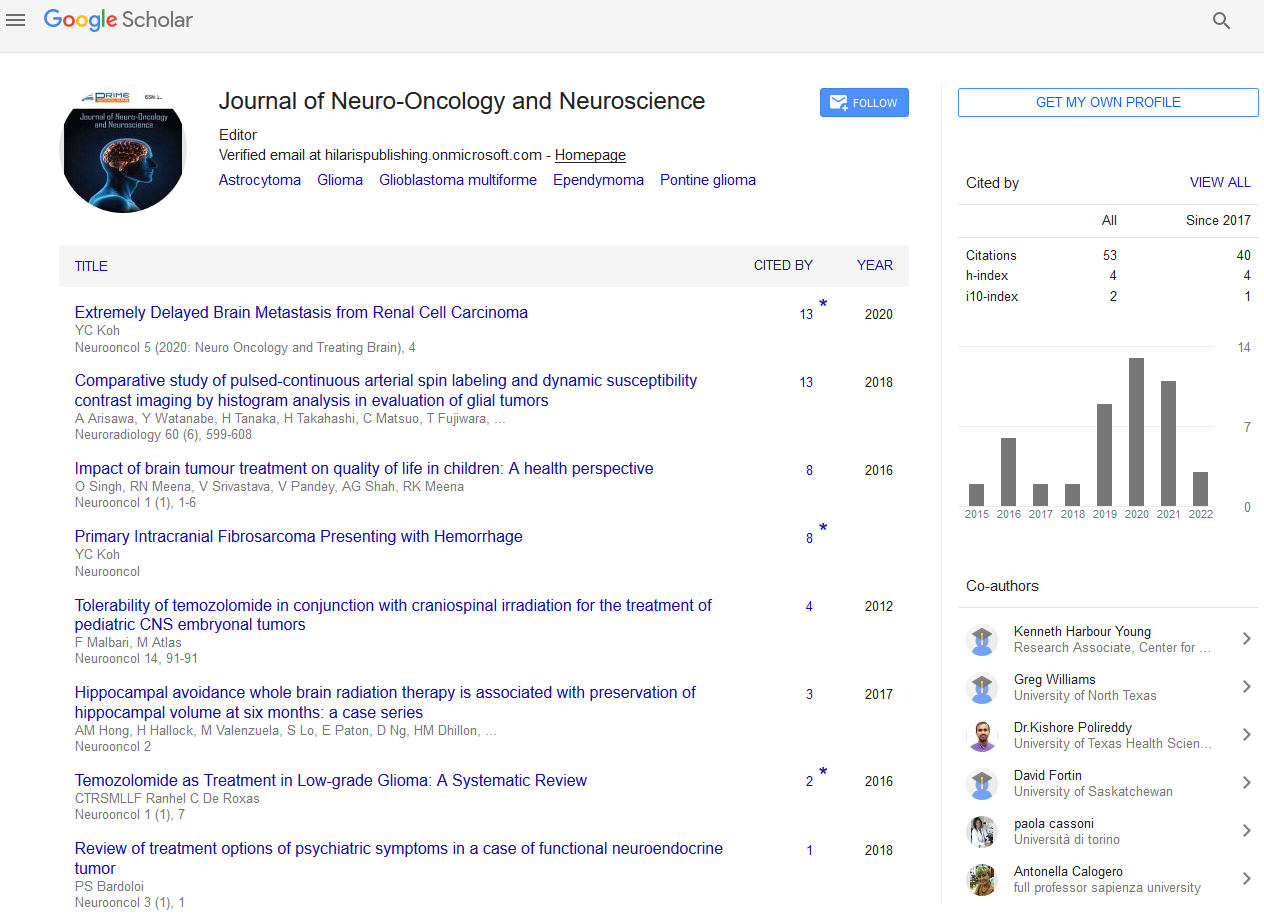
Research Article - (2022) Volume 7, Issue 5
Culture Insights of Cellular Mechanisms of Glioblastomas Growth
Valerii Matcovschii1,
Valentin Gudumac2,
Dan Lisii1* and
Lilia Andronache2
1Department of Neurosurgery, Institute of Neurology and Neurosurgery, Moldova
2Department of Biochemistry, Nicolae Testemi?anu State University of Medicine and Pharmacy, Moldova
*Correspondence:
Dan Lisii,
Department of Neurosurgery, Institute of Neurology and Neurosurgery,
Moldova,
Email:
Received: 31-Aug-2022, Manuscript No. IPJNO-22-14539;
Editor assigned: 02-Sep-2022, Pre QC No. IPJNO-22-14539 (PQ);
Reviewed: 16-Sep-2022, QC No. IPJNO-22-14539;
Revised: 21-Sep-2022, Manuscript No. IPJNO-22-14539 (R);
Published:
28-Sep-2022, DOI: 10.21767/2572-0376.22.7.52
Abstract
At present, glioblastomas of the brain are incurable tumours and the new developments of clinical neurosurgery, radiation therapy and chemotherapy do not solve the issue. Studying the cellular and subcellular growth mechanisms of the initial glioblastoma cells taken from tumours during neurosurgery and cultivating said cells for 3-6 months, allows us to put forward a relatively new hypothesis about the amitotic division of the glioblastoma cells. It is important to note that the tumour growth occurs via the transfection and expression of fragments of proteins and nucleic acids produced by the glioblastomas into the healthy contractile glial cells. This hypothesis is indirectly confirmed by conducing experimental studies with the introduction into the cell culture of polymerase, adenovirus of the AstraZeneca vaccine, as well the visual data obtain during magnetic resonance imaging (MRI) to observe the dynamic and character of the growth of glioblastomas in the brain.
Keywords
Glial cell; Glioblastoma; Mitosis; DNA; mRNA; Transfection; Biochemical resonance; PCR; MRI; Infiltrative
growth of glioblastoma.
Introduction
Glioblastomas of the brain are incurable tumours with a one
hundred % mortality rate within 1.5 years-2 years after the full
macroscopic removal by using all of the modern techniques,
alongside with radio and chemotherapy. When talking about
a partial tumour removal, this period is reduced to one year
[1-3].
One of the reasons of such modest success over the course of
decades is the incomplete understanding of the cellular mechanism
of growth of glioblastomas. It’s commonly assumed that
the malignancy of tumours is determined by acceleration of
the cell division rates. Moreover, the root cause of the genetically
modified clone is a single cell that is continuously dividing,
resulting in a tumour [4]. This is caused by various DNA defects
remaining unrepaired when the cell enters the next cycle of the
G1-G2-M division; meaning that at key phases (check points),
G1/S the integrity of the DNA double helix are not checked.
When the correctness of the DNA replication is not checked at the G2/M point and finally at the M point, the proper attachment
of the spindle to kinetochores and centromeres is also
not verified.
The fact of cells going through these checkpoints without undergoing
DNA repairs is caused by the deactivation of suppressor
genes, such as P53 and RS1, as well as the activation of
proto-oncogenes; leading to the accumulation of gene mutations
without triggering apoptosis and stimulation of the rate
and number of mitoses [5]. Both of these processes result in a
malignant transformation of cells. Epigenetic factors, particularly
the hypo–methylation of the DNA cancer cells, enrich the
more modern concepts of oncogenesis. Alongside mitosis the
hyper-methylation of individual suppressor genes will sharply
reduce the control on having artefact–free DNA and encourage
the accumulation of mutations [6,7].
There are multiple studies dedicated to the polyploidy and
the amitotic cell division during the process of carcinogenesis.
Given the unstable nature and genetic variability, polyploidy is viewed as a characteristic feature of cancer [8]. Certain metabolic
aspects of aneuploidy clearly contribute to the resistance
and recurrence of tumors with a high degree of malignancy
[9-11]. Cells that divide amitotically are not highly clonogenic;
however, the giant polyploidy cells have a high survivability rate
and are typical not only for the late stages of cancer but can also
be seen during the precancerous stage, a fact which suggests
the possibility of them having another metabolic role besides
genetic selection [12-14] Given that, one must evaluate the amitosis
as an important prognostic and curative factor [15,16].
On a system level, the insufficient limitation of the intensive proliferation
of malignant cells is caused by the failure of humoral
and cellular mechanisms of immunity. It is considered that the
membrane of the cancer cell carries very few antigen bodies
that are foreign to the human organism and since usually they
are monovalent, they trigger a wear precipitation reaction with
the immunoglobulins that are produced by B lymphocytes, as
well as a weak cytotoxic reaction of T lymphocytes.
Our experimental studies on the long term in vitro cultivation
of glioblastomas combined with an analysis of MRI imaging of
the cells and their intraoperative morphology allow us to propose
a hypothesis of a non-mitotic division of glioblastoma cells
and an increase in tumour volume caused by the transfection of
healthy glial cells with glioblasts.
Methods and Materials
Small glioblastoma fragments around 5-6 cm3 in volume, taken
directly during the tumour removal, were placed in sterile dishes
filled with 20 ml of the patient’s own plasma. No less than six
hours later, the tumour tissue would be grinded and dispersed
by filtering through sieves with a mesh size from 1.5 mm to 0.5
mm. This was then planted in sterile flasks filled with DMEM
medium with a high glucose concentration (4.5 grams per litre)
and an added 20% of a serum obtained from the patient’s blood
and fluconazole (100 milligrams per litre). The culture was then
placed in a CO2 incubator in which the following conditions
were maintained: A temperature of 37°, a CO2 concentration of 3.5% and a humidity of 95%. Over a period of three weeks,
the culture would be re-suspended and re-centrifuged. On the
fourth week the amount of cells would be sufficient to allow
checking their individual sensitivity to various chemotherapy
drugs, the cell tropism of lymphocytes to glioblastoma cells as
well as allowing video monitoring of globalists’ division. In the
search for the growth factors of glioblastomas after two/three
months of cell cultivation, repeated removal form the culture
media and for overcoming the crisis of cell division in every
15 ml. of the culture media a DNA polymerase I (20 to 40 UA
activity units) and 70 microgram of all 4 deoxyribonucleotides
was added. In addition, in order to evaluate the growth of glioblastoma
cells in the presence of a recombinant vaccine, 0.1
ml of standard Oxford/AstraZeneca (ChAdOx1-S [recombinant]
vaccine) COVID-19 vaccine was supplemented to each 15 ml of
culture media.
Results
Our research on the cultivation and monitoring of primary glioblastoma
cultures obtained from post-operative patients, over
a period of three-six months, allows us to state that the first
two weeks of incubation, the cellular make-up of the culture is
made up by glioblastoma cells that are round in shape, have a
diameter of 20 mm-30 mm and have intensely hyper chromic
nuclei (×200) (Figure 1a).

Figure 1: The dynamic of hyper chromic glioblast cell cultivation (X200). (a) hyper chromic glioblastoma cells in suspension, (b) the initial stages
of the monolayer of hyper chromic glioblasts, (c) the stage of the subtotal filling of the monolayer of hyper chromic glioblasts, (d) the death phase
of the hyper chromic glioblasts - karyorrhexis and karyopyknosis.
The vast majority of these cells have a significant higher mass
than the medium in which they are placed and they settle on
the bottom of the dish, where they spread out in a fibrous like
fashion (Figure 1b). Prolonged observation of the steady increase
in number of these cells gown in a monolayer allows us
to conclude that the cells that have condensed nuclei spread out
evenly, reaching the shape of an irregular oval elongated along
one axis. Once they reach the bottom of the dish, they clump
into clearly separated cell formations, which do not move (Figure
1c). These cells are not capable to undergo multiple rounds
of mitosis in the medium and within three-four months of cultivation,
they die due to karyorrhexis and karyopyknosis, leaving
behind but a shadow (Figure 1d).
That division capacity is retained by a very small number of cells
(in the single digits percentage wise from the full sample), characterized
by a transparent cytoplasm and increased volume.
They can be seen clearly see only on the 4th-8th week of cultivation,
when the medium is less cloudy. Toward the 4th-8th month
of cultivation, these cells make-up the majority of the cell population
(Figures 2a and 2b).

Figure 2: The dynamic of cultivation of glioblastomas with a transparent cytoplasm. (a) single cell with a transparent cytoplasm – 1-2 months within
cultivation, (b) multiple cells with transparent cytoplasm – 4-6 months within cultivation.
Their cytoplasm remains relatively transparent, there aren’t any
nuclei, there are no condensed chromosomes and often, there
isn’t even a state of hyper chromium cytoplasm. If the culture
medium contains a serum concentration of 20%-30%, then the
glioblasts don’t migrate to the bottom and get cultivated in
suspension while retaining their round shape (Figures 3a and 3b). The process of a new cell creation is more reminiscent of
gemmation and can be recorded as it happens via video monitoring
under the microscope. In the meanwhile the cells that
have a transparent cytoplasm one can observe movement of
that cytoplasm without any nucleus edges, which suggests the
movement of the replicated DNA and protein in the synthetic
phase of the interphase. This seemingly chaotic movement is
quite intense and the outside cellular membrane is constantly
changing shape and creating cytoplasmic peaks, which appear/
disappear at various times (Figures 4a-4d).

Figure 3: A culture of metastasized lung adenocarcinoma cells in the brain. (a) The mitotic division of the adenocarcinoma in the monolayer observed
under the microscope in a bright field, (b) The mitotic division of the adenocarcinoma – phased contrast microscopy (the mitoses are indicated with
arrows)under.

Figure 4: The process of cytoplasm’s active movement with protrusions of the outer membrane and the gemmation of the daughter glioblast cell.
(a-c) the circular motion of the protruding membrane of the glioblastoma cell, (d) The formation and sub-total division of the mother-daughter glioblastoma
cell.
Within a couple of minutes, we can observe one-two protrusions
on the membrane, which are increasing to a size that is
comparable to the mother’s cell. After that, this protrusion is
pulled to a point that there is only a narrow attachment between
this pseudo cell and the original one. In the process
of lacing, you can see how the contents of the cytoplasm are
chaotically transferred from the mother to the daughter’s cell.
Upon continuous observation of the gemmation process one
can clearly see that there isn’t any mitosis but rather the contents
of the mother’s cytoplasm are haphazardly transferred
into the daughter’s cell, creating a multi-cell conglomerate (Figures
5a-5d).

Figure 5: Variants of glioblastomas’ division via gemmation. (a) Subtotal separation of the daughter’s cell from the mother’s, (b) Multiple buds with
total and subtotal separation of the mother/daughter cells, (c) Gemmation with complete separation of the daughter cells, (d) Gemmation without a
complete separation of cells, resulting in “monster” cells.
A fraction of the cells with this transparent cytoplast spread
quite significantly, resulting in the creation of spindles. It is important
to note that one cellular spindle is continued by another
one and collectively they form long chains where you can’t
really see the membranes that separate one spindle from the
other (Figure 6). In essence, the sequential nature of these spindles
mirrors the aforementioned gemmation of daughter cells
from one mother cells, same are cultivation in suspension; however
as the third coordinate of the cell freedom is missing, i.e.
the fixation at the bottom of the dish, these spindles is formed
instead. The contents of the cytoplasm of the daughter cells is
transferred just as haphazardly from one cell to the other, without
any indication of chromosome condensation, typical for mitosis.

Figure 6: The creation of spindles of glioblasts in the monolayer. (a) Beginning stage of the formation of the glioblast spindles’ grid in the monolayer,
(b) Subtotal filling of the glioblast spindles’ grid in the monolayer.
A clear confirmation of the gemmation process in the monolayer
is the trypsinization of glioblasts, during which the process of
cell separation from the bottom of the dish is accompanied by
dragging several other cells via a thin continuous membrane,
one after the other. During a complete separation from the
bottom of such cells and their transition to a suspended state, daughter cell groups are formed, with a high number of bulbous protrusions (Figures 7a-7d).

Figure 7: Trypsinization of the monolayer of glioblasts. (a) Subtotal monolayer of glioblatst prior to trypsinization, (b) The beginning of the separation
of the layer from the bottom of the dish with the formation of daughter cells, (c) Subsequent separation and rounding of cell groups, (d)
Complete separation of a group of cells with their transition into suspension.
Taking that into consideration, when primary glioblastoma cells
are being cultivated in suspension or in a monolayer, it’s practically
impossible to observe a mitotic cell division with hyperchromic
condenced nuclei. Those cells are present at the beginning
stages of incubation in the absolute majority of cases;
however towards the 3rd-4th month of the process almost all of
those cells die. In contrast, the cells that have a decondenced
and potentially replicated DNA, and are present in very small
numbers at the beginning, make up the majority of the population
at the later stages of incubation. Nevertheless, in the process
of sifting the culture, if the cells are not frozen during the
preliminary division stages to pseudo-immortalize the culture;
the cell mass is constantly declining and ultimately all of the
cells are dead by the 4th-6th month.
At the later stages of the incubation, the cell population is almost
exclusively made up by the cells with a transparent cytoplasm
and the transformation process gets triggered, resulting
in an increase in cells’ volume, a significant shape distortion and
the appration of “monster” cells (Figure 8)

Figure 8: “Monster” cells – late incubation stages.
Adding into this environment of the culture media with a DNA
polymerase I (20 to 40 UA activity units) and 70 microgram of
all 4 deoxyribonucleotides contributed to the cell gemmation
process in a drastic fashion, as well as increasing in their size.
These “monster” cells have a linear size between 40-100 micro
meters and they become a key component of the entire cell
mass. There are multiple inclusions that are visible in the cell’s
cytoplasm as well as multiple barriers. Besides that, we can observe
the emergence of small (7-10 micro meters in diameter),
oval cells with transparent cytoplasm, that following multiple gemmations become similar to bunches of grapes (Figure 9)

Figure 9: The introduction of polymerase 1 into a glioblastoma culture. (a) Significant increase of the number of glioblasts under the influence of
polymerase 1, (b) The emergence of a large number of “monster” cells under the influence of polymerase 1, (c) The emergnece of colonies of small
cell under the influence of polymerase 1, (d) Control sample of the same culture without the influence of polymerase 1.
It is important to note that the increase in numbers is caused
exclusively by gemmation and not mitosis; during which the cytomplasm
is always transparent or semi-transparent and there
isn’t any chromosome concensation.
An almost identical effect of a significant acceleration of glioblastomas’
division as well as their increase in size is observed
when introducing into the culture the Oxford/AstraZeneca (Ch-
AdOx1-S [recombinant] vaccine), with a concentration of 0.1 ml
to 15-40 ml of culture. Both the Oxford/AstraZeneca and Pfizer
vaccines also supported the division of glioblasts in the later
stages of incubation, after the control sample has already died
(Figure 10)

Figure 10: The influence of AstraZeneka on the glioblasts’ growth. (a) Signification increase in the number of glioblasts after the introduction of the
vaccine (control sample on Fig. 9), (b) Increase in the number of “monster” cells after the introduction of the vaccine.
Discussion
By observing the division process of the glioblastoma cells in
vitro, we are allowed to look at that process from a different
angle and give logically indisputable interpretations of imagistic
and intraoperative characteristics of glioblastomas.
During an MRI examination of glioblastomas’ defining characteristics,
as a rule we can observe the following:
• Infiltrative growth
• Significantly irregular shape of the new formation
• Irregular edges of the tumour
• The tumour crossing the boundaries of brain lobes
• Infiltration into the corpus callosum and the ventricular
ependyma
• Often, the presence of multifocal nodes that are closely positioned
but not directly linked to each other
• A significantly lower mass effect compared to other brain
tumours, especially meningiomas of the same size
• Presence of necrosis at the base of the tumour
An accumulation of gadolinium and infiltration by small capillaries of the irregular edge of the tumour (Figures 11a and 11b)

Figure 11: MRI of a patience with a glioblastoma of the right frontal lobe. (a-b) MRI prior to the first surgery, (c-d) MRI four months after the surgecy
– continual tumour growth.
What stands out in the post-operation follow-up MRI where
there were indications of a relapse is not the overall tumour
growth in the yet unformed post-op cavity, but rather the tumour
infiltration via a narrow slit on the edge of the cavity deep
into the healthy brain tissue and the significantly higher area
and steep of the infiltrative growth, compared to the pre-operation
state. You can see the appearance of a couple of unlinked
nodules of the tumour not far from the main process (Figures
11c and 11d)
The observations made during the surgery itself indicate the
heteromorphic nature of the glioblastoma and the state of the
brain tissue surrounding it. Areas of the tumour that got involved
in the infiltration process into the white matter at later stages
do so without any borders and are virtually indistinguishable
from the brain, even when operating on an area that has been
expanded by 5-7 times. The areas of the original tumour growth
are much easier to distinguish that area has significantly less
blood vessels and the density of the tumour can reach that of
a fibroblastic meningioma. The newly formed small vessels and
capillaries are concentrated on the outer edges of the tumour
and the surrounding brain tissue whereas inside the tumour
they are present in much smaller numbers or not at all. The tumour
core that is considered on an MRI as necrosis, shows up
as a as a colloid, protein. Opalescent, yellow-grey, non-vascular
mass; that often transforms into a light brown cyst.
Comparison of data coming from experimental cultivation of
glioblastomas in vitro, imagery results from MRI alongside with
the observations made during the surgical process of removing
glioblastomas, allow to postulate a non-traditional model of
amitotic growth of glioblastomas in the brain. This hypothesis
differs from the traditional understanding of the glioblastoma
cell clones that underline the actual tumour theory after multiple
uncontrolled mitotic divisions.
In essence, the healthy glial cells, under the influence of unknown
catalysts, go from the G0 phase to the synthetic G1
phase. The single–stranded DNA of these cells gets replicated
and starts amplifying uncontrollably gets transcribed into the
mRNA and synthetises a large amount of protein with the formation
of a bulla and gemmation of new cells. Said cells significantly
increase in size, swell up and then proceed to gemmate
again. The outer membrane of these cells is very thin and penetrable
for DNA fragments-small expresser proteins for DNA amplification.
These components go through the membrane of the
healthy glial cell and this process spreads on its own, creating
a picture of the infiltrative nature of the tumour growth. This
way, the volume of the tumour increases not only due to the
amitotic increase of the number of cloned cells but also due to the involvement of the healthy glial cells into the self-sufficient
process of them becoming now glioblastomas and genome of
the gemmated and transfected cells does not correspond at all
with that of a healthy glial cell. They are in perpetual synthetic
phase and remain transparent and without a nucleus. At the
same time, the process of copying remains self-stimulating and
it should be viewed as a biochemical process, rather than biological;
which can be replicated in vitro such as polymerase
chain reaction (PCR). The cell goes into a state of biochemical
resonance that is not controlled by the homeostatic cell mechanisms.
It is important to note that for the maintenance of this
process only the following components are needed-all nucleosides,
ribose, triphosphates and polymerase. It’s not excluded
that the proteins synthesized in these cells are expressers for
the DNA amplification, so one can talk about there being positive
biochemical feedback between the proteins and the DNA
of these cells.
An indirect confirmation of this hypothesis is the experimentally
confirmed fact of a significant increase in the rate of cell gemmation,
and the appearance of monster cells when polymerase
and nucleotides or the vaccine, in our case is Oxford/AstraZeneca
(ChAdO×1-S [recombinant] are added to the glioblastoma
cells medium), which transform the cell division process into a
self-sustained biochemical resonance process.
This concept allows a reasonable explanation of all the main
signs of glioblastomas via MRI examination and intraoperative
morphology.
Conclusions
1. The cellular proliferation of glioblastomas is polymorphic in
size and shape, with hyperchromic nuclei and condensed
chromosomes; and insignificant number of glial cells with a
transparent cytoplasm and invisible nuclei. The latter type
of cells is difficult to observe in histological samples and
culture dishes at the early stages of incubation.
2. Cells with condensed chromosomes divide via mitosis,
however the percentage of mitoses is insignificant. Cells
that have a transparent cytoplasm and de-condensed chromosomes
divide amitotically, without entering the mitosis
phase, creating a daughter cell via gemmation.
3. Infiltrative growth of glioblastoma in the brain is mainly due
to amitotic division, “budding” or gemmation of glioblastic
cells and transfection of pathological fragments of DNA
(RNA) into neighbouring healthy glial cells of the brain.
4. Chemotherapeutic drugs that affect various mechanisms of
blocking mitosis are not effective, since the process of glioblast
growth is amitotic, subcellular, biochemical in nature.
The protocol of this study was approved by the Research Ethics
Committee of the “Nicolae Testemitanu” State University of
Medicine and Pharmacy (nr.81 of 19.09.2020). All participants
gave their informed consent, both orally and in writing, in accordance
with the principles of the Helsinki Treaty adopted in
June 1964 with subsequent revisions and additions.
Acknowledgement
This study was supported by the State Program (2020-2023) of the Republic of Moldova (research grant No. 20.80009.5007.10).
Conflict of Interest
The authors declare that there is no conflict of interests regarding
the publication of this paper.
REFERENCES
- Mukasa A (2020) Surgical treatment of glioblastoma: Current limitations and future possibilities. JPN J Neurosurg. 29(3):173-180.
[Crossref] [Google Scholar]
- Gutenberg A, Lumenta CB, Braunsdorf WEK, Sabel M, Mehdorn HM, et al. (2013) The combination of armustine wafers and temozolomide for the treatment of malignant gliomas. A comprehensive review of the rationale and clinical experience. J Neurooncol. 113: 163–174.
[Crossref] [Google Scholar] [PubMed]
- Westphal M, Ram Z, Riddle V, Hilt D, Bortey E (2006) Gliadel wafer in initial surgery for malignant glioma: Long-term follow-up of a multicenter controlled trial. Acta Neurochir. 148:269–275.
[Crossref] [Google Scholar] [PubMed]
- Klug WS, Cumming MR, Spenser SA, Palladino MA (2013) Essential of Genetics.8th ed. Boston, Pearson Education. 521-545.
- Albertson DG, Collins C, Cormick F, Gray JW (2003) Chromosom aberrations in solid tumors. Nat Genet. 34:369-376.
[Crossref] [Google Scholar] [PubMed]
- Bird A (2007) Perceptions of epigenetics. Nature. 396-398.
[Crossref] [Google Scholar] [PubMed]
- Easwaran H, Tsai HC, Baylin SB (2014) Cancer epigenetics: Tumor heterogeneity, plasticity of stem-like states, and drug resistance. Mol Cell. 54:716–727.
[Crossref] [Google Scholar] [PubMed]
- Matsumoto T, Wakefield L, Peters A, Peto M, Spellman P, et al. (2021) Proliferative polyploid cells give rise to tumors via ploidy reduction. Nat Commun. 12:646.
[Crossref] [Google Scholar] [PubMed]
- Daniel J, Coulter J, Woo JH, Wilsbach K, Gabrielson E (2011) High levels of the Mps1 checkpoint protein are protective of aneuploidy in breast cancer cells. Proc Natl Acad Sci USA. 108:5384-5389.
[Crossref] [Google Scholar] [PubMed]
- Simonetti G, Bruno S, Padella A, Tenti E, Martinelli G (2019) Aneuploidy Cancer strength or vulnerability? Int J Cancer. 144:8-25.
[Crossref] [Google Scholar] [PubMed]
- Sheltzer JM, Replogle JM, Habibe Burgos NC, Chung ES, Meehl CM, et al. (2017) Single-chromosome gains commonly function as tumor suppressors. Cancer Cell. 31:240-255.
[Crossref] [Google Scholar] [PubMed]
- Swift LH, Golsteyn RM (2014) Genotoxic anti-cancer agents and their relationship to DNA damage, mitosis, and checkpoint adaptation in proliferating cancer cells. Int J Mol Sci. 15:3403-3431.
[Crossref] [Google Scholar] [PubMed]
- Xuan B, Ghosh D, Jiang J, Shao R, Michelle R (2020) Vimentin filaments drive migratory persistence in polyploidal cancer cells. Proc Natl Acad Sci USA. 117: 26756-26765.
[Crossref] [Google Scholar] [PubMed]
- Walen K (2018) Genomic instability in cancer I: Dna-repair triggering primitive hereditary 4n-skewed, amitotic division-system, the culprit in emt/met/metaplasia cancer-concepts. J Cancer Ther. 9:974-997.
[Crossref] [Google Scholar]
- Ben David U, Amon A (2020) Context is everything: Aneuploidy in cancer. Nat Rev Genet. 21:44–62.
[Crossref] [Google Scholar] [PubMed]
- Bhattathiri VN (2001) Amitotic cell divisions and tumour growth: An alternative model for cell kinetic compartaments in solid tumorts. Oral oncol. 37:288-295.
[Crossref] [Google Scholar] [PubMed]
Citation: Matcovschii V, Gudumac V, Lisii D, Andronache L (2022) Culture Insights of Cellular Mechanisms of Glioblastomas
Growth. Neurooncol. 7:52.
Copyright: © 2022 Matcovschii V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and
source are credited.