EUS Endoscopic ultrasound; BISAP Bedside Index of Severity in Acute Pancreatitis; CT Computed Tomography; MRI Magnetic resonance imaging; MRCP Magnetic resonance cholangiopancreatography; FNA Fine-Needle Aspiration; IPMN Intra- Ductal Papillary Mucinous Neoplasm
As high as a third of patients with acute pancreatitis do not have an identifiable cause after initial evaluation on history, physical examination, laboratory testing, and abdominal imaging [1]. Endoscopic ultrasound (EUS) provides high resolution imaging of the pancreatobilliary system, which is important for evaluating causes of acute pancreatitis, while maintaining a favorable safety profile [2, 3]. Society guidelines recommend EUS for patients >40 years of age with acute pancreatitis when standard evaluation does not reveal a definite etiology, given the possibility of occult pancreatic adenocarcinoma [4].
The timing of EUS in the setting of acute pancreatitis is controversial given concerns that inflammation from acute pancreatitis may lead to missed lesions and impact the safety of the procedure [2, 3]. In clinical practice, endoscopists commonly delay performing EUS for >4-8 weeks after a presentation of acute pancreatitis, based on expert opinion [2, 5, 6]. However, the disadvantages of delaying EUS include missed or delayed diagnosis of occult pancreaticobiliary tumors [3]. Limited studies demonstrate that EUS without fine-needle aspiration (FNA) in the setting of acute biliary pancreatitis can accurately evaluate choledocholithiasis without impacting safety [7, 8]. However, performing early EUS with FNA during hospitalization among patients with acute pancreatitis is currently not well described. The aim of the study is to evaluate the diagnostic yield, safety, and completeness of performing EUS in hospitalized patients with acute pancreatitis, compared to those who received EUS after hospitalization.
Study Design
The study was approved by the Institutional Review Board at Loma Linda University Medical Centre prior to initiating the study. Consecutive patients who received EUS for the primary indication of acute pancreatitis, between 2007 and 2014, were searched using the internal endoscopy database. The inclusion criteria consisted of patients who received diagnostic EUS during or following hospitalization for acute pancreatitis. Acute pancreatitis was defined by patients meeting at least 2 of the 3 criteria: characteristic abdominal pain; amylase or/and lipase elevated >3 times the upper limit of normal; and/or radiographic evidence of pancreatitis on cross-sectional imaging [9]. Patients who received EUS for drainage of pancreatic fluid collections were excluded. Furthermore, patients who were pregnant or age <18 years were also excluded. In patients who had multiple EUS performed during the study period, the initial procedure that met inclusion criteria was considered the index case. Patients’ medical records were reviewed to characterize the clinical course before and after EUS following acute pancreatitis.
The final cause of acute pancreatitis was determined based on consistent history, biochemical testing, abdominal imaging, and endoscopic ultrasound findings. Clinical outcomes were obtained by reviewing medical records including radiographic, endoscopic, surgical, and histologic report to characterize the clinical course and to establish the cause of acute pancreatitis. When possible, telephone consent and survey were conducted to clarify patient’s clinical status, recurrence of acute pancreatitis, and change in cause of acute pancreatitis.
Data Collection
Demographic data including sex, age, and race/ ethnicity were obtained. Furthermore, first or recurrent episodes of acute pancreatitis, smoking history, alcohol use, family history of pancreatitis, and weight loss in the last 6 months were recorded. Laboratory values including serum amylase, lipase, bilirubin and alkaline phosphatase levels at presentation of acute pancreatitis were recorded. Triglycerides, calcium, APACHEII score (age, vital signs, complete blood count, basic metabolic profile and Glasgow coma scale on admission) were also documented. All radiographic studies (ultrasound, computed tomography (CT), magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP) were reviewed. Focal solid lesion in the pancreas was defined by presence of a localized pancreatic or peri-pancreatic mass, prominence, fullness, or enlargement documented on ultrasound, CT, and/or MRI/MRCP. Focal cystic lesion in the pancreas was defined by presence of a localized pancreatic or peri-pancreatic cystic lesion documented on ultrasound, CT, and/or MRI/MRCP. The Bedside Index of Severity in Acute Pancreatitis (BISAP) score was calculated for each patient [10]. Furthermore, the severity of acute pancreatitis and presence of pancreatic and/or peri-pancreatic fluid collections were categorized according to the 2012 Atlanta Classification [11]. EUS findings were reviewed in detail, noting specifically for the presence of common bile duct stones/sludge, cystic and/ or solid mass, choledochal or pancreatic cysts, pancreatic divisum, and the overall pancreatic parenchyma, as well as, completeness of the examination. Chronic pancreatitis on EUS was categorized on the basis of the Rosemont criteria (consistent, suggestive, indeterminate, or normal) based on index EUS findings [12].
Study Endpoints
The primary endpoint of the study was the proportion of patients with a new cause of acute pancreatitis identified following EUS. New cause of acute pancreatitis was defined by typical EUS findings of microlithiasis, choledocholithiasis, pancreatic divisum, or a cystic/ solid pancreatic mass as documented by the endoscopist. Findings of chronic pancreatitis on EUS were not considered a cause of acute pancreatitis. Secondary endpoints were the proportion of patients with incomplete EUS examination, adverse events associated with EUS, and repeat EUS. An incomplete EUS examination was defined by failure to advance the echoendoscope to the ampulla and/or incomplete visualization of the pancreas.
Analysis
Descriptive statistics are reported as mean±standard deviation (SD) for continuous variables or as median and range otherwise. Comparison of proportional data between the study groups was performed using Chi-square or Fisher’s exact test where appropriate, and continuous data was compared using t-test. Two-sided p-values <0.05 were considered significant.
Patient Characteristics
During the study period, 61 patients received EUS following hospitalization for acute pancreatitis (Table 1). The mean age was 50.2±18.7 years, 30 (49%) were male, and 21 (34%) had a prior episode of acute pancreatitis. On presentation, the median BISAP score was 1 (range 0-4), and 38 (62%) patients had no definite etiology of acute pancreatitis after 47 (77%) receiving documented cross-sectional imaging with CT and/ or MRI/MRCP. Cross-sectional imaging studies revealed solid with or without cystic lesions in 12 (20%) patients and cystic lesions in 17 (28%) patients. Of the 23 (38%) patients with a possible cause of acute pancreatitis (alcohol in 12, gallstone in 5, hypertriglyceridemia in 3, medication-induced in 2, and ischemic in 1), 14 (61%) had solid and/or cystic lesions in the pancreas on cross-sectional imaging. Of the 38 patients without a cause of acute pancreatitis, 15 (39%) had solid and/or cystic lesions in the pancreas on cross-sectional imaging (Table 2).


Endoscopic Ultrasound Outcomes
Following acute pancreatitis, EUS was performed at a median of 23 days (range 1-438) from presentation including 29 (47%) during the index hospitalization and 32 (53%) after discharge. Eight (13%) patients received EUS<72 hours, 8 (13%) received EUS 3-7 days, 18 (30%) received EUS 7-28 days, and 27 (44%) received EUS>28 days from the onset of acute pancreatitis. Fifty-five (90%) of patients received EUS with moderate sedation and 23 (38%) received FNA.
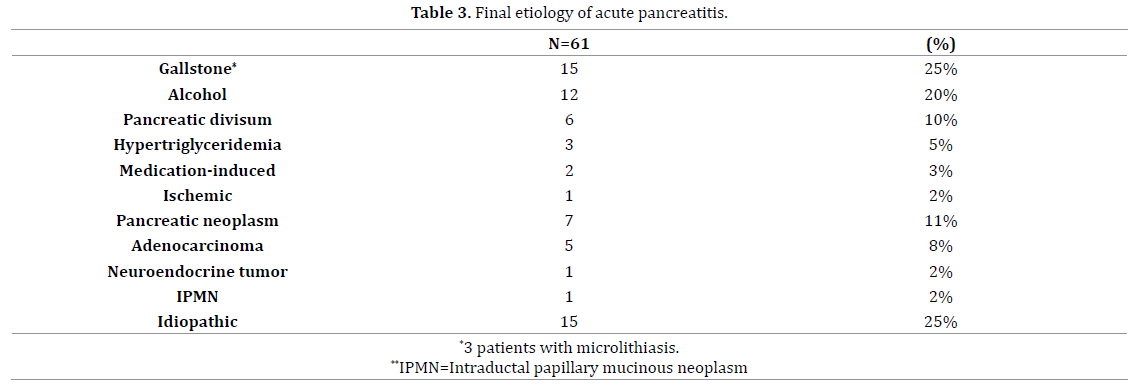
Following EUS, 15 (24%) patients received a new diagnosis (Table 3) including 6 (10%) with pancreatic neoplasm (adenocarcinoma in 4, neuroendocrine tumour in 1, intra-ductal papillary mucinous neoplasm (IPMN) in 1) and 9 (14%) with benign etiologies (pancreatic divisum in 6, microlithiasis/choledocholithiasis in 3). Furthermore of the 28 patients with solid with or without cystic pancreatic lesions (N=11) or cystic pancreatic lesions (N=17) on cross-sectional imaging, 3 (10%) were diagnosed with pancreatic neoplasms (pancreatic adenocarcinoma in 1, pancreatic neuroendocrine tumour in 1, and IPMN in 1). Four (7%) patients, including 3 receiving moderate sedation and 1 receiving anaesthesia assistance, had incomplete EUS examinations (difficulty with sedation in 2, inability to intubate the second portion of the duodenum in 1, altered anatomy in 1). No adverse events related to the EUS were documented. Subsequently, 9 (7%) received repeat EUS at median of 21 days (range 1-1,078 days) from the initial examination without a change or new diagnosis in any of the patients.
Clinical Outcomes
During mean follow up of 3.7±3.5 years, one patient who received EUS during hospitalization had a change in diagnosis (pancreatic adenocarcinoma). Furthermore, 3 (5%) patients including 2 who received EUS during and 1 after hospitalization developed recurrent acute pancreatitis
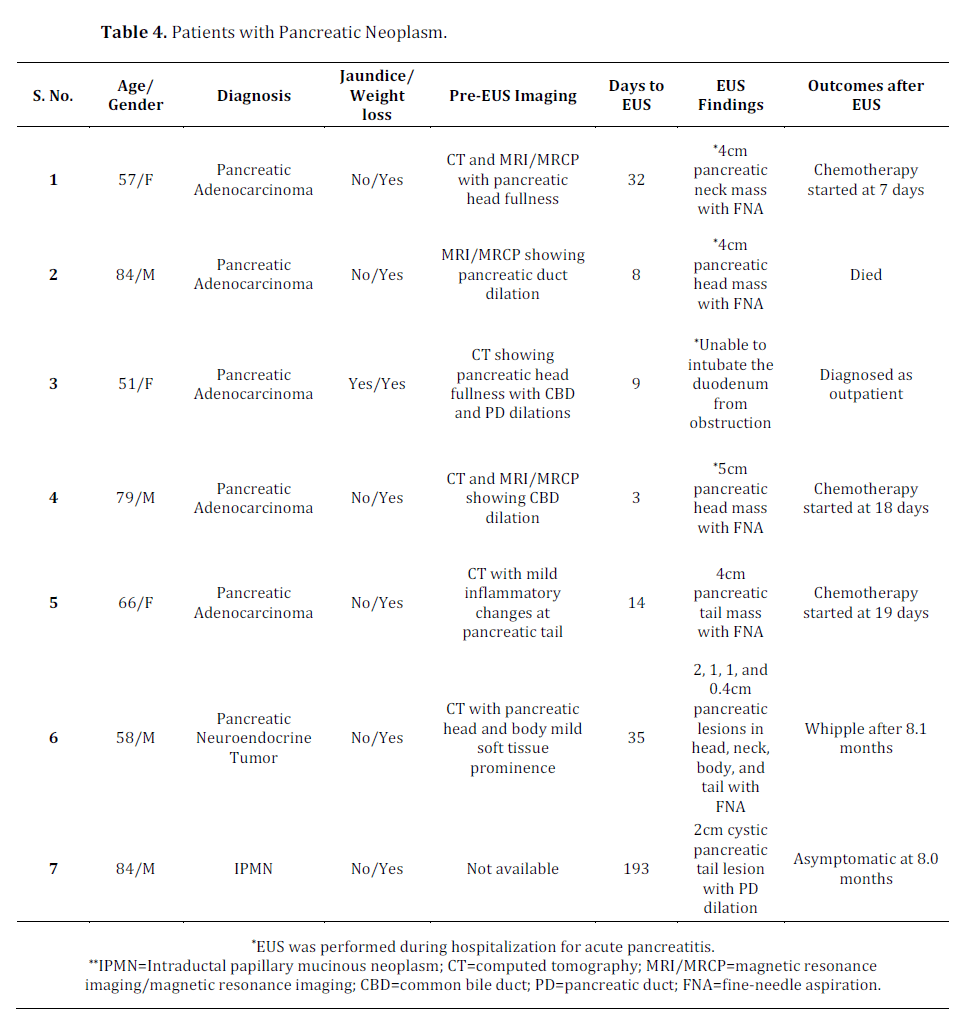
Diagnosis of Pancreatic Neoplasm
Among the 7 patients diagnosed with pancreatic neoplasm, 6 were diagnosed at the time of EUS. However, one patient was later diagnosed with pancreatic adenocarcinoma after receiving an incomplete EUS examination performed during the hospitalization for acute pancreatitis. Of the 5 patients diagnosed with pancreatic adenocarcinoma, 3 received chemotherapy for pancreatic adenocarcinoma 1 died, and 1 was lost to follow-up. One patient received curative resection for pancreatic neuroendocrine tumour (Table 4).
In a single centre study of 61 hospitalized patients with acute pancreatitis, 38 (62%) did not have a cause of acute pancreatitis and 29 (48%) had focal pancreatic lesions identified on cross-sectional imaging prior to receiving EUS. EUS was performed at a mean of 2 months earlier (mean difference=61.2 days, 95%CI 33.0-89.4) during hospitalization in 29 (47%) compared to 32 (53%) patients who underwent EUS after hospitalization. Of the patients receiving EUS during hospitalization, FNA was performed in 14 (50%) and a new cause of acute pancreatitis was identified in 4 (pancreatic adenocarcinoma in 3, choledocholithiasis in 1). No difference in diagnostic yield, proportion of incomplete procedure, or adverse events was observed among patients receiving EUS during or after hospitalization. Among patients who received EUS during hospitalization, 2 (7%) developed recurrent acute pancreatitis, and one was later diagnosed with pancreatic adenocarcinoma after an incomplete index exam.
American Society for Gastrointestinal Endoscopy guidelines recommend EUS for evaluation of idiopathic acute pancreatitis in patients >40 years of age when clinical symptoms, biochemical testing, and crosssectional abdominal imaging are unrevealing [4]. The recommendation is based on the rationale that 20% of such patients will develop recurrent acute pancreatitis, and clarifying the etiology may potentially prevent a future attack [1]. Furthermore, acute pancreatitis is the initial presentation in 5% of patients with pancreatic adenocarcinoma, associated with a small window of opportunity for curative resection [13]. In a systematic review, EUS identified a cause or associated pathology in 1,096 (62%) of 1,850 patients with idiopathic acute pancreatitis [14]. Furthermore, EUS demonstrated higher diagnostic accuracy (64% vs. 34%, P<0.001) compared to MRCP in a systematic review of 477 patients with idiopathic acute pancreatitis [15]. Although the diagnostic yield is high, the optimal timing to perform EUS in the setting of acute pancreatitis remains unclear. During the acute phase of acute pancreatitis, anatomic derangements including duodenal wall edema, peri-pancreatic fluid collections, or pancreatic necrosis may interfere with deep duodenal intubation of the echoendoscope, precluding complete visualization of the pancreas or the bile duct. Furthermore, diffuse hypoechoic changes from edematous pancreatic parenchyma may obscure visualization of pancreatic duct changes or occult lesions [6]. Finally, performing a EUS prior to clinical resolution of acute pancreatitis in patients who are generally treated with potent analgesics, may impact the ability to achieve adequate sedation or increase the risk of adverse events. Subsequently, some experts have advocated delaying EUS for >4-8 weeks after presentation of acute pancreatitis [2, 5, 6]
In our study, EUS was performed relatively early at a median of 23 days from presentation in patients with mostly mild pancreatitis (median BISAP=1). Focal pancreatic lesions were observed in a high proportion of patients on cross-sectional imaging likely given typical findings associated with acute pancreatitis and high prevalence of chronic pancreatitis (consistent or suggestive of chronic pancreatitis in 12 (20%)) in this population. Performing EUS identified a new cause in 15 (24%) of 61 patients including 6 (10%) with pancreatic neoplasm. More importantly, the diagnostic yield, proportion with incomplete procedures, or need for repeat procedure was similar between patients who received EUS during and after hospitalization. Furthermore, no procedure-related adverse events were documented despite half the patients receiving EUS with FNA during hospitalization for acute pancreatitis. However, EUS failed to diagnose pancreatic adenocarcinoma in one patient after an incomplete procedure due to duodenal obstruction. Interestingly, prior cross-sectional imaging with CT and/or MRI failed to demonstrate an obvious mass in all patients with pancreatic neoplasm, although non-specific changes were commonly observed (pancreatic head fullness in 2, bile duct changes in 2, pancreatic duct changes in 2, and pancreatic head soft tissue prominence in 1). In a study of 107 patients receiving EUS for non-specific abnormalities of the pancreas on CT (i.e. enlarged pancreas, fullness of the pancreas, abnormal pancreas, prominent pancreas, or ill-defined pancreas), 29 (27%) were diagnosed with pancreatic neoplasm, including 22 (21%) with pancreatic adenocarcinoma [14, 15, 16].
Previous studies examined variable time to performing EUS in patients with acute pancreatitis. In a prospective study of 71 patients with acute biliary pancreatitis, EUS performed <48 hours from presentation identified choledocholithiasis in 31 (44%) with complete evaluation in all patients [17]. However, the study excluded 110 patients with severe acute pancreatitis, concurrent cholangitis, clinical instability, or other possible causes of acute pancreatitis including 5 (3%) with pancreatic neoplasm. In another prospective study of 65 patients, EUS performed <48 hours from the time of hospitalization for acute pancreatitis following a negative CT, demonstrated choledocholithiasis in 23 (35%) patients and pancreatic adenocarcinoma in one (2%) [7]. In 31 patients receiving EUS performed >2-3 weeks after hospitalization, 8 (26%) received a new diagnosis including 1 (3%) with pancreatic adenocarcinoma [17]. In 370 patients with acute pancreatitis receiving EUS>4 weeks after hospitalization, 108 (29%) had a new diagnosis including 3 (1%) with pancreatic neoplasm [18]. In a prospective study of 201 patients with acute pancreatitis, EUS performed >1 month from hospitalization demonstrated a cause in 90 (45%) but none with pancreatic neoplasm [5]. Furthermore, recurrent acute pancreatitis occurred in 46 (33%) of 139 and 17 (28%) of 60 patients with or without a cause identified on EUS [5]. Finally in a study of 40 patients who received EUS >1 month after the episode of acute pancreatitis without abdominal pain, a biliary source was identified in 20 (50%) patients and one (3%) with occult pancreatic neoplasm [19]. Our study demonstrated the highest reported prevalence of pancreatic neoplasm as a cause of acute pancreatitis of 11% compared to other studies (0-3%), which is likely reflective of institutional EUS practice patterns and analysing unselected patients who received EUS regardless of hospitalization status [5, 17, 18, 19, 20]
Our findings have clinical implications. In patients receiving EUS after acute pancreatitis, nearly half the patients had focal pancreatic lesions and more than a tenth were found to have a time-sensitive diagnosis, including pancreatic adenocarcinoma. Cross-sectional imaging in this population may commonly identify benign focal lesions that raise concerns for malignancy but also fail to identify occult pancreatic neoplasm as a cause of acute pancreatitis. Furthermore, an incomplete procedure was infrequent, while procedure-related adverse events were not documented in patients who received EUS during hospitalization for acute pancreatitis. Therefore, performing EUS during the hospitalization may lead to rapid diagnosis and reduce the risk of lost to follow-up in patients with potential diagnosis of pancreatic neoplasm. Finally, one patient with pancreatic adenocarcinoma was missed after having an incomplete EUS examination. If the index EUS is non-diagnostic or incomplete, a repeat EUS should be performed as soon as possible in patients with high suspicion for pancreatic neoplasm based on clinical features (i.e. jaundice or weight loss) or radiographic findings (e.g. presence of focal lesions or changes in bile or pancreatic duct).
There are several limitations of our study. Given the retrospective study design, patients selected to receive EUS in our study are likely reflective of local physician and institutional practice patterns, and the results may be less generalizable to other settings. For example, a proportion of patients in our study with a possible cause of acute pancreatitis after standard evaluation received EUS given suspicion for alternative cause of acute pancreatitis, inability to receive contrast-enhanced cross-sectional imaging, or follow-up evaluation for abnormal findings detected on cross-sectional imaging. Furthermore, despite telephone follow-up, complete follow-up was not available in all the patients.
In summary, nearly half the patients with acute pancreatitis had focal pancreatic lesions detected on cross-sectional imaging and a tenth were diagnosed with pancreatic neoplasms. EUS performed in acute pancreatitis during hospitalization led to a more rapid diagnosis of pancreatic neoplasm without differences in diagnostic yield compared to those performed after hospitalization. Incomplete procedures were infrequent, and procedural complications were not observed. In patients with acute pancreatitis with high suspicion for underlying neoplasm, EUS performed during the hospitalization may lead to a more rapid diagnosis, without increased risk of adverse events.
No competing or conflicting interests to declare.