- (2005) Volume 6, Issue 6
Günay Gürleyik1, Seyfi Emir1, Gamze Kiliçoglu2, Alper Arman2, Abdullah Saglam1
1Department of Surgery and 2Department of Radiology, Haydarpasa Numune Education and Research Hospital. Istanbul, Turkey
Received May 29th, 2005 - Accepted August 4th, 2005
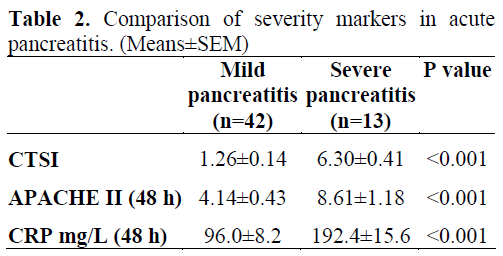
Context The assessment of the severity of pancreatitis is important for proper management of this challenging disease. A highly accurate system which could predict the severity and identify the local extent and complications of a serious inflammation, is beneficial for patient outcome. Objective The aim was to establish the value of the computed tomography severity index in predicting the severity of acute pancreatitis and to compare it with the accuracy of the APACHE II score and serum CRP concentrations. Design Prospective clinical series. Patients Fifty-five consecutive patients (37 women, 18 men; mean age 57 years) with a clinical and laboratory diagnosis of acute pancreatitis. Interventions Clinical evaluation, biochemical analysis of blood and contrastenhanced abdominal CT. Main outcome measures Computed tomography severity index within the first 5 days, serum CRP level, and clinical APACHE II score at 48 hours after admission. Results Thirteen patients had severe pancreatitis according to the Atlanta classification. The mean values of predictive markers in the mild and the severe pancreatitis groups were: computed tomography severity index 1.26 and 6.30 (P<0.001); APACHE II 4.14 and 8.61 (P<0.001); and CRP 96.0 mg/L and 192.4 mg/L (P<0.001), respectively. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy were calculated for the CTSI (greater than 3: 85%, 98%, 92%, 95%, and 95%), for APACHE II (equal to, or greater than 7: 62%, 86%, 57%, 88%, and 80%) and for CRP (equal to, or greater than 150 mg/L: 85%, 74%, 50%, 94%, and 76%). Conclusion The computed tomography severity index is a reliable method for staging the severity of acute pancreatitis; moreover, CT has the ability of showing the local extent of the inflammation and the occurrence of local complications.
Acute-Phase Reaction; Diagnostic Imaging; Inflammation; Pancreas
APACHE: acute physiology and chronic health evaluation; CTSI: computed tomography severity index; NPV: negative predictive value; PPV: positive predictive value
Acute pancreatitis is highly variable in clinical presentation and severity. In the majority of patients, the course is mild and self-limiting, but in 20% of patients it may become fulminant and progress to multisystem organ failure and death [1]. Because of this potential for catastrophic deterioration, the stratification of injury severity is essential. It is necessary to manage these patients in an intensive care unit with early and aggressive treatment in order to improve outcome. Both anatomic and physiologic criteria are used to stage the severity of acute pancreatitis [1, 2, 3]. The most common anatomic method of staging is based on contrast-enhanced computed tomography imaging. Balthazar and Ranson developed a grading system for severity based on CT findings. This computed tomography severity index (CTSI) is derived by assessing the degree of pancreatic and peripancreatic inflammation, fluid collection and parenchyma necrosis [4, 5]. The severity scoring system of the acute physiology and chronic health evaluation (APACHE II) was applied by Larvin and McMahon in the setting of acute pancreatitis, and it was demonstrated that those with scores higher than 7 were likely to have severe disease [6]. The acute phase reactant C-reactive protein (CRP) is the best established and most available predictor of inflammation [7, 8].
The purpose of this study was to assess the predictive value of the CTSI for severity of inflammation, and compare it with the APACHE II score and serum CRP level in acute pancreatitis patients.
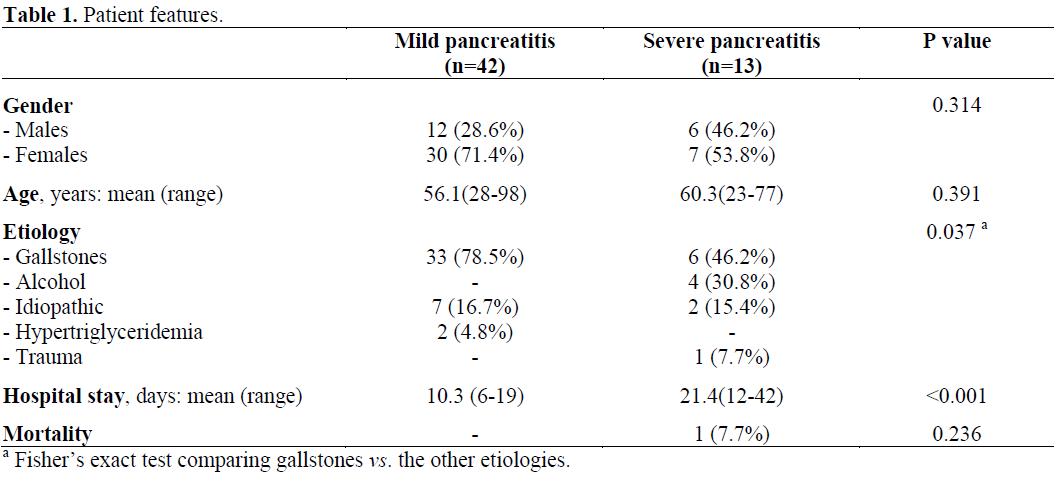
Between January 2001 and March 2005, a total of 55 consecutive patients with acute pancreatitis were prospectively studied. There were 18 men and 37 women. The mean age was 57 years (range: 23-98 years) (Table 1). Inclusion criteria were typical abdominal pain and a serum amylase level three times higher than normal. APACHE II scores were calculated at 48 hours [6, 9]. CRP levels were measured using an immunonephelometric method (Behring Turbitimer, Behringwerke AG, Marburg, Germany) at 24, 48 and 72 hours after the onset of symptoms. The levels of CRP determined at 48 hours were used in this study and those higher than 150 mg/L were accepted as being indicative of severe inflammation as reported in previous studies [8]. Intravenous contrast-enhanced abdominal CT was performed to assess the degree of pancreatic inflammation, pancreatitis-related fluid collections and necrosis within the first five days. Abdominal CT was performed using 5 mm axial slices before and after contrast material injection with a spiral CT device (Hitachi, Pronto, Japan). The CTSI was calculated from the extent of inflammation and necrosis, and the presence of fluid collections. The CTSI is scored as: normal gland (0 points), gland enlargement (1 point), peripancreatic inflammation (2 points), single fluid collection (3 points), and multiple fluid collection (4 points), extent of pancreatic necrosis less than 30% (2 points), extent of pancreatic necrosis from 30 to 50% (4 points), and extent of pancreatic necrosis more than 50% (6 points) [5]. The criteria of the severity of acute pancreatitis were based on the Atlanta classification [10] including the presence of local (pancreatic necrosis, pseudocysts, abscess), and systemic complications (accompanying organ failure, renal failure, pulmonary insufficiency, shock e.g.). The sensitivity, specificity, accuracy, and positive predictive values (PPVs), and negative predictive values (NPVs) of all parameters were calculated in order to evaluate their diagnostic capacity in identifying the severity of pancreatitis.
Informed consent was obtained from each patient on the day of admission. The study protocol conforms to the ethical guidelines of the World Medical Association, Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004, as reflected in a priori approval by the appropriate institutional review committee.
Results were expressed as mean±SE. Statistical analyses were made using the Student t test, the Fisher’s exact test, and the McNemar test and were carried out by means of the SPPS for Windows (version 13.0). P values less than 0.05 were accepted as statistically significant.
RESULTS
All 42 patients with acute mild pancreatitis according to the Atlanta classification have shown complete resolution with conservative treatment. Thirteen patients were classified as having severe disease and were monitored in the intensive care unit (ICU) due to local and/or systemic complications (necrosis less than 30% in 6, necrosis less than 30% and renal failure in 3, the extent of necrosis between 30 and 50% in 3, and respiratory failure in one patients). One patient (7.7%) with severe pancreatitis died after multiple organ failure. Hospital stay was significantly longer in the group with severe disease as compared to the group with mild disease (P<0.001). Gallstones were the leading cause in both of acute pancreatitis groups (Table 1). The severity markers which were used in this study, were found to be significantly different between the mild and the severe groups (P<0.001) (Table 2). The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value which were calculated for evaluating the diagnostic capacity of the three parameters used for identifying the severity of pancreatitis have pointed out the superiority of the CTSI. The accuracy of the CTSI for predicting the severity of acute pancreatitis was found to be significantly higher than the other parameters used (Table 3).
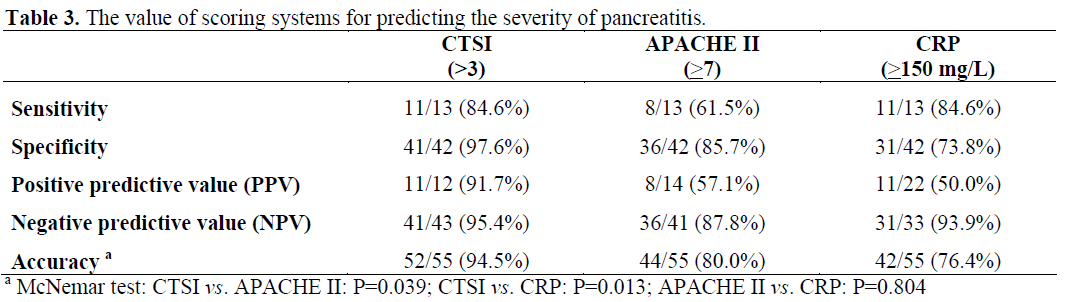
The majority of patients with acute pancreatitis have mild disease and their clinical symptoms and laboratory findings resolve with supportive care within 3 to 5 days. On the contrary, severe pancreatitis is associated with organ failure and local complications such as necrosis, abscess formation and pseudocysts, and constitutes 15-20% of such cases [1, 2, 10]. Twenty-four percent of our cases were complicated but, in the majority of patients, the disease was self- limiting. Various scoring systems are used for predicting the severity of acute pancreatitis [2, 3, 11, 12]. In this study, an index based on imaging method, a score based on a physiologic and health evaluation system, and a biochemical inflammatory parameter were prospectively used to predict the severity of disease. Therefore, the accuracy of the CTSI, APACHE II score and serum CRP measurement were investigated for determining the severity of acute pancreatitis. APACHE II which is a nonspecific scoring system and a health status indicator has been in use for patients with acute pancreatitis since 1989 [6]. Previous studies have shown that acute pancreatitis with APACHE II scores greater than 7 were likely to have a severe course. The development of organ failure and/or local complications were defined as features of a complicated disease [6, 11]. The mean APACHE II score which was significantly higher in our severe pancreatitis group has confirmed the complicated course of the disease. In our study, the PPVs of APACHE II were found to be lower (57%) at 48 hours after admission. Larvin and McMahon [6] have shown that the APACHE II score had PPV as 67% and 71% at 24 and 48 hours after admission. In our study, the sensitivity (62%) and the specificity (86%) of APACHE II were comparable with previous findings. Osvaldt et al. [3] have reported the sensitivity and specificity to be 75% and 79%, respectively. The APACHE II system allows monitoring of disease progression and response to therapy but the system is complex, more difficult to perform and is less accurate for identification of local complications [11, 12]. Serum CRP is an acute phase reactant, which is elevated in various inflammatory conditions, and serves as a nonspecific inflammation marker. It is easy and economical to measure the CRP serum level. CRP is a proven predictor of severity for acute pancreatitis when serum level over 150 mg/L is measured within 48 hours after the onset of symptoms [11, 13]. Significantly higher serum concentrations of CRP in our patients with severe disease have shown the value of this easy detectable marker. Neoptolemos et al. [14] have also found that CRP concentrations were significantly different between mild and severe pancreatitis cases at 48 hours, but not at 24 hours. The sensitivity and the positive predictive values of serum CRP levels in patients with severe pancreatitis have been reported to be 83 to 100%, and 37 to 77 %, respectively [8]. In our study, the sensitivity (84%), the specificity (73%) and the PPVs (50.1%) of serum CRP measurements have revealed their potential to determine the severity of the disease. These rates were not considerably high but the advantage of easily measuring the CRP level by blood chemistry outweighs these relatively lower values. Arvanitakis et al. [15] have investigated the correlation between magnetic resonance imaging (MRI) and clinical outcome. They have demonstrated that MRI on admission correlated with CRP levels at 48 hours after admission.
Balthazar and Ranson [5] have shown that contrast-enhanced computed tomography assessment correlated with the clinical course of the disease and with the prediction of mortality. They found a 3% mortality rate in patients with a CTSI score greater than 3 whereas patients with a CTSI score greater than 7 had a mortality rate of 17%. Similarly, the higher CTSI scores in our severe pancreatitis cases with local and/or systemic complications have predicted the complicated course of the disease when compared with the CTSI score of the mild group. Simchuk et al. [12] have shown that there was a correlation not only with the CTSI score and the mortality rate but also with the duration of the hospital stay and the need for necrosectomy. In our study, a CTSI score greater than 3 suggested was indicative of a longer hospital stay and a higher complication rate than in cases with a lower CTSI score. The risk of infection increases with the extent of intrapancreatic and extrapancreatic necrosis; therefore, early recognition of necrosis is important in order to prevent a poor outcome. Contrast-enhanced computed tomography provides a better and earlier recognition of such a risk as compared to other scoring systems [5, 12, 16]. On the other hand, Mortele et al. [17] used a modified CTSI which included a simplified assessment of pancreatic inflammation, necrosis and extrapancreatic complications. When using the modified index, a significant correlation was found between the severity of pancreatitis and the development of organ failure.
The final evaluation was to compare and comment on the values of the diagnostic markers for predicting the severity of pancreatitis. Contrast-enhanced computed tomography assessment and CTSI calculation requires expertise. The APACHE II system is complex and has a low accuracy rate in identifying local complications. The serum CRP level is easily detectable using blood chemistry and it is the most economical marker for severity of inflammation. In our study, the sensitivity of CRP measurement was comparable with the CTSI. We found a close correlation with CRP levels and the CTSI, so high that 91% (10/11) of patients having severe pancreatitis and a CTSI score greater than 3 had a serum CRP level in excess of 150 mg/L. The complex APACHE II system is not advantageous when compared to the easily detectable CRP concentration, having a lower sensitivity, and comparable PPVs and accuracy rates. These two markers (APACHE II and CRP) are incapable of identifying local complications. The highest (sensitivity, specificity, PPV, NPV, and accuracy) rates of a CTSI score greater than 3 according to the other two markers of our study have supported the value of enhanced computed tomography evaluation for determining the severity of acute pancreatitis. Additionally, computed tomography has the ability of detecting the extent of local inflammation and the presence of local complications.
We concluded that scoring systems allow us to target patients with high scores for close monitoring and more aggressive intervention. The CTSI correlates to the clinical course, severity of disease, and has better accuracy rates when compared with APACHE II score and CRP level. Enhanced computed tomography is advantageous in establishing the extent of local inflammation and the occurrence of local complications. Although CT examination is not necessary for patients with mild inflammation, it is beneficial when the diagnosis is in doubt, and it is indicated in patients who do not respond to supportive therapy when the disease course is complicated.