- (2006) Volume 7, Issue 6
Kevin J Koomalsingh, Rafael Fazylov, Mitchell I Chorost, Joel Horovitz
Department of Surgery, Maimonides Medical Center. Brooklyn, NY, USA
Received: 24 July 2006 Accepted: 24 August 2006
Context Congenital cystic lesions of the pancreas are rare findings. Furthermore, a dermoid cyst of the pancreas is exceptionally uncommon. A review of the world literature shows 18 documented cases. The preoperative evaluation of this lesion is rather questionable, with definitive diagnosis taking place intra-operatively.Case report A 52-year-old male with a symptomatic, 3-cm cystic-type mass in the pancreas.Conclusions From our case presentation and review of the world literature, we hope to establish an increased awareness in the diagnostic evaluation of these patients.
Dermoid Cyst; Pancreas; Teratoma
Teratomas can be divided into two subtypes, mature and immature. The mature type can be further subdivided into a solid type and a cystic type, hence dermoid cyst. A review of the English literature has identified about twenty cases limited to the pancreas, the rarest site. Derived from totipotent stem cells, they possess the ability to generate tissues from all three germ layers: endodermal, mesodermal and ectodermal. We present our case and review the literature, in an attempt to increase awareness for the preoperative detection of these rare tumors.
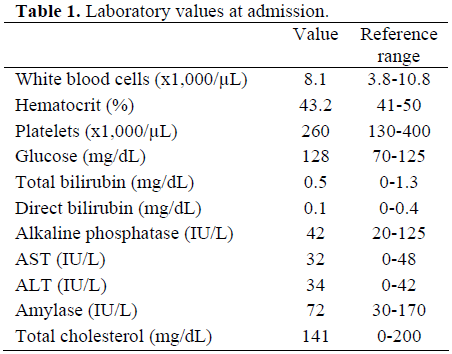
A fifty-two-year-old male with past medical history of non-insulin dependent diabetes mellitus and hypertension, presented with nonspecific epigastric pain for several weeks. Review of systems was otherwise negative. Physical exam revealed mild epigastric tenderness. Laboratory studies were essentially normal (Table 1), likewise an abdominal X-ray. Further evaluation was undertaken. Computed tomography (CT) imaging of the abdomen demonstrated a 3.5x3.0 cm soft tissue mass arising from the distal portion of the pancreas with possible extension to the posterior stomach (Figure 1). Its exact origin though could not be clearly defined. Esophagogastroduodenoscopy demonstrated mild gastritis and endoscopic ultrasound confirmed a cystic lesion arising from the pancreatic tail measuring 2.2x3.2 cm. No septations, vascular invasion or solid components were identified but the lesion did exhibit a non-homogenous appearance (Figure 2). Again, the margins could not be clearly identified. Our patient consented to a distal pancreatectomy, with possible splenectomy. Intraoperatively, a cystic lesion was palpated arising from the tail of the pancreas without any infiltration into the surrounding tissues. The lesion was intrapancreatic. Its borders were well defined and the mass contained predominantly sebaceous material. Frozen section identified the specimen as a cystic teratoma. A simple cystectomy was performed, without any compromise to the surrounding pancreatic parenchyma. Pathological evaluation revealed a benign teratoma (dermoid cyst). Histologically, the mass contained stratified squamous epithelium and skin appendages, surrounded by a wall composed of abundant lymphoid tissue. Our patient had an uneventful postoperative stay and was discharged home on post-op day three. Laboratory values prior to discharge were again normal. At 16-month follow-up, our patient has been asymptomatic, without any evidence of recurrence.
Dermoid cysts are thought to arise from the embryonic inclusion of skin, at the time of neural groove closure [1], therefore, typically found lying along the midline. Most commonly located in the ovaries, they have been found at several extragonadal sites, the pancreas being most rare.
Surrounding the lesion is the cyst wall, which may contain adnexal tissue, sebaceous glands, lymphoid tissue and even inflammatory cells. Beneath this surface, lies a single layer of keratinizing squamous epithelium [1]. The inner compartment, often filled with thick, pasty, doughy sebaceous secretions, contains fully differentiated tissue(s) from one or more germ cell layers, most commonly ectodermal. Amongst the list of differentials includes pseudocyst and neoplastic cysts, including both benign and malignant lesions. As stated by Brugge et al., the clinical challenge rests in distinguishing the more common benign cystic lesions from their rarer, malignant counterparts [2]. Our clinical concern, therefore, was ruling out a malignant process. Though benign, dermoid cysts prove clinically and radiologically challenging in differentiation from the more concerning lesions, but once identified can be treated appropriately.
Akin to most pancreatic cystic lesions, their clinical presentation is nonspecific. The symptomatology has ranged from an asymptomatic palpable mass to obstructive jaundice with liver failure. Most patients though, present with varying severity of abdominal pain, back pain, vomiting or jaundice.
Laboratory values will likely be normal unless an obstructive pattern to the normal drainage of biliary or pancreatic secretions exists. Unlike dermoid cysts elsewhere in the body, little radiographic evidence is available regarding their pancreatic location. However, extrapolating the documented findings to the pancreas, it appears equally so that the radiologic appearance of these lesions depends on the proportions of the various tissues of which they are composed [3]. Ultrasound will initially define the mass as cystic, without septations and with distinct margins. The fatty component would be expected to appear hyperechoic with focal areas of high-intensity signals plus acoustic shadowing, secondary to the presence of calcified tissues [3]. CT will confirm these areas of calcifications and fat and characterize the fluid as sebum, serous or complex [3]. Magnetic resonance imaging (MRI) can also be performed for further characterization. We did not proceed with MRI. But expected findings may include: low signal intensity on T1-weighted images [3], areas of fat-fluid level, if present, and distinct margins.
At this point an excisional biopsy is usually performed with the possibility of a more extended resection, if warranted. However, the prospect of cytologic diagnosis should not be overlooked. In 1991, Markovsky et al. [4] described the findings of the first reported preoperatively diagnosed cystic teratoma by fine needle aspiration. Cytological findings included mature benign squamous cells, keratin debris and inflammatory cells (the three predominant cell types, also found in ovarian dermoid cyst). Furthermore, Markovsky et al. illustrated that such histological findings are inconsistent with other pancreatic disorders as pseudocyst, pancreatitis and degenerated carcinomas for their lack of specific histological elements. Despite our failure to perform an FNA, we do believe in its selective utility in asymptomatic patients and patients considered high-risk surgical candidates. If a differential diagnosis for a cystic lesion in the pancreas has been assimilated and radiologic evidence is inconclusive but consistent with the features illustrated above, a fine needle aspiration for cytologic analysis can confirm the diagnosis pre-operatively.
Treatment has been surgical. Observation has not been reported. Can these lesions be observed? With a high enough pre-test probability (based on cross sectional imaging studies and cytology findings consistent with dermoid cyst) these lesions can be safely observed. For the eighteen reported cases though, surgical procedures included simple cystectomy (9 patients, 50%), external drainage procedures (5 patients, 20%), distal pancreatectomy (1 patient, 6%), distal pancreatectomy plus splenectomy (1 patient, 6%), cystogastrostomy (1 patient, 6%), and one case unreported (6%). The trend over the years has steered away from external drainage procedures. They are not recommended because complete healing is unlikely, as the retained elements contain secretory epithelium and thus the possibility of recurrence or fistula formation is increased [5]. In addition, the long-term sequela of internal drainage is unknown as the one patient who received a cystogastrostomy was lost to follow-up. Partial pancreatectomy with splenectomy is unnecessary, as avoided in our patient. The mainstay of surgical therapy therefore, is simple cystectomy, unless otherwise indicated.
Given the list of differentials and the high incidence of patients presenting with radiologically detected pancreatic cystic lesions, how does one identify a benign process as a dermoid cyst from something potentially pre-malignant or even frankly malignant? The answer is a difficult one, as evident by the literature concerning the management of pancreatic cystic lesions. The nonoperative criteria proposed by Allen et al. [6] were reviewed, but since our patient was symptomatic, he required operative intervention. Our recommendation therefore is to maintain a high degree of clinical suspicion. With a closer analysis of the cross sectional imaging studies, looking for areas of fat attenuation and calcifications along with an FNA biopsy sample in an asymptomatic or high-risk surgical patient, results consistent with the findings of Markovsky et al. [4], we may be able to preoperatively diagnose these rare but benign lesions and even observe the asymptomatic cases.