Key words
adaptation, asylum, community nursing,
cultural competence, equity, quality
Introduction
The UK National Health Service (NHS) is a universal,
insurance-based scheme, providing mostly free treatment
and nursing care at the point of delivery. Within Scotland, the NHS is devolved to the Scottish Government;
14 health boards are charged to deliver quality
health services within acute and community settings.
A primary healthcare system underpins NHS provision;
all UK residents are entitled to register with
a General Practitioner (GP). Community nursing is
integral to primary care provision, providing a range
of services including nursing in the home for housebound
adults and health visiting; the latter is a universal
service for women and families which aims
to promote health and reduce health inequalities
(Cowley and Frost, 2006).
The main driver to improve Scottish healthcare
quality in recent years has focused on the delivery of
person-centred, safe and effective healthcare (The
Scottish Government, 2010). Person-centred care is
an important element of cultural competence; healthcare
professionals are expected to respect individual
needs and values, whilst working in partnership with
patients and families in the delivery of compassionate
care. Although community nursing in Scotland has
historically served a largely white population, increased
immigration is resulting in a more culturally diverse
population. The Scottish Census in 2011 demonstrated
a population of 5,295,403 people, 7% (369,000) of
whomwere born outside Scotland (Scotland’s Census,
2014).
The United Nations High Commissioner for Refugees
(UNHCR) was instrumental in establishing the
Geneva Convention (1951), which remains the major
instrument of international refugee law (UNHCR
2003) and defines a person seeking asylum as someone
who:
‘Owing to a well-founded fear of being persecuted for
reasons of race, religion, nationality, membership of a
particular social group or political opinion is outside the
country of his nationality and is unable, or owing to such
fear, is unwilling to avail himself of the protection of that
country; or who, not having a nationality and being
outside the country of his former habitual residence as a
result of such events, is unable or, owing to such fear, is
unwilling to return to it.’ (1951 UN Convention Relating
to the Status of Refugees: Article 1A2).
Although Scotland now has its own parliament, it
makes no decisions regarding the regulation of UK
immigration, which is controlled centrally by the UK
Government. At the end of the twentieth century the
media highlighted the increasing number of asylum
applicants, raising concerns about abuse of the asylum
system which led to a lack of public sympathy
(Barclay, 2003). More recently, the plight of Syrian
refugees has received more compassionate reporting
(BBC News, 2014).
The tightening of UK asylum legislation in the 21st
century has reduced asylum applications. The UK
Visas and Immigration (UKVI) section of the Home
Office now manages the complex asylum application
process, which involves an initial screening, caseworker
allocation, an asyluminterview and an asylum decision (GOV.UK, 2014) . In 2013 there were 23,765
asylum applications compared to 84,132 in 2002
(Statistics at the Home Office, 2013). However, in
2013 only 37% of UK applicants were granted asylum
or temporary protection, most commonly applicants
were from Pakistan, Iran, Sri Lanka and Syria. Those
refused asylum are offered voluntary and assisted
return to their country of origin, but many are unable
to return home due to an unsafe home situation.
Since 2000, asylum applicants have been dispersed
throughout the UK, including Glasgow where the
study was carried out. UKVI provides welfare support
for asylum applicants through means-tested cash
support and housing accommodation on a no-choice
basis. Education is provided for the children of asylum
applicants. Whilst their application is in process,
asylum applicants and their families are entitled to
NHS primary care services on the same basis as UK
residents.
The asylum journey creates a huge psychological
stress for applicants (Maddern, 2004). The physical
wellbeing of asylum applicants is also compromised
by a previous lack of preventive healthcare, experience
of violence and rape, resulting in difficult childbirth
for female applicants (Maternity Action and Refugee
Council, 2013). Moreover, exposure to infectious
disease, such as HIV/AIDS, tuberculosis, hepatitis A,
B, C, malaria and other parasitic infections commonly
occurs during the journey.
Theoretical view of cultural
competence
Cultural competence is a social construction, open to
different interpretations and meaning; culture is the
medium through which we understand and interpret
the social and health behaviours of others and which I
defined as:
‘A socially acquired complex set of capabilities and
customs needed to operate coherently within society’
(Quickfall, 2010).
Community nurses require cultural competence skills
to provide equitable, accessible and non-discriminatory
services for their patients and clients (Jirwe et al,
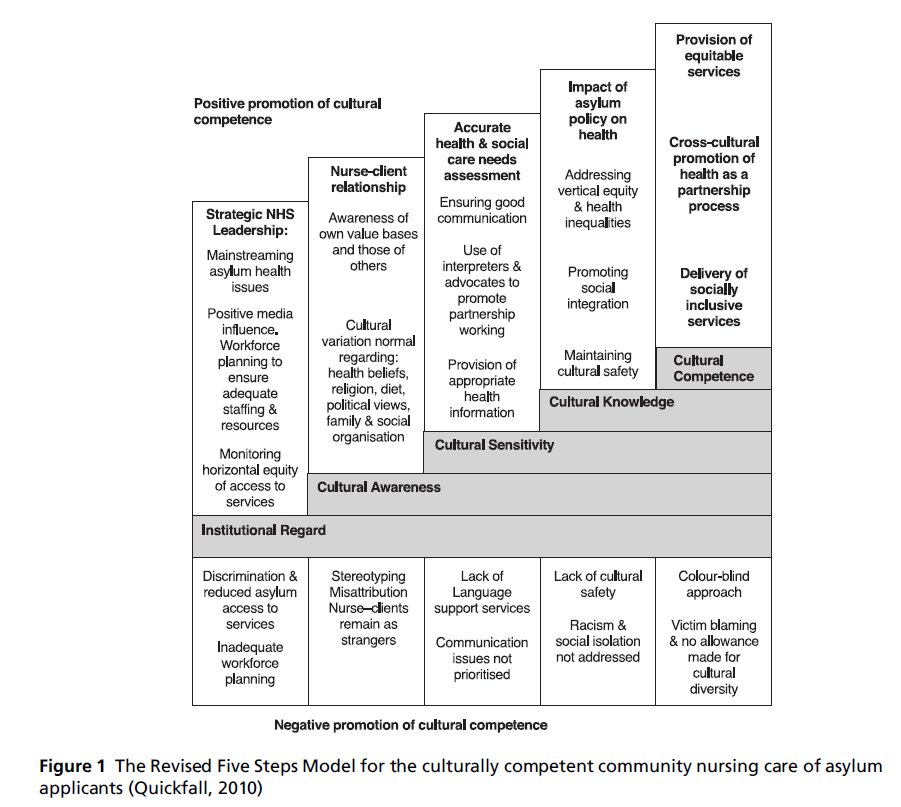
2009). Early in the study, I developed a Five Steps
Model for culturally competent care from the nursing
literature (Quickfall, 2004). Institutional regard is
placed first in the model as it provides strategic
direction for the operation of corporate values in
service delivery, including primary care and community
nursing capacity to promote equitable access
to services. Although entitled to mainstream NHS
Service, asylum applicants are known to experience difficulty in obtaining GP registration (Burnett and
Peel, 2001). Restricting asylum applicant access to
NHS primary care services is not cost-effective and
may result in additional demands on Emergency
Departments (Hargreaves et al, 2006).
The elements of the Papadopoulos model of cultural
competence, which includes cultural awareness, cultural
sensitivity and cultural knowledge (Papadopoulos,
2006), are included in the model. Cultural awareness
involves establishing nurse–client relationships through
the mutual exchange of values and beliefs to provide
person-centred care, whilst recognising the need to
challenge inappropriate or illegal cultural behaviour.
Cultural sensitivity relates to how healthcare professionals
communicate effectivelywith clients in their
care. When the nurse and client do not have a common
language, interpreter-mediated consultations
(IMCs) are essential for safe and effective care management.
Mediating through an interpreter requires
additional communication skills. An information requestmust
be adequately complex to obtain the required
information, but be sufficiently simple to be correctly
understood by the interpreter and meaningful to the client when interpreted into the client’s own language.
Cultural knowledge refers to the effects of poverty,
social marginalisation and racism leading to health
inequalities. Moreover, in fleeing persecution and
violence, asylum applicants frequently suffer posttraumatic
stress disorder (PTSD) (Silove et al, 2007).
The Revised Five Steps Model (Figure 1) (Quickfall,
2010) shows the four elements described above on the
horizontal axis, which are brought together as cultural
competence. The vertical axis of the revised model
highlights the positive or negative influences on the
delivery of culturally competent care.
Previous to 2000, small numbers of asylum applicants
from various countries throughout the world
were integrated into communities across Scotland.
Once operational, the UK Government Dispersal Programme
transferred large numbers of asylumapplicants
to Glasgow. Glasgow established an integrated infrastructure
to manage the accommodation, education
and primary health services for this vulnerable group
(McDonald, 2001). To enable access to primary care
services, specialist teams led by Health Visitors were
established in areas with high numbers of asylum applicants. Health Visitors in the UK are nurses, based
in the community, who have undertaken further
training in child health and development and in public
health.
Figure 1 :The Revised Five Steps Model for the culturally competent community nursing care of asylum
applicants (Quickfall, 2010)
Study design
The aim of the study was to establish the underlying
principles of cultural competence. Using an interpretive
theory of culture, the study aimed to find out
how community nurses incorporated the concept into
their practice to provide cross-cultural health and
nursing care of asylum applicants in Glasgow
(Quickfall, 2010).
Research design
Ethnography was chosen as the research methodology
to take account of the interpretive nature of cultural
competence in community nursing practice. I used an
iterative design to observe and record how the study
participants behaved and interpreted their own situation.
Ethnography is particularly challenging in that
the researcher has to be sufficiently involved to understand
the participants’ position whilst maintaining a
distance to be able to critically examine the study
context and produce a critical and interpretive account
of culturally competent nursing care of asylum
applicants (Fetterman, 1989; Hammersley and Atkinson,
1995). Ethical approval for the study was obtained
fromNHSGreater Glasgow and Clyde Research Ethics
Committee (www.nhsgg.org.uk) and Research and
Development consentwas obtained from the Assistant
Director of Nursing.
Methods
Following an initial pilot study, the fieldwork for the
study was conducted between 2005 and 2008. As the
major instrument of data collection, I carried out 25
sessions of participant observation of 21 primary care
informants and their asylum applicant patients or
clients (three GPs, eight health visitors, one family
health nurse, four staff nurses, one practice nurse, one
nursery nurse, two healthcare support workers, one
administrative assistant) and 39 of their asylum applicant
patients or clients. I observed routine home
visits, where interactions between community nurses
and their clients took place. Each observation was
followed by one ormore interviewswith each informant
separately, using an interpreter if necessary. The sample of 39 asylum applicant informants was obtained
in different ways; 27 asylum applicant informants
were typical everyday cases of the community nurses’
workload and 12 were part of an ESOL (English for
Speakers of Other Languages) class. Moreover I
interviewed five managers involved in asylum applicant
service provision. The observation and interview
data were recorded manually to avoid increasing
anxiety for asylum applicants, who were often very
wary of authority and would not have consented to a
recording of the interview. Field notes were written up
electronically within 24 hours to reduce researcher
bias and errors.
Findings
The data analysis was ongoing throughout the study
to identify and investigate emerging themes. The
findings were confirmed with the nursing literature
and other asylum applicant studies. The study is
context specific; there are limitations to the transferability
of the study findings, as Glasgow was the only
Scottish city at the time to receive UKBA dispersed
asylum applicants. The Revised Five Steps Model
described earlier provides a framework to examine
the study findings and to identify the challenges of
delivering nursing care for asylum applicants (Figure 1).
All study informants have been anonymised in this
article.
Institutional Regard
The promotion of equitable access to UK primary care
services for asylum applicants incurs additional costs,
due to the additional use of language support services
and extended consultations (Audit Commission, 2000).
At the time of the study, many asylum applicant
families were dispersed to Glasgow. To contain the
costs of asylum applicant primary healthcare, dedicated
health visitor-led services operated in densely
accommodated areas and mainstream primary care
services in less densely accommodated areas. June, a
health visitor informant with over 20 years’ experience
noted the additional workload:
‘[Today’s]...visit lasted one hour, as an interpreter was
used. It would normally have lasted only half an hour to a
member of the indigenous population.’
June recognises the provision of equitable care requires
language support, to ensure the service delivered is
non-discriminatory and an accurate health needs
assessment is carried out. Consequently additional
staff time and language support costs were incurred.
However, June notes in the quotation below that ideally all asylum applicants should receive mainstream
services to receive non-discriminatory services.
‘The integration of all asylum applicants into mainstream
services requires a more culturally competent model of
health visiting to achieve non-discriminatory services and
additional training to cascade the necessary knowledge
and skills.’
Moreover, health visitors at the time of the study
required additional training in cultural competence
skills to ensure equitable care and enable the integration
of asylumapplicants into mainstream services.
Cultural awareness
Cultural awareness skills in community nursing practice
involved the development of interpersonal relationships
to gain an understanding of a client’s
health beliefs and values. The nurse focus group
participants noted that asylum applicants were often
were wary of people in authority. Sharing the refugee
journeywith them helped to establish an interpersonal
relationship and build trust.
Cynthia, a Scottish informant with less than 10
years’ health visiting experience, recognised the importance
of person-centred care, as shown in the
following quote:
‘I try to meet my clients in the middle. I get the feel of
things and ask clients how they would normally resolve
this at home.’
When Cynthia states that ‘she gets the feel of things’,
she hopes to understand the client’s health beliefs, so
that she can work in partnership to build on these
beliefs when advising on a health issue. The client’s
cultural norms provided a framework for advice on
childcare. For example, I observed Cynthia giving the
following advice to the parents of Hasan, a child with
special needs who demonstrated difficult bedtime
behaviour:
‘You need to provide Hasan with a firmer bedtime
routine. It will give him confidence, and enable him to
adapt more easily to going to school.’
This advicewas given using an authoritative approach,
but it also helped the parents to adapt to a new social
environment. Moreover, it emphasised the expectation
of parents living in Scotland to ensure children
were ready and not too tired to attend school.
Cultural sensitivity
Cultural sensitivity involves both verbal and nonverbal
skills to communicate and to provide crosscultural
care. When no interpreter is available, health
professionals may resort to mime to overcome
language barriers (Bradby, 2001). Likewise, an asylum applicant focus group informant noted the importance
of non-verbal communication and stated:
‘Even though NHS 24 service operators can access an
interpreter language line service, it’s difficult to use
telephone-based services without the prompts of nonverbal
signals.’
In the study I observed that an initial contact visit was
frequently conducted to assess the client’s level of
spoken English. The community nurses did not automatically
request an interpreter, an expensive resource
that could take some days to arrange. Although family
members can act as interpreters, this high-risk strategy
makes the health assessment more difficult to carry
out due to insufficient linguistic skills (Hogg et al,
2006). Moreover, the family member interpreting the
consultation may find the client’s reply too sensitive to
translate into English or wish to control the information
shared. For example, a nurse focus group
informant commented:
‘I request an interpreter when there are concerns that the
husband can filter the conversation for his wife.’
Although a return visit might appear time consuming,
it provided an opportunity to further cement the
interpersonal relationship and work in partnership
with clients. In the following example, I observed
Cathy, a healthcare support worker, communicating
clearly with her client on how to use prescribed skin
medication effectively and safely, using body language
to clarify the message:
‘Cathy is very direct with her instructions about how to
apply the cream to the dry skin areas and uses a raised
voice and hand signs saying ‘this is what you do’.’
The community nurses had developed additional
communication skills to work through an interpreter
to find out the required information and give advice.
One nurse informant stated:
‘I use key words and phrases to simplify the message. The
interpreter does not always understand the message if I
use complex sentences.’
There were many opportunities for miscommunication
in using a third party to communicate with
clients. The nurse focus group informants commented
that with experience they knew when the interpreter
was not translating word for word. Major clues were
body language, as the interpreter would look uncomfortable.
Cultural knowledge
Once dispersed to Glasgow, asylum applicants at the
time of the study were not allowed to work and were
housed in condemned tower blocks. The specialist
community nursing services provided outreach clinic services for asylum applicants, which enabled easy
access to child health clinics close to their home.
Similar to previous reports (Clarke, 2004), women
were frequently the victims of rape, resulting in unintended
pregnancy. The burden of the asylum application
combined with mental and physical health
issues created high levels of psychological stress, as
an asylum applicant participant revealed:
‘I do not think about things too much – or else I feel my
head explodes.’
These high levels of stress are known to be damaging to
psychological health in the longer term. Mental health
is often compounded further by marginalisation and
racism, as the following vignette describes:
‘Wilma, a 35 years old asylum applicant from Liberia lived
with her husband, aged 37 years and their three daughters,
aged ten years, four years and three weeks old. She
described an incident, which made her cry, even though
it had occurred some months previously. She reported
that she had been waiting in the local supermarket
checkout queue and she was ready to be served at the
till. Someone put his groceries in front of hers. Wilma
said, ‘‘Excuse me, but there is a queue.’’ The white person,
who was obviously rather drunk replied, ‘‘You are just an
asylum seeker and have no right to be here’’.’
Asylum applicant respondents were confused by the
mixture of racist and non-racist attitudes of community
members. The adaptation process takes time
and is challenging, requiring the understanding of a
new set of social norms and behaviour. Community
nurses can help this adaptation process through enabling
access to ESOL classes to achieve greater fluency
in English and also through reinforcing the norms and
social expectations of parents living in Scotland. For
example Cynthia (health visitor informant described
earlier) stated:
‘One of the common child protection issues I have
encountered is that of leaving children at home alone.
For example, an Afghani woman had left her two children,
aged five years old and three years old, alone in the flat
while she went shopping. On my visit, the children invited
me into the flat. I waited with them until their mother
returned and explained that, although it may be safe to do
so in Afghanistan, UK parents are not allowed to leave
their children alone at home. The mother understood the
dangers and accepted that she should make appropriate
childcare arrangements in future.’
This example demonstrates the range of childcare
norms and parenting behaviour of asylum applicants.
The community nurses had a major role in aiding
adaptation to the new host environment through
reinforcing parenting expectations of asylum applicant
parents.
Discussion
This ethnographic study was carried out in Glasgow
and involved a small number of respondents. The
findings are context-specific and are not necessarily
applicable to the care of asylum applicants in other
settings, but there are common themes emerging from
the study.
An acceptance of a diverse range of health beliefs
rather than an emphasis on difference is fundamental
to the delivery of culturally competent community
nursing care. Although the Scottish healthcare quality
agenda centres on person-centered, safe and effective
community nursing care (The Scottish Government,
2010), cultural competent care is broader and encompasses
the notions of equity (Jirwe et al, 2009), as
well as promoting adaptation to a new social environment.
Specialist services for asylum applicants facilitate
equitable access to primary care services, but
separate services may be detrimental to aiding adaptation
to the new host community and potentially
create health inequalities. Thus mainstream access for
asylum applicants to NHS primary care services is
preferable, but embedding cultural competence into
practice may require additional workforce training.
Cultural competence skills are as important as
clinical skills in conducting a robust health and
nursing assessment (McDonald, 2001). In an economic
environment of escalating costs and constrained
resources, cultural competence skills are not a luxury,
but are cost-effective through ensuring that there is
neither an under prescription or an over prescription
of care. For example, the use of language support
services is complex, requiring additional skills to
deliver cross-cultural health and nursing care with
the support of an interpreter. Moreover, nurse prescribers
must ensure patient safety in the prescribing
and taking of medicines through working in partnership
with clients to understand any issues that might
arise from their cultural health beliefs and behaviour.
Community nurse informants at the time of this study
recognised the importance of aiding asylum applicants
to adapt to their new host environment. In
enabling their clients to become more fluent in English
through access to English classes, the nurses were
promoting acculturation and enabling equitable access
to services for their asylum applicant clients.
Moreover, the asylum applicants themselves were
gaining cultural competence skills through the adaptation
process, which enabled them to understand the
norms and values of the adopted community and
behave as expected in their new community.
Cultural competence is a complex concept
(Papadopoulos, 2006). When translated into practice,
it not only encompasses person-centred, safe and
effective care, but also involves promoting equitable access to NHS primary care and community nursing
services and siding adaptation to a new host community.
Thus, cultural competence involves the delivery
of cross-cultural care, whilst building on the
cultural assets of the clients to promote health.
Conclusion
The study findings showed that community nurses
employed skills of cultural awareness, cultural sensitivity
and cultural knowledge in their practice to
provide culturally competent care. Cultural competence
was as important as clinical skills; without a
robust health assessment inappropriate, ineffective or
unsafe nursing care might be provided. However,
cultural competence required a supporting corporate
infrastructure, referred to earlier as institutional regard,
to provide training, language support and other
specialist health services.
Three major themes emerged from the study as
major influences on the delivery of cultural competence;
the need for equitable service provision, the
cross-cultural promotion of health as a partnership
process and aiding adaptation to a new social environment
through the delivery of socially inclusive services.
The Revised Five Steps model described earlier
(Figure 1) incorporates these themes.
ACKNOWLEDGEMENTS
I wish to thank the Queen’s Nursing Institute Scotland
for funding the PhD study, my supervisors Dr Elaine
Haycock Stuart and Professor Tony Good for their
support and my husband for his patience.
ADDRESS FOR CORRESPONDENCE
Julia Quickfall. Email: quickfalljulia52@gmail.com
References
- Audit Commission (2000) Another country: implementing dispersal under the Immigration and Asylum Act 1999. Audit Commission, London.
- Barclay A, Bowes A, Ferguson I, Sim D, Valenti M (2003) Asylum seekers in Scotland. Scottish Executive Social Research, Edinburgh.
- BradbyH(2001) Communication, interpretation and translation. In: L Culley, S Dyson, eds, Ethnicity and nursing practice. Houndmills: Palgrave.
- Burnett A, PeelM(2001) Health needs of asylum seekers and refugees. British Medical Journal 322:544ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Clarke P (2004). Women who are raped. In:MPeel, ed, Rape as a method of torture. London: Medical Foundation for the Care of Victims of Torture, pp43ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â69.
- Cowley S, Frost M (2006) The principles of health visiting: opening the door in the 21st century. London: Community Practitioners and Health Visitors Association.
- GOV.UK (2014) Last update, Asylum www.gov.uk
- Hargreaves S, Friedland J, Gothard P, Saxena S, Millington H, Eliahoo J, Le Fetterman DM (1989) Ethnography step by step. Sage Publications, Newbury Park.
- Feuvre P and Holmes A (2006) Impact on and use of health services by international migrants: questionnaire survey of inner city London A&E attenders. BMC Health Services Research 6:153.
- Hammersley M and Atkinson P (1995) Ethnography principles in practice. Routledge, London.
- Hogg R, De Kok B, Hanley J et al (2006) An analysis of the experience of parenthood and of the health visiting service, from the perspectives of Pakistani and Chinese mothers of young children. Edinburgh: University of Edinburgh.
- Statistics at the Home Office (2014) Migration statistics. Available www.gov.uk/government/collections/migrationstatistics
- Jirwe M, Gerrish K, Keeney S, Emami A (2009) Identifying the core components of cultural competence: findings from a Delphi study. Journal of Clinical Nursing 18(18): 2622ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â34.
- Maddern S (2004) Post-traumatic stress disorder in asylum seekers. Nursing Standard 18(18):36ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Maternity Action and Refugee Council (2013) When maternity does not matter. Dispersing pregnant women seeking asylum. London: Maternity Action and Refugee Council.
- McDonald, A., 2001. Sanctuary in Glasgow. Community Practitioner 74(3):86ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Papadopoulos I (2006) The Papadopoulos, Tilki and Taylor model of developing cultural competence. In: I Papadopoulos, ed, Transcultural health and social care. Development of culturally competent practitioners. Edinburgh: Elsevier Churchill Livingstone.
- Quickfall J (2010) The cross-cultural promotion of health: a partnership process? Unpublished PhD thesis, University of Edinburgh, UK.
- Quickfall J (2004) Developing a model for culturally competent primary care nursing for asylum applicants and refugees in Scotland: a review of the literature. Diversity in Health and Social Care 1(1):53ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â64.
- ScotlandÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Census (2014) March update, Census Results 2011 www.scotlandscensus.gov.uk/census-results
- Silove D, Steel Z, Susljik I et al (2007) The impact of the refugee decision on the trajectory of PTSD, anxiety, and depressive symptoms among asylum seekers: a longitudinal study. American Journal of Disaster Medicine 2(6):321ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- The Scottish Government (2010) The Healthcare Quality Strategy for NHS Scotland. Edinburgh: NHS Scotland; Healthier Scotland.
- UNHCR (2003) The state of the worldÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s refugees 2000: fifty years of humanitarian action. www.unhcr.org/4a4c754a9. html