Keywords
Coronary sinus; Great cardiac vein; Coronary sinus interventions; Synchronized coronary venous retroperfusion; Stem cell delivery
Abbreviations
PCI: Percutaneous Coronary Intervention; CS: Coronary Sinus; SRP: Synchronizing Retroperfusion; SSR: Synchronized Suction and Retroperfusion; PICSO: Pressure-controlled Intermittent Coronary Sinus Occlusion; ABMMC: Autologous Bone Marrow Mononuclear Cell Transplantation; PRCSP: Percutaneous Retrograde Coronary Sinus Perfusion; FMR: Functional Mitral Regurgitation
Introduction
Percutaneous coronary intervention (PCI) and cardiac by-pass surgery remains the corner stone management for severe angina, myocardial ischemia and myocardial infarction. But there are instances when patient may not be a candidate for both the procedures. Coronary sinus remains the potential site for alternative approach in these situations. Pratt was the first to describe use of coronary sinus to deliver arterial blood to ischemic myocardium [1]. Beck was an important pioneer in developing Beck I procedure which includes surgically narrowing the coronary sinus and elevating the coronary venous pressures in association with partial pericardiectomy. In the Beck II procedure, the coronary venous system was arterialized [2]. Later coronary sinus lost its charm with development of PCI. In this study, I explored the opportunity to consolidate and review the anatomy, various physiological and biochemical aspects, therapeutic approaches in invasive cardiology and future research prospects in a nutshell. The routine use of coronary sinus for electrophysiological procedures is well known and is described briefly in this article.
Coronary Sinus Anatomy
The coronary sinus (CS) is the main cardiac vein and it has become a clinically important structure especially through its role in providing access for different cardiac procedures. The CS is a wide venous channel, about 2-5.5 cm long, situated in the left, diaphragmatic part of the coronary sulcus, covered by muscular fibers from the left atrium and is dependent on the site of the drainage of the posterolateral vein. It ends in the right atrium, between the opening of the inferior vena cava and the atrioventricular aperture. Its orifice (coronary sinus ostiumCSO) is 5-15 mm in diameter and it is often guarded by a fold of endocardial tissue, an embryological remnant of the caudal portion of the right valve of the embryonic sinoatrial orifice, termed the valve of the CS or thebesian valve [3].
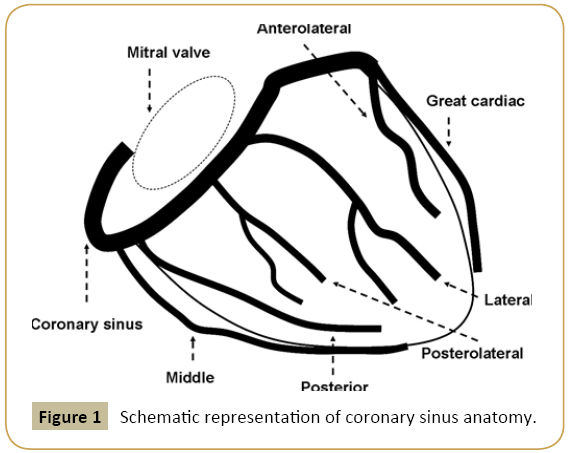
Coronary sinus is formed by greater cardiac vein and main posterolateral vein. Greater cardiac vein runs along the interventricular groove similar to its counterpart left anterior descending artery. The anterior wall of the left ventricle and interventricular septum are drained by branches of the anterior interventricular vein, known as the great cardiac vein on the annulus [4]. Other major tributaries entering the CS include inferior left ventricular vein and the middle cardiac vein that drain the posterior aspect of the left ventricle. Various atrial veins and vein of marshall drains atrial myocardium into the CS. The smaller cardiac veins also known as Thebesian venous network drains the inner layers of myocardium directly into the right ventricle. Their orifices are less than 0.5 mm in diameter [5] (Figure 1).
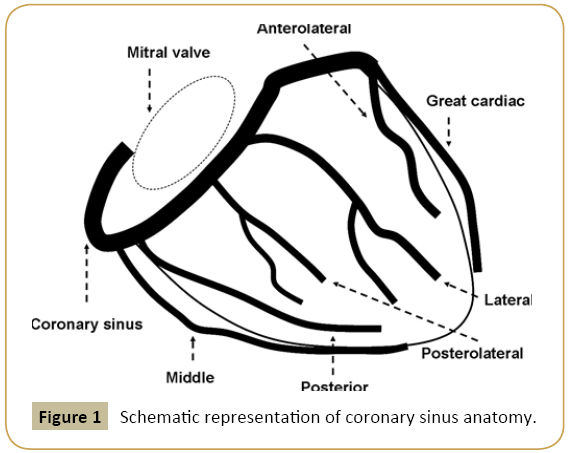
Figure 1: Schematic representation of coronary sinus anatomy.
Basic Science Aspects
Physiological aspects
The acute effects of elevation of coronary sinus pressure have been studied on dogs. It has been shown that the perfusion of the sinus from a systemic artery produces larger retrograde flows than those resulting from simple sinus occlusion, probably because of the higher sinus diastolic pressure. Arterialization of the coronary sinus provides acute benefit to the myocardium following coronary ligation, but it is insufficient to maintain normal contraction. However, in the presence of normal or reduced coronary inflow, acute elevation of sinus pressure results in myocardial anoxia probably due to restriction of capillary flow [6].
Faxon, et al. concluded that in humans, end-diastolic CS occlusion pressure closely parallels LV end-diastolic pressure, and measurement of CS occlusion pressure to assess LV end-diastolic pressure may have clinical use [7].
Biochemical aspects
Truong, et al. showed that CS sampling of heart failure biomarkers may be better than PV sampling for predicting Cardiac Resynchronization Therapy (CRT) outcomes. NT- pro BNP, galectin-3 and soluble ST2 levels were measured in 73 patients at the time of CRT implantation from coronary sinus and peripheral blood sampling. NT-proBNP concentrations were 20% higher in the CS than in the periphery, while galectin-3 and soluble ST2 concentrations were 10% higher in the periphery than in the CS (all P<0.001). There were 45% CRT nonresponders at 6 months and 16 (22%) patients with MACE. Triple-positive CS values yielded the highest specificity of 95% for predicting CRT nonresponse [8].
Literature Supporting Coronary Sinus Interventions in Myocardial Ischemia
Several decades ago the advances in catheter technology led to the development of a more sophisticated method of synchronizing retroperfusion (SRP) to diastole, allowing normal drainage during systole aiming to penetrate the venous system more effectively. The method was even evaluated as support of highriskangioplasty 9 and in patients with acute coronary syndromes, but the concept had to be abandoned due to the lack of efficiency and missed clinical end points. A further advancement of the SRP concept was selective synchronized suction and retroperfusion (SSR). SSR relies on a selective access of the local coronary vein draining the ischemic area. In contrast to SRP, the regional cardiac veins are emptied by suction of blood before retroinfusion. Early clinical evaluations have shown benefits of pressure-controlled intermittent coronary sinus occlusion (PICSO) during coronary artery bypass grafting [9] and experimental studies demonstrate the salvage potential for the ischemic myocardium.
Synchronized coronary venous retroperfusion is a technique that provides perfusion of the patient's arterial blood to the jeopardized myocardium retrogradely through the coronary veins. Because perfusion is retrograde rather than anterograde, its efficacy is not influenced by the number, location or degree of stenosis, tortuosity or branching of the coronary artery. This method has been extensively investigated in animals and has been shown to provide significant myocardial support in preliminary clinical studies. Kar, et al. [9] studied coronary sinus retroperfusion in 36 patients during balloon angioplasty was safe, feasible and effective in ameliorating and delaying the onset of ischemia. Furthermore, retroperfusion provided myocardial support during complicated and failed angioplasty and reversed cardiogenic shock in one patient [10].
The development of percutaneous coronary interventions and stenting in acute coronary syndromes clearly shifted the interest away from the coronary venous system. Despite considerable improvements in experimental and early clinical studies, the existence of two schools of thought and the unilaterally aligned interest of the medical device industry drowned an otherwise interesting and clinically feasible concept for almost three decades.
Angiogenesis and resurrection
The central contribution in this hypothesis is the discovery of Zheng, et al. [11] who demonstrated that coronary microvascular endothelial cells under shear stress upregulate vascular endothelial growth factor (VEGF). This mechanical kinetic action of blood flow is also modeling the developing heart [12]. Pulsatile stretch on coronary venous endothelium by intermittent elevated pressure resumes actions in the developing heart and opens dormant pathways in the adult heart. Grunewald, et al. [13] found that VEGF induces perivascular expression of the chemokine SDF1, homing circulating progenitor cells and enhancing in situ proliferation of resident activated endothelial cells [13], thus promising that angiogenesis and regeneration can be achieved by mobilization, attraction, and implantation of pluripotent cells.
Role in stem cell therapy
Autologous bone marrow mononuclear cell transplantation (ABMMC) for acute myocardial infarction in patients not eligible for percutaneous coronary intervention or coronary artery bypass surgery is performed through intracoronary infusion and was studied in majority of the trials [14,15]. In refractory ischemia, few trials studied about intramyocardial injection of ABMMC [16]. There have been some preclinical studies which show Percutaneous retrograde coronary sinus perfusion (PRCSP) is a reasonable alternative to intracoronary and intramyocardial delivery in preclinical therapeutic angiogenesis models using angiogenic proteins, gene therapy and stem cell therapy [17].
Tuma et al. [18] studied delivery of ABMMC by PRCSP technique in 14 patients with chronic refractory angina and stress induced reversible ischemia using SPECT. They demonstrated that ABMMC delivered by PRCSP in patients with chronic refractory angina and stress-inducible ischemia was safe, may reduce anginal symptoms and improve exercise capacity. In addition they observed that improved systolic LV function occurred only in patients with low ejection fraction at enrollment [19].
Current clinical implications
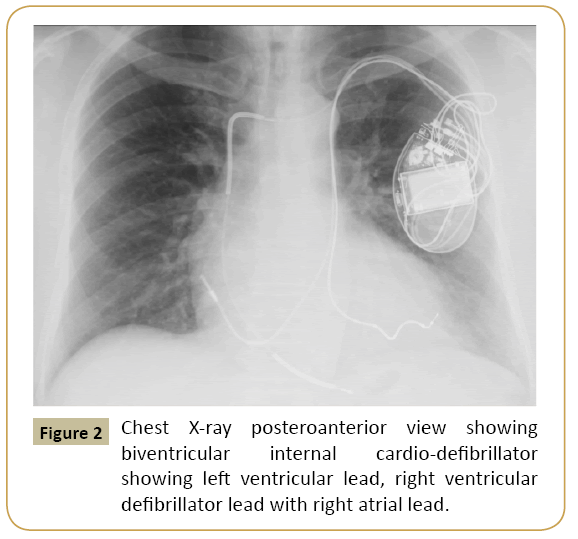
Electrophysiological procedures like left ventricular pacing during EP study are performed through coronary sinus. AICD and biventricular lead placement is performed using coronary sinus cannulation. Arrhythmia mapping and radiofrequency catheter ablation are the other clinical procedures done using coronary sinus conduits. Retrograde cardioplegia is now widely used in coronary artery bypass surgeries. Recently para-hisian pacing was attempted through coronary sinus was found to have better outcomes than right ventricular pacing [20,21] (Figure 2).
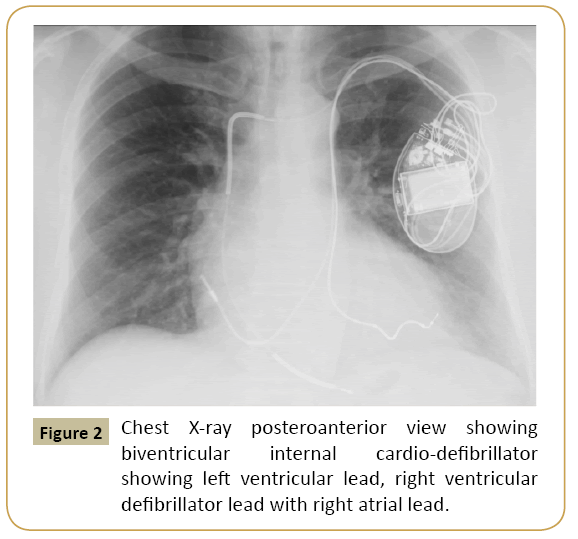
Figure 2: Chest X-ray posteroanterior view showing biventricular internal cardio-defibrillator showing left ventricular lead, right ventricular defibrillator lead with right atrial lead.
Role in functional mitral regurgitation
The valve of Vieussens is usually seen in midway of great cardiac vein and coronary sinus which demarcates the differentiation where the great cardiac vein becomes the coronary sinus. This venous structure lies about 1 cm above the posterior mitral annulus on the left atrial size and passes parallel to the annulus, extending from approximately commissure to commissure. Secondary or functional mitral regurgitation (FMR) occurs when the mitral leaflets are effectively normal; however, cardiomyopathy-induced annular dilation and/or tethering of the mitral valve affects its competence. The relationship between the great cardiac vein and coronary sinus (henceforth referred to as the coronary sinus) has been used to place devices capable of providing a cinching force on the posterior annulus of the mitral annulus. Theoretically, this force on the mitral annulus may be helpful in reducing secondary mitral regurgitation by reducing annular size. Three safety and efficacy studies were carried out in Europe: AMADEUS (CARILLON Mitral Annuloplasty Device European Union Study), TITAN, and TITAN II [19]. All subjects had to have symptomatic congestive heart failure, New York Heart Association classification (NYHA) 2 to 4, 6 minute walk test (6 MWT) 150 to 450 m, 2+ or greater FMR, depressed left ventricular function (ejection fraction <40%), and dilated left ventricle (left ventricular end-diastolic diameter >55 mm). Each of the studies demonstrated a low incidence of major adverse events out to 30 days and no events were deemed to be device-related by independent safety and monitoring boards. There was clinical benefit in each trial, with a consistent 1-grade improvement in NYHA class and approximately 100 m 6 MWT increase seen in all 3 trials. These benefits were seen immediately and demonstrated durability for 2 years (evaluated for 6 MWT) and 4 years (for NYHA class) [19]. The lack of randomized trials and blinded comparison is not available with these studies which limits the clinical use and warrants further studies comparing interventions.
Research directions
Coronary venous catheterization opens up new horizons for interventional cardiology research. Transcoronary sinus techniques for myocardial ischemia or infarction should be helpful for patients not a candidate for surgery or PCI. But the great potential for research lies in stem cell transplantation through coronary venous sinus retrograde perfusion and also mechanical induction of angiogenesis by intermittent pressure and mechanoduction. Further thoughts are research on retrograde perfusion of thrombolytics and heparin through coronary sinus in severe or large myocardial infarction.
Conclusion
Coronary sinus interventions are compiled in a nutshell in this article with brief discussion of anatomy, physiology and biochemical concepts. Excessive mortality and severe side effects, such as myocardial edema and hemorrhage, and an insufficiently advanced technology resulted in the temporary demise of the coronary sinus approaches. Recently, however, the need to improve myocardial protection, despite enormous advances in coronary bypass surgery and interventional cardiology, has resulted in renewed interest in the coronary sinus as an access route to deprived myocardium. Advances in technology such as percutaneous catheter techniques have improved access to the coronary venous system and allowed for a physiological adaptation of coronary sinus retroperfusion techniques.
References
- Pratt FH (1898) The nutrition of the heart through the vessels of Thebesius and the coronary veins. Am J Physiol1:86.
- Beck CS, Stanton (1948) Revascularization of heart by graft of systemic artery into coronary sinus. J Am Med Assoc 137:436-442.
- ZhivadinovikJ, Papazova M, Matveeva N, Dodevski A, Zafirova B. Anatomy of coronary sinus ostium. Folia Morphol (Warsz).
- Grzybiak M (1996) Morphology of the CS and contemporary cardiac electrophysiology. Folia Morphol (Warsz)55:272-273.
- Cendrowska-Pinkosz M, Urbanowicz Z (2000) Analysis of the course and the ostium of the oblique vein of the left atrium. Folia Morphol (Warsz) 59:163-166.
- Eckstein Rq, HornbergerJc, Sano T (1953) Acute effects of elevation of coronary sinus pressure. Circulation 7:422-436.
- Faxon DP, Jacobs AK, Kellett MA, McSweeney SM, Coats WD, et al. (1985) Coronary sinus occlusion pressure and its relation to intracardiac pressure. Am J Cardiol56:457-460.
- Truong QA, Januzzi JL, Szymonifka J, Thai WE, Wai B, et al. (2014) Coronary sinus biomarker sampling compared to peripheral venous blood for predicting outcomes in patients with severe heart failure undergoing cardiac resynchronization therapy: the BIOCRT study. Heart Rhythm 11:2167-2175.
- Kar S, Drury JK, Hajduczki I, Eigler N, Wakida Y, et al. (1991) Synchronized coronary venous retroperfusion for support and salvage of ischemic myocardium during elective and failed angioplasty. J Am Coll Cardiol18:271-282.
- Mohl W, Simon P, Neumann F, Schreiner W, Punzengruber C (1988) Clinical evaluation of pressure-controlled intermittent coronary sinus occlusion: randomized trial during coronary artery surgery. Ann Thorac Surg 46: 192-201
- Zheng W, Seftor EA, Meininger CJ, Hendrix MJ, Tomanek RJ (2001) Mechanisms of coronary angiogenesis in response to stretch: role of VEGF and TGF-beta. Am J Physiol Heart CircPhysiol 280: 909-917.
- Groenendijk BC, Hierck BP, Vrolijk J, Baiker M, Pourquie MJ, et al.(2005) Changes in shear stress–related gene expression after experimentally altered venous return in the chicken embryo. Circ Res 96: 1291-1298.
- Grunewald M, Avraham I, Dor Y, Bachar-Lustig E, Itin A, et al. (2006) VEGF- induced adult neovascularization: recruitment, retention and role of accessory cells. Cell 124: 175-189.
- Schachinger V (2004) Transplantation of progenitor cells and regeneration enhancement in acute myocardial infarction: final one-year results of the TOPCARE-AMI Trial. Journal of the American College of Cardiology 44:1690-1699
- Chen SL (2004) Effect on left ventricular function of intracoronary transplantation of autologous bone marrow mesenchymal stem cell in patients with acute myocardial infarction. The American journal of cardiology 94:92-95.
- Perin EC (2003) Transendocardial, autologous bone marrow cell transplantation for severe, chronic ischemic heart failure. Circulation 107:2294-2302.
- Hoshino K (2006) Three catheter-based strategies for cardiac delivery of therapeutic gelatin microspheres. Gene therapy 13:1320-1327.
- Tuma J, Fernández-Viña R, Carrasco A, Castillo J, Cruz C, et al. (2011) Safety and feasibility of percutaneous retrograde coronary sinus delivery of autologous bone marrow mononuclear cell transplantation in patients with chronic refractory angina. J Transl Med 9:183.
- Schofer J, Siminiak T, Haude M (2009) Percutaneous mitral annuloplasty for functional mitral regurgitation: results of the CARILLON Mitral Annuloplasty Device European Union Study. Circulation 120: 326-333.
- Mohl W (1987) Coronary sinus interventions: from concept to clinics. J Card Surg 2:467-493.
- Hong Kim J, Won Hwang K, Ku Chon M, Byoung Nam G (2015) Trans-coronary sinus intraseptalpara-Hisian pacing: Cerclage pacing. Heart Rhythm.