Original Research Article - (2023) Volume 24, Issue 1
Received: 14-Feb-2023, Manuscript No. IPP-23-15700 ; Editor assigned: 16-Feb-2023, Pre QC No. IPP-23-15700 ; Reviewed: 02-Mar-2023, QC No. IPP-23-15700 ; Revised: 04-Mar-2023, Manuscript No. IPP-23-15700 ; Published: 10-Mar-2023, DOI: 10.35841/1590-8577-24.2.792
Objectives Region based data of chronic pancreatitis (CP) in the North Indian Population were studied. We determined the incidence, prevalence, category distribution, region wise distribution and clinical data comparable with controls. Methods All consecutive patients in three years of time with tropical chronic pancreatitis (TCP) attending the Gastroenterology O.P.D. at S.G.P.G.I.M.S. Lucknow were included in the study as per inclusion criteria. Clinical diagnosis was based on phenotypic and radiological criteria and exocrine function tests. Patients giving the history of occasional alcohol consumption were excluded from the study. Results Mean age of patients was 49.9 ± 14.8 years, of which 105 (56.6%) were male. Maximum number of patients was in the age group of 20 to 40 years. The age of presentation of disease occurs in Ist decade. Among 150 cases of CP, 49% of TCP patients were recruited with no other clinical complications. The history of all the patients indicated the age of onset of the disease at 26.04±9.8 years, which is quite early but confound diagnosis was usually established at later stages of 35.8±16.7 years. Cigarette’s smoking was found quite common in 39% cases and diabetes gets precipitated in second and third decades of life in TCP patients that leads to complications in duration of calcification and pain. Conclusion The onset and incidence of CP cases diagnosed during life were found to be increased. Disease progression of CP patients was high in smokers as well as in the people having life style with comparable modifiable risk factors.
Pancreatitis is a heterogeneous disease with varied etiologies, defined as an inflammatory disease of the pancreas leading to morphological changes that typically causes pain and/or loss of function. Chronic Pancreatitis (CP), [Online Mendelian inheritance in man (OMIM) 167800], is characterized by irreversible destruction and fibrosis of the exocrine parenchyma, leading to exocrine pancreatic insufficiency and progressive endocrine failure leading to diabetes. Histological changes from the normal pancreatic architecture include irregular fibrosis, loss of acinar and islet cells, inflammatory cell infiltrates, and distorted and blocked ducts [1]. Patients present at a young age with recurrent abdominal pain and diabetes and follow an accelerated course of the disease even with no history of alcoholism [2, 3]. According to Mittal et al. [2002][4] 60-70% of patients with CP in developed countries have a long history of heavy alcohol consumption in male patients and unknown causes are responsible for 25% of cases, termed as idiopathic chronic pancreatitis (ICP). Tropical calcific pancreatitis (TCP, OMIM 608189) is a juvenile form of chronic calcific non-alcoholic pancreatitis, seen almost exclusively in developing countries of the tropical world [Barman et al. 2003]. In the simplest terms, TCP has been described as a disease with “pain in childhood, diabetes in puberty and death at the prime of life” [5].
The disease has most commonly been reported from Kerala but is prevalent throughout India. The prevalence of chronic pancreatitis in south India is very high and is estimated to affect 1 in 793, or 126/100000 in the population [6], a figure far greater than the 10-15/100000, reported from the western countries and 45.4 per 100000 from Japan [7, 8]. A recent population-based study in southern India has shown the prevalence of TCP to be 0.02% in the general population [9]. The study on acute exacerbation of chronic pancreatitis (CP) in tertiary care centre of North Indian population showed that Alcoholic chronic pancreatitis patients have lower milder disease course and low morbidity [10]. Arterial pseudoaneurysms were more commonly associated with Chronic Pancreatitis compared to Acute Pancreatitis with similar presentations, the study was conducted on 980 patients in which Pseudoaneurysms in patients with AP were associated more often with fluid collections (94.7% vs. 55.6%, P = 0.004) with more requirement of surgery compared to patients with CP (15.8% vs. 3.7%, P = 0.033)[11].
The etiology of TCP is unknown. Identified risk factors such as hypertriglyceridemia, hyperparathyroidism, obstruction of pancreatic duct by tumor, alcoholism and biliary stones are absent. It has been proposed that the consumption of cassava (Tapioca, Manilot esculents) or the protein energy diet may be the causative factor of the disease. But the disease may also affect the patients from higher economic background where malnutrition is unlikely. Gastrointestinal problems associated with malnutrition are very common in developing countries, and the diagnosis of CP can therefore be missed due to a low index of suspicion.
For this reason, we aimed to document the incidence and distribution of CP cases of North India.
Study Subjects
Clinically confirmed chronic pancreatitis cases from Department of Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS), Lucknow were recruited with exclusion criteria of alcoholic intake and familial history of pancreatic cancer.
Diagnosis: Inclusion criteria for TCP
• Radiological evidence of pancreatic intraductal calcification
• Non-alcoholic
• No family history of Pancreatitis
Exclusion criteria for TCP
• Absence of any other etiological factor like alcoholism, hypercalcaemia, gall stones
• Presence of pancreatic cancer
Inclusion criteria for Control
• Age and Sex matched control
• No history of Pancreatitis.
• Absence of any other cause for abdominal pain
Exclusion criteria for Control
• Presence of pancreatic cancer
• History of alcohol ingestion
Data was analyzed using software Statistical software for Social Sciences (SPSS, Version 17, Chicago, Illinois, USA) and EPI6. Chi- square and Students t-test were used to test the association between categorical and continuous variables. Fisher’s exact test was used if expected cell frequencies were lower than 5. Statistical inferences were based on the conventional level of statistical significance (P < 0.05)
The present study includes 150 cases of TCP and 150 age and sex matched controls from October 2009 to March 2013. (Figure 1A) represents the number of patients recruited each month over a period of 3 years. The maximum numbers of patient were recorded in the months of April and May. Mean age of patients was 49.9 ± 14.8 year, falling in the range of 10-55 years, of which 56.6% were male and 43.4% were female.
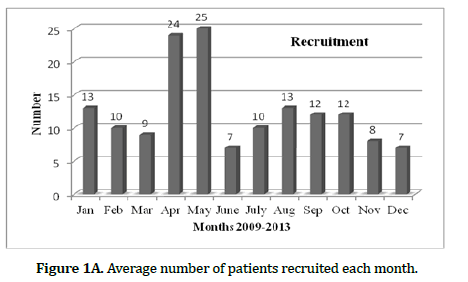
Figure 1A: Average number of patients recruited each month.
The categorization of patients was done on the basis of age at recruitment in years with maximum number of patients in the age group of 20 to 40 years. The age of presentation showing the occurrence of disease in second decade has been presented in (Figure 1B).
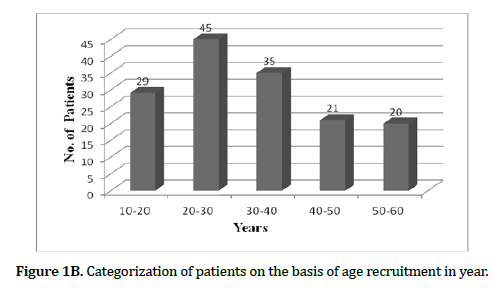
Figure 1B: Categorization of patients on the basis of age recruitment in year.
The 150 cases of TCP patients were further categorized in various groups like: 49% TCP patients with no other clinical complications, 42% TCP with diabetes mellitus with exocrine / endocrine insufficiency, 8% TCP with Pancreas Divisum (PD) and 1% of CP with pancreas divisum and diabetes mellitus. Though PD itself is not a cause of pancreatitis but it is one of the important clinical factors for TCP. These four groups are shown in (Figure 2).

Figure 2: Number of subjects studied in cases with category distribution.
The geographical distribution of TCP patients was also a reflection of the etiologies of the disease. 8% of the patients were from Basti and 7% from Gorakhpur. The results presented in (Figure 3) showed that there was a common denominator of the region, which reflects the poor standard of nutrition. Moreover, the climate of this region is favourable in progression of disease. Large segments of population in this region use insufficient amount of protein in their diet. Further, the quality of their lives is relatively poor. So, the factors closely associated with quality, environment, diet and congenital abnormality increase the threat of the disease. As the number of patients recruited was less, so it does not reflect the overall frequency.
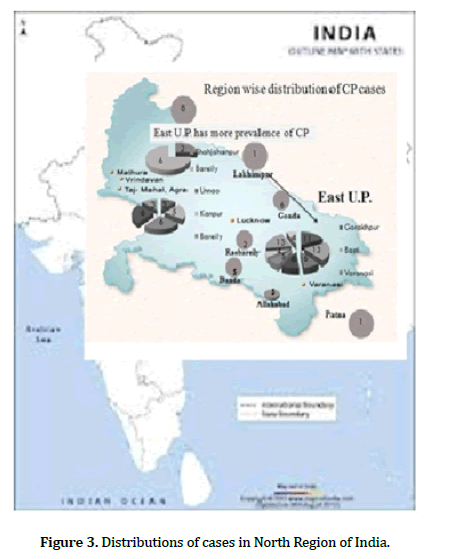
Figure 3: Distributions of cases in North Region of India.
The TCP patients (150) and controls (150) were further classified into three groups; depicted in (Figures 4A and 4B). Group I consisted of diabetics/non diabetics, group II contained smokers/Nonsmokers and group III consisted of family history/no family history of TCP. The ratio of diabetics/non-diabetics was 42:49 in TCP as compared to 28:72 in control groups. The percentage of smokers in TCP group was 39.3% more than the control group.
The number of individuals having classical risk factors viz diabetes; smoking and family history was found to be significantly higher in patients group shown in (Figure 4C).

Figure 4A: TCP patients group.
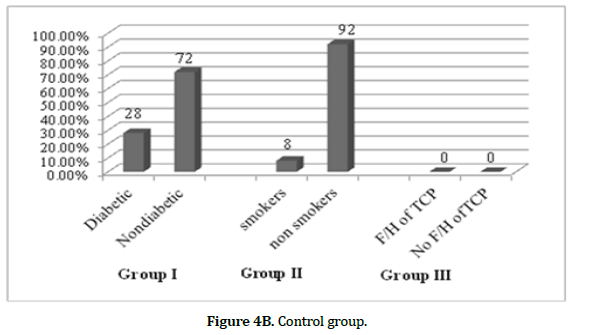
Figure 4B: Control group.
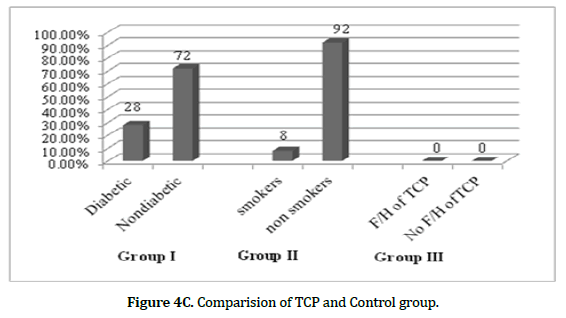
Figure 4C: Comparision of TCP and Control group.
The present study includes 105 males and 45 females in the TCP group, and 104 healthy males and 46 healthy females in control group. This shows an insignificant difference in male: female ratio in both the groups. However, a significant (p=0.001) difference for mean values of BMI and weight were noted between TCP patients and controls. A complete lipid profile like: triglycerides, total cholesterol, high density lipoprotein (HDL), cholesterol, low density lipoprotein (LDL) cholesterol and very low-density lipoprotein (VLDL), cholesterol in controls and patients are shown in Table 1. The values of total cholesterol, triglyceride (TG), VLDL and LDL were found significantly higher in CP patients than in controls with significant association. However, the level of HDL was found lower in TCP patients’ group. A higher percentage of smokers and diabetes was observed in patients’ group (p<0.001) compared to controls.
| Characteristics | Controls | TCP cases | P- value |
|---|---|---|---|
| N | 150 | 150 | - |
| Age | 36.86± 1.23 | 34.86± 1.183 | 0.2 17 |
| Sex (M:F) | 104:4 6 | 105:45 | 0.892 |
| Weight (kg) | 68. 19±9.634 | 56.23±13.230 | 0.001 |
| BMI (wt/ht2) | 25.16±3.15 | 23.3±3.25 | 0.001 |
| Diabetic: non diabetic | 42 :108 | 59:9 1 | 0.030 |
| Smoker: non smoker | 12:138 | 55:95 | 0.000 |
| Alcohalic:non-a lcoholic | 9:14 1 | 13:137 | 0.333 |
| Triglyceride ( 45-150 mg/dL) | 154.62±39.37 | 170.34±49.6 1 | 0.131 |
| Total Cholesterol (J 25-250mg/dL) | 95.34±27.47 | 151.18±43.03 | 0.001 |
| HDL-chol sterol (23-60mg'dL) | 39.34 ±7.79 | 36.62±7.678 | 0.023 |
| LDL-choksterol ( 92- l -ISmg'dL) | 38.41±7.76 | 86.35±3l.l l | 0.002 |
| YLDL- cholesterol ( I 0-30mgldL) | 19.54±6.6 1 | 25.96± 12.22 | 0.023 |
Table 1. Demographic and biochemical profile of controls and patients.
The male to female ratio in TCP patients was 2.3:1.0. The mean age of diagnosis was found to be 35.8±16.7. The presentation of the disease was 30.5 years in the calcific group and 23 years in the non-calcific group. Pain was the commonest presenting symptom, and it was present in 65% of patients. The age of onset of diabetes mellitus was 36.2±11.27 years. The duration of pain in calcific and non-calcific groups was found to be 2.19 years. The age of onset of disease and the presentation and duration of the symptom are given in Table 2. In addition, calcification was observed in 54% of patients. Steatorrhea was observed in 4.3% cases whereas Cholelithiasis was observed in 16.5% of cases. The history of all the patients indicated the age of onset of the disease to be 26.04±9.8 years which is quite early but confound diagnosis was usually established at later stages of life i.e.,35.8±16.7 yrs. Cigarette’s smoking was found quite common in 39% of cases and diabetes get precipitated in second and third decades of life in CP patients, that leads to complications in duration of calcification and pain.
| TCP patients(n) | 150 |
|---|---|
| Males (%) | 70 |
| Females (%) | 30 |
| Age (years; means ±s.d.) | 49.9±14.8 |
| Age at diagnosis(years; mean±s.d) | 35.8±16.7 |
| Age of onset (years; means±s.d) | 26.04±9.82 |
| Age of onset of pain (years; means±s.d) | 30.8±14.56 |
| Age (mean) at presentation calcific /non-calcific | 30.5/23 =1.3 |
| Pain (%) | 65.3 |
| Duration of pain calcific /non-calcific (Years) | 2.19 |
| Smokers (%) | 39 |
| No. of cigarettes( cig/day; mean±s.d) | 19.1±13.4 |
| BMI (kg/m2; mean±s.d.) | 23.3±3.25 |
| Age of onset of DM (means±s.d) | 36.2±11.27 |
| Complications of diabetes calcific /non-calcific (%) | 1.22 |
| Colelithiasis (%) | 16.5 |
| Dyslipidemia (%) | 5.2 |
| Pancreas divisum (%) | 8 |
| Autoimmune TCP (%) | 1.5 |
| Obstructive TCP (%) | 9.3 |
| Calcification (%) | 53.5 |
| Pseudo cysts (%) | 29.6 |
| Steatorrhea (%) | 4.3 |
Table 2. The age of onset of disease, age of presentation and duration of the symptom.
The diabetes related complications in TCP patients are given in (Table 3) showing the presence of ketosis, neuropathy and tuberculosis. The neuropathy and tuberculosis were present in 1% and 2% of patients.
| Complications | Percentage |
|---|---|
| Ketosis | 2 |
| Hypoglycemic episodes | - |
| K.W. Syndrome | - |
| Neuropathy | 1 |
| Retinopathy | - |
| Tuberculosis | 2 |
Table 3. Diabetes-complications.
In our studied subjects none of the TCP patients died in their thirties as a result of neuropathy or infections. Nearly 10% of TCP patients had to undergo surgery mostly for intractable pain occurring due to formation of pseudo cysts or common bile duct obstruction. Only 42% of TCP patients developed diabetes mellitus type 2 during the course of study.
Tropical Chronic Pancreatitis (TCP) is an incurable, persistent and inflammatory disease characterized by progressive and ultimately irreversible damage to both exocrine and endocrine functions of the pancreas. Genetic and biochemical evidences define a pathological pathway in which a sustained imbalance between intrapancreatic trypsinogen activation and trypsin inactivation results into the development of the disease. Most of the patients included in this study were from low socio-economic strata, possibly because of the location of this tertiary medical care hospital which caters the complicated and untreatable patients referred by medical doctors posted at various Government and private hospitals. The poor quality of lives of majority of patients is associated with inadequate intake of proteins and other nutrients [10].The factors closely associated with quality, environment, diet and congenital abnormality may augment the threat of the CP disease [11].
The results from the present study on TCP indicate that this disease develops in the first and second decades of life and is seen more commonly in males. Abdominal pain is the most common presenting symptom of TCP. The profile of TCP in the present study seems to be changing with time. Diabetes was found more commonly associated with TCP presentation. The development of pseudocysts is also the most common complication of TCP. One third to half of the patients with TCP had pancreatic calcification but the data obtained on frequency and pattern of calcification in TCP was heterogeneous as some centres reporting higher frequency of pancreatic calcification and ductal calculi whereas some having the pattern and frequency similar to alcohol related TCP [12]. Diabetes mellitus was significantly more common in calcific pancreatitis group as compared to the non-calcific group. The data from the present study reflect that calcification develops in late stages of TCP associated with advanced endocrine deficiency.
The biochemical profile of controls and TCP patients in the present study indicated increased levels of LDL, TG, VLDL and cholesterol and lower level of HDL; the data showing good agreement with those of others [13]. They have shown the occurrence of abnormal metabolism of triglycerides fractions in TCP patients of Polish origin.
The clinical features of TCP patients included in the present study indicated pain as a common feature in both the calcific and non-calcific groups. Goulden and his colleagues in [2013] [14] have reported the pathogenesis of pain in TCP patients as a major challenge to physicians, pain specialists, gastroenterologists and surgeons. They reported that upper abdominal pain and back pain with nausea and vomiting could be the main symptoms of TCP. In present study, other environmental factors such as smoking and consumption of alcohol etc increases complications in TCP patients. Similar observations have also been reported by Monique et al. [2010] [15]. They have found that cigarette smoking is a dose-dependent risk factor for acute pancreatitis, recurrent acute pancreatitis and chronic pancreatitis. However, some of chronic alcohol consumers develop recurrent acute pancreatitis but very heavy drinking associates with chronic pancreatitis [16].
The diabetes related complications in TCP patients have always been posing challenges towards treatment of TCP. The results from the present study have demonstrated that such TCP patients may be prone to ketosis, neuropathy and tuberculosis. No death of such patients was recorded. Similar observations have been reported by other workers in diabetic TCP patients [17, 18].
Authors are thankful to Suresh Gyan Vihar University Mahal, Jagatpura, Jaipur for academic platform and Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), Lucknow, India for providing infrastructural facilities.
None
None
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Singh S, Sharma B, Choudhuri G. Clinical study of chronic pancreatitis patients in North Indian population and its outcome. JOP. J Pancreas. (2023) 24:792.
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.