Keywords
cervical cancer screening, ethnicity, immigrants,
minority, Pap smear
Introduction
Cervical cancer is the second commonest cancer among
women worldwide. In the industrialised nations, the
age-standardised incidence rate is 7.7 in 100 000 and
the mortality rate is 3.6 in 100 000 women per year
(Parkin et al, 2005). Cervical cancer screening is based
mainly on the Papanicolaou test (Pap smear), which
identifies pre-cancerous lesions on a woman’s cervix.
The diagnosis necessitates early treatment to prevent
advanced-stage cervical cancer or death (Swiss Society
of Obstetrics and Gynecology, 2004; American Cancer
Society, 2005). Currently the World Health Organization
(2004) and the European Commission (2006)
recommend systematic programmes for cervical cancer
screening, as this is a cost-effective method of reducing
both the incidence andmortality rates of cervical cancer.
Organised Pap smear screening means that cervical
cancer has become a preventable disease. Invasive
squamous-cell cancer is considered to represent a
failure of screening (Garner, 2003). Furthermore, the
introduction of human papillomavirus (HPV) vaccines
has contributed to a reduction in the incidence and
mortality of the disease (Beres, 2008).
In Switzerland, the European-standardised incidence
and mortality rates of cervical cancer are 7 in 100 000
and 1.6 in 100 000 women per year, respectively. This
results in an average of 90 deaths from cervical cancer
each year (Association of Swiss Cancer Registries,
2006). One of the aims of the National Cancer Control
Programme for Switzerland 2005–2010 is the improvement
of early detection of cervical cancer (Schopper
and Obrist, 2005).
The international literature shows that women
in ethnic-minority groups are at risk for underutilisation
of preventive services (Rodriguez et al,
2005; Tammemagi, 2007). Immigrant women often
present with advanced-stage cancer and are treated
less aggressively compared with the majority population
(Rodriguez et al, 2005). In several countries
there has been increasing awareness of health-related
inequalities between minority groups and the majority
population (Smedley et al, 2003).
Wanner et al (2001), in an earlier survey in
Switzerland, did not find any difference between Swiss
and immigrant women with regard to mortality from cervical cancer. However, those authors recommend
that their findings be interpreted with caution because,
for example, the accuracy of diagnosis was limited,
and deaths in cases of re-migration to the country of
origin were not taken into account. Self-reported use
of Pap smears in Switzerland is significantly lower for
less educated women (Raymond et al, 1996; Huwiler
et al, 2002), for women over 65 years of age (Zemp,
2000) and for immigrants (Raymond et al, 1996; Vranjes
et al, 1996; Wanner et al, 1998).
Studies in the UK, the USA and Australia have
investigated the self-reported use of Pap smears among
immigrant women, often by comparison with use among
the native population. Although there is generally a
lower rate of utilisation of cervical cancer screening by
immigrant women, in one study the effect of having
been born in another country (Goel et al, 2003; Taylor
et al, 2003) disappeared after controlling for sociodemographic
variables, including income, education,
employment status, health insurance and marital status
(Rodriguez et al, 2005). Swan et al (2003) suggested
that women who have migrated to the USA within the
last 10 years should be one of the groups targeted for
intervention in order to increase participation in
cervical cancer screening.
Not speaking the official language is also known to
be a barrier to cancer screening (Taylor et al, 2001;
Jacobs et al, 2003; De Alba et al, 2004).
The impact of race and/or ethnic origin has been
highlighted by David et al (2000) in Germany. They
found that Turkish women were less aware of the
existence of the Pap smear than German women.
Over the last few years, there has been increasing
awareness of health-related inequalities. According to
Fiscella (2002), such inequalities result from interactions
between socio-economic status, racism, segregation,
culture, health behaviours and beliefs, access to
and quality of healthcare, and genetics. Studies in
Switzerland have confirmed that in that country, too,
there is a relationship between low socio-economic
status and poor health. The self-perceived state of health
among immigrants in Switzerland is slightly worse
than that among Swiss nationals (Bischoff andWanner,
2008). In addition, immigrants use the healthcare system
more often for accidents and illnesses than for disease
prevention. It may be that prevention programmes are not easily accessible to certain immigrant groups (Swiss
Federal Office of Public Health, 2002).
During the last three decades, Switzerland has
become a culturally diverse country. Around 22% of
people currently living in Switzerland are immigrants,
defined as people with foreign nationality (Rausa et al,
2006). Of the 1.7 million immigrants in Switzerland,
22% are Italian, 14% are from the former Yugoslavia
(Serbia-Montenegro, Bosnia-Herzegovina and Kosovo),
10% are Portuguese, 8% are German, 6% are Spanish
and 4% are French. The remaining 36% consist of
smaller groups of other nationalities.
Against this background of increased diversity, we
investigated whether there are inequalities in the uptake
of cervical cancer screening between the main immigrant
groups and Swiss nationals. We analysed baseline
data from the Swiss Health Survey (SHS; Bischoff
and Wanner, 2008) in order to detect variability in the
self-reported use of the Pap smear.
Methods
Data source and population studied
The SHS is a household survey of health and illness,
health-related behaviour and its determinants, and
health service utilisation, and includes information on
the socio-demographic characteristics of respondents.
In 2002, on behalf of the Swiss Federal StatisticalOffice
(SFSO), a telephone interview was conducted in three
of the four official languages in Switzerland, namely
German, French and Italian. The people who were
interviewed were Swiss residents aged 15 years or over.
The stratified random sample consisted of 32 868 individuals,
and the participation rate was 64%, resulting
in a final sample consisting of 19 706 residents (Graf
and Renfer, 2005). Stratification was undertaken according
to the administrative regions of residence (the
cantons) in order to increase the sample for further
cantonal analyses.Trained staff performed the interviews
in four waves, corresponding to the four seasons. In
certain circumstances (e.g. in the case of language or
hearing problems) the interview was conducted using
a proxy for the index person (5.7%). Excluded from
the sample were asylum seekers, individuals who did
not speak one of the three interview languages, and
people in institutions such as hospitals, homes for elderly
people, and prisons. At the time of the survey, approximately
2.5% of the total population lived in collective
households, and the proportion of asylum seekers was
less than 1%. Even if these figures are low, the exclusion
of these groups may lead to an inaccurate estimate of
the behaviours of non-European populations.
A total of 10 046 women, including all nationalities,
aged 20 years or over, were asked whether they had ever had a Pap smear. Women who had had a hysterectomy
were not excluded, as they are also recommended
to have a regular Pap smear, albeit at less
frequent intervals (Swiss Society of Obstetrics and
Gynecology, 2004).
The analysed subsample of our study consisted of
women from the following major groups by nationality
(large to small): Italian (n = 306), German (n = 203),
the former Yugoslavia (Serbia,Montenegro, Macedonia,
Bosnia and Herzegovina, and Croatia; n = 89),
Portuguese (n = 80), Spanish (n = 78) and French (n =
72), with Swiss as controls (n = 9 011). This gave a total
sample size of 9839. Foreigners of other citizenship
(n = 207) were excluded.
Variables and analyses
Descriptive statistics, Chi-square tests (Pearson’s) and
a logistic regression analysis were performed. The
dichotomous variable of interest was ‘never/ever had
a Pap smear.’ The main independent variable was
‘immigrant group’, with the categories according to
country of origin (Italy, Germany, former Yugoslavia,
Portugal, Spain and France). Women of both Swiss
and another nationality were considered to be Swiss.
Based on international and Swiss studies (Raymond
et al, 1996; Zemp, 2000; Huwiler et al, 2002; De Alba
et al, 2005; Rodriguez et al, 2005), five further independent
variables were considered, namely age, level
of education, occupational status, household income
and area of residence.
Age was used as a continuous variable in the logistic
regression analysis, and as both continuous and categorical
(20–34, 35–49, 50–64 and � 65 years) variables
in the descriptive statistics.
The variables ‘level of education’ and ‘occupational
status’ are composites of other variables (Swiss Federal
Statistical Office, 2003). Level of education consisted
of four different categories, namely no education, primary
school, secondary school (e.g. apprenticeship)
and tertiary education. Occupational status was also
divided into four categories, namely manual unskilled,
blue collar (e.g. independent craftsmen, farmers), white
collar, and management (higher qualified professionals).
The variable ‘income’ refers to equivalent income.
In the research literature this is considered to indicate
the distribution of earnings, and is relevant for international
comparisons and discussions of socio-political
implications (Swiss Federal Statistical Office, 2004).
The variable ‘area of residence’ consisted of Region of
Lake Geneva,BernerMittelland,North-West Switzerland,
Zurich, East Switzerland, Central Switzerland and
Ticino.
To reduce the impact of non-responders and to
improve statistical estimates, data from the telephone
interviews were weighted by the SFSO using non response rates (Graf and Renfer, 2005), taking into
account nationality, gender, age and area of residence
(canton or region). Uni- and bivariate calculations
were weighted using a factor calculated by the SFSO.
In the multivariate analysis, the four relevant weighting
variables were included in the regression model.
Signs of multicollinearity were checked and analyses
were run with the Statistical Package for Social Sciences
(SPSS), using the correlations of estimates test (Chan,
2004). Correlations of any two variables were checked
and showed moderate to low correlations. All procedures
were run on SPSS 13, and the level of significance
was set at P < 0.05.
Ethical considerations
The Swiss Health Survey was conducted on behalf of
the Swiss Confederation by the SFSO, according to the
principles and regulation of the Ethics Board of Public
Statistics (Switzerland Schweizerische Gesellschaft fu¨r
Statistik, 2008) Data were de-identified. We obtained
permission to analyse the data via contract #04/100/
05.04.04 (entitled ‘Towards improving outcomes for
migrant patients with chronic illness’) with the SFSO.
Results
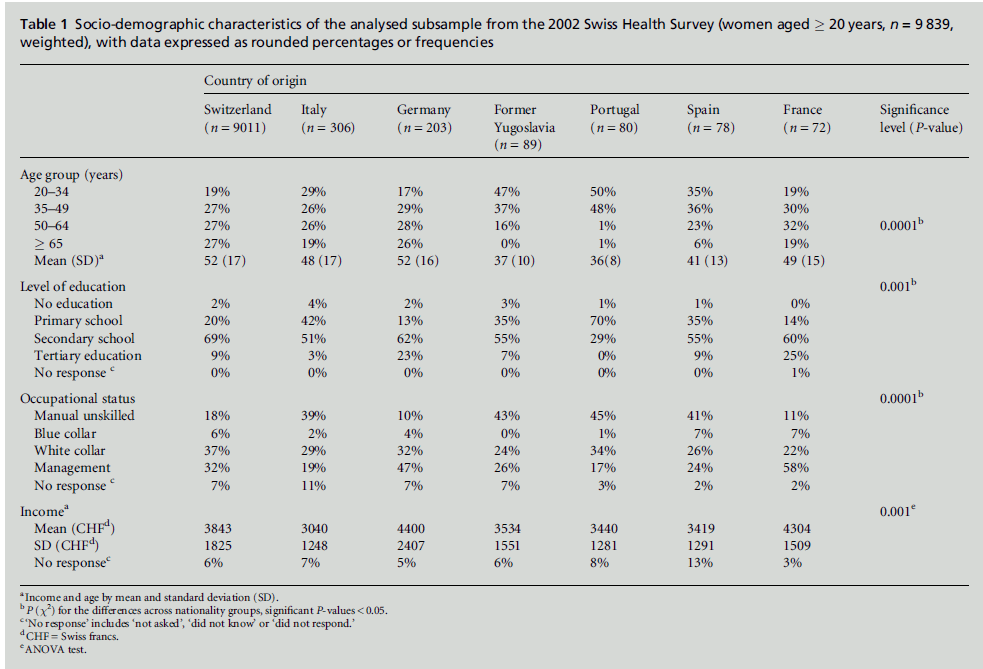
The socio-demographic characteristics of the subsample
are presented in Table 1. Swiss and German women
showed a similar distribution across all age categories,
as did Italian and French women. Compared with
these four nationality groups, women from the former
Yugoslavia, Spain and Portugal had a lower mean age.
French and German women were the most highly
educated, and Portuguese women were the least well
educated. With regard to occupation, women from
Portugal, the former Yugoslavia, Spain and Italy had
the highest percentage of individuals in the blue collar
category. Women from Germany had the highest
household income, followed by those from France and
then those from Switzerland. The other four groups
had lower household incomes, with Italian women
having the lowest.
Pap smear
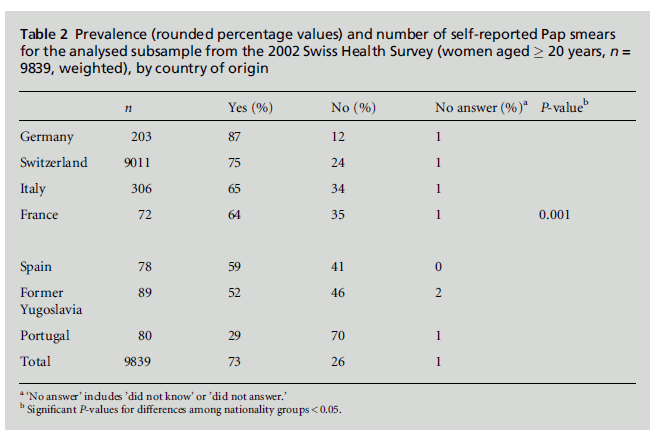
Table 2 shows theweighted, bivariate results of the Pap
smear question for all nationality groups. A high
proportion of women from Portugal (70%), the former
Yugoslavia (46%), Spain (41%), France (35%) and
Italy (34%) said that they had never had a Pap smear.
This proportion was lower for women from the Swiss
reference group (24%) and from Germany (12%).
These differences are statistically significant.
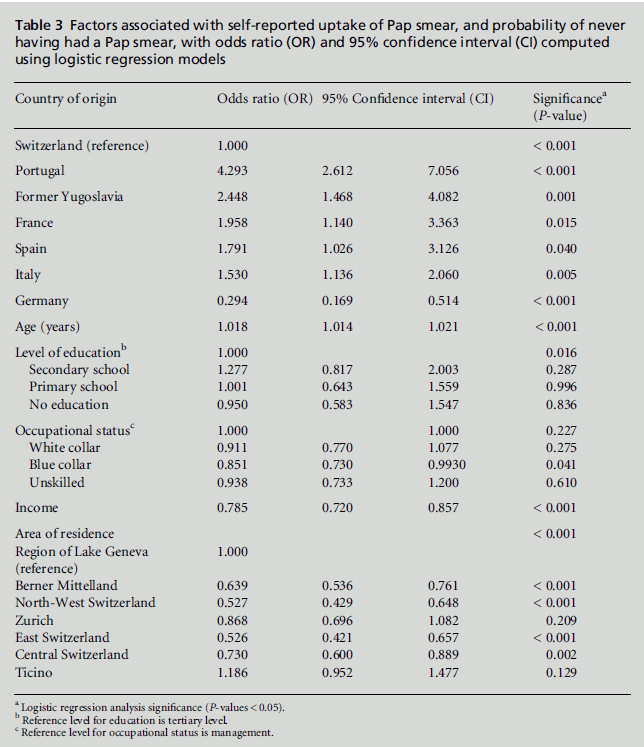
Table 3 shows the results of the logistic regression
analysis. Beforehand, collinearity testing produced no
strong correlation between the independent variables.
The probability of never having had a Pap smear
depended significantly on women’s nationality, even
when adjusted for age, level of education, occupational
status, income and area of residence (P < 0.001).
Most of the immigrant groups were less likely to
have been screened than the Swiss comparison group.
This was the case for women from Portugal (odds ratio
(OR) = 4.29) ), the former Yugoslavia (OR = 2.45),
France (OR=1.96), Spain (OR=1.79) and Italy (OR=
1.53). Only women from Germany had been screened
more often (OR = 0.29). The probability of never
having had a Pap smear increasedwith age (OR = 1.02),
and decreased with higher levels of education (OR =
0.089) and higher income (OR= 0.78). There was no
association between occupation and the probability of
never having had cervical cancer screening (OR =
1.05), but there were significant associations between
the uptake of Pap smears and certain areas of residence.
Discussion
According to the Global Health Watch, migrants tend
to experience poorer access to healthcare compared
with the rest of the population (People’s Health Movement,
2008). The epidemic of chronic diseases, including
cancer, is now considered to be a major challenge
among the ethnically diverse populations in Europe
(Bhopal, 2009). Cervical cancer is a case in point.
Uptake of the Pap smear is an important element of
preventive behaviour and an indicator of healthcare
accessibility for women. In this study we investigated
cervical cancer screening among different immigrant
groups in Switzerland. We analysed the Swiss Health
Survey data and found significant variability in the
self-reported use of Pap smears among six foreign
nationality groups living in Switzerland, namely women
from Italy, Germany, the former Yugoslavia, Portugal,
Spain and France. Our results are consistent with the
increasing body of research that documents healthcare
inequalities between minority (immigrants and ethnic
minorities) and majority (mainstream and local) populations
(Fiscella et al, 2002; Smedley et al, 2003; Bhopal,
2007). These inequalities persist even after controlling
for socio-demographic factors, including age, level of
education, income and area of residence, especially
with regard to women from Portugal, the former
Yugoslavia and Italy.
Table 1: Socio-demographic characteristics of the analysed subsample from the 2002 Swiss Health Survey (women aged � 20 years, n = 9 839,
weighted), with data expressed as rounded percentages or frequencies
Table 2:Prevalence (rounded percentage values) and number of self-reported Pap smears
for the analysed subsample from the 2002 Swiss Health Survey (women aged � 20 years, n =
9839, weighted), by country of origin.
Our findings correspond to those of international
studies which show that immigrant women are less
likely to undergo cervical cancer screening compared
with women born in the country being studied (Goel
et al, 2003). In Canada, ethnic-minority groups are less commonly screened for cervical cancer than women
from the majority population (Vissandje´e and Dupe´re´,
2002), even after adjusting for socio-demographic and
health characteristics (Quan et al, 2006). In Australia,
the number of immigrant women from southern
Europe who reported that they had ever had a Pap
smear was significantly lower than that for the majority
population (Taylor et al, 2001). In California, Latinas
were less likely ever to have had a Pap smear than non-
Latina whites (Rodriguez et al, 2005). However, in
contrast, the California Health Interview Survey 2001
found no significant differences in the proportions of
black, white and Hispanic women who had ever had a
Pap smear (De Alba et al, 2004). This finding may
reflect the effectiveness of the Californian National
Breast and Cervical Cancer Early Detection Program
(Centers for Disease Control and Prevention, 2006),
which supports various organisations in their efforts
to overcome disparities by implementing outreach
and education programmes.
Both Swiss and international studies (from Canada
and the USA) have shown that women of lower socioeconomic
status, as measured mainly by level of education
and income, have less access to cervical cancer
screening (Huwiler et al, 2002; Vissandje´e and Dupe´re´,
2002; Parikh et al, 2003). Education raises awareness
of the importance of regular health checks, and empowers
people to take control over their own lives
(Sabates and Feinstein, 2006). Wolff et al (2005, p. 2153)
have described the role of low income in an insurancebased
system: ‘Poor people choose an insurance type with a high contribution in order to keep their premium
low, which causes major financial problems
when healthcare is actually needed.’ In Switzerland,
cervical cancer screening requires a personal financial
contribution, and is therefore more likely to be neglected
by women on a low income.
Our analysis provides evidence that ethnicity, as
defined by country of origin (Stronks et al, 2008), in
combination with income and level of education,
affects uptake of the Pap smear by immigrant women
(Bischoff and Wanner, 2008; Fontana and Bischoff,
2008). Therefore cervical screening policies need to
take into account both ethnicity/immigrant grouprelated
and socio-demographic inequalities (Qi et al,
2006; Ingleby, 2008; Vitorino, 2009).
Cervical cancer screening policies in
Europe
It can be assumed that the attitudes of immigrants
living in Switzerland towards cancer screening are also
influenced by screening practices in their country of
birth. There is some evidence that television channels
and newspaper campaigns that are received from the
country of birth influence immigrant women’s attitudes.
The most commonly cited source of health
information is that provided in the native language
commonly used by ethnic minorities (O’Malley et al,
1999), through television, magazines and newspapers
(Brunton and Thomas, 2002). The results of media
research on the topic are inconsistent. An Austrian study (Growth from KnowledgeMarket Research, 2008)
indicated that immigrants prefer to watch television
news from their country of birth (74%) compared
with other programmes, whereas a German media
group reported that most immigrants except Turkish
nationals (14%) show the same behaviour as the native
population (Handelsblatt, 2007). However, the influence
of an Italian-language media campaign that was
directed towards the Italian community in Australia
did not significantly increase attendance at screening
services (Page et al, 2005).
Table 3:Factors associated with self-reported uptake of Pap smear, and probability of never
having had a Pap smear, with odds ratio (OR) and 95% confidence interval (CI) computed
using logistic regression models.
The European Commission (2006) recommends that
cervical cancer screening should be offered through a
population-based organised programme. This includes
personal letters of invitation to have a Pap test, and a
mechanism for systematic quality control. A survey
of cervical cancer screening policies in 18 European
countries showed that only a few of them met the
recommendations of the European Commission (Anttila
et al, 2004). In Germany, 80% of the population have
undergone cervical cancer screening within the last
three years (van Ballegooijen et al, 2000). Germany has
an opportunistic system,with no organised programme, and experts suggest a one-year interval between tests.
In Germany, both Pap smear tests and human papillomavirus
(HPV) vaccinations are cost-free (Deutsche
Krebshilfe, 2008), although so far there has been no
nationwide organised screening. No national recommendations
or data were found for Portugal, but
regional data showed a participation rate of 37% in
the last three years (van Ballegooijen et al, 2000). In
Catalonia (Spain), according to regional self-reported
data from the 1994 Catalan Health Survey, 42% of
women have a Pap test at some stage (Borras et al,
1999). In Italy, some well-organised screening programmes
are available on a regional basis, but these are
concentrated in the northern part of the country.
Overall, there is 50% coverage in Italy (Segnan et al,
2000; van Ballegooijen et al, 2000). In France, some
systematic programmes have been implemented, with
50–69% of the population having had a Pap test
within the last three years (Anttila et al, 2004). There
are very few data for the former Yugoslavia. In two
cities in Serbia, 66% of women have had a test at some
stage (n = 775; Kesic et al, 2005; Markovic et al, 2005).
In general, it seems that cervical cancer screening
policies in most of the countries that have been
examined differ, although the fact that the methodology
of the studies also differs must be taken into
account. Nevertheless, some of the findings are striking.
There are very few data from Portugal and the
former Yugoslavia about uptake of cervical cancer
screening, and Germany has the highest screening
rate. Switzerland has an opportunistic approach to
cervical cancer screening. One problem with opportunistic
systems is that they may not cover the whole
population adequately, possibly missing people with
reduced access to information (Bhopal, 2007), including,
among others, immigrants. However, it is sometimes
argued that some women in Switzerland undergo
too many Pap tests, incurring unnecessary costs for
the health system (Biedermann, 2005).
Promoting equal access to cervical
cancer screening in Switzerland
As part of the move to achieve a system of equal health
opportunities for everyone living in Switzerland (World
Health Organization, 1998; Saladin et al, 2007), both
unequal access to cervical cancer screening and overscreening
must be eliminated. The aim of the National
Cancer Control Programme 2005–2010 is to improve
the early detection of cervical cancer (Schopper and
Obrist, 2005). Prevention and healthcare promotion,
healthcare provision, and research on the health and
healthcare needs of immigrants are three of five goals
in the Migration and Public Health Strategy 2002–
2007 (Swiss Federal Office of Public Health, 2002). A
systematic screening programme, as recommended by the European Commission and the World Health
Organization, adapted to the needs of still underserved
population groups such as immigrants, could
bring these three concepts together.
To achieve an organised and culturally sensitive
screening programme, letters of invitation to attend
screening services should be sent toimmigrantwomen
in their first language (Vellozzi et al, 1996), and the
cost of Pap smears should be deducted from any
personal financial contribution (Biedermann, 2005).
Loerzel and Bushy (2005) distinguish between system
barriers, such as insurance, usual source of care, low
income, and communication within the healthcare system,
and human barriers, such as low level of education,
fear of the test, lack of knowledge about cervical
cancer, and cultural beliefs. In Germany, David et al
(2000) found that Turkish women are less aware of
the Pap test than are German women. Garbers and
Chiasson (2004) reported that Latina immigrants in
New York have difficulty in understanding medical
information, even when it is written in Spanish. In
Israel, feelings of embarrassment and the belief that
there is no cure for cancer were identified as barriers to
breast cancer screening among Muslim women (Aziza
and Cohen, 2006). The Institute ofMedicine states that,
among numerous reasons for inequalities in access to
screening services, bias, prejudice and stereotyping on
the part of health professionals may contribute to
differences in and lower quality of care (Smedley et al,
2003). Despite providers’ best intentions, women who
belong to minorities can experience negative racial
attitudes that are unconsciouslydemonstrated by healthcare
professionals.
Giarratano et al (2005) have described a programme
designed to improve access to breast and cervical cancer
screening for ethnic-minority, under-served women
in the USA. Community lay health educators deliver
their message in a spiritual context, and empower
women to take responsibility for their health through
education, self-care practices and annual screening.
Culturally competent advanced practice nurses then
follow up women who have an appointment for Pap
testing.
In Switzerland, as part of the national Migration
and Health Strategy (Swiss Federal Office of Public
Health, 2002), efforts should be made to find out how
to increase access to cervical cancer screening for underserved
immigrant women and other minorities, including
the elderly and women of low socio-economic
status. A combination of strategies may be desirable,
including the mass media, direct bilingual mailings,
provider education and focus groups (Vellozzi et al,
1996; Markovic et al, 2005). The implementation of an
immigrant group-specific, culturally sensitive and organised
cervical cancer screening programme in Switzerland
will require collaboration among different healthcare
professionals with immigrant communities.
Study limitations
Our study has several limitations. Some of these are
due to the fact that the Swiss Health Survey was not
developed with a view to examining immigrant-specific
issues (Bischoff and Wanner, 2003) The participation
rate according to immigrant group was not measured
(Graf and Renfer, 2005). However, it is known that this
rate is lower amongimmigrant groups than among the
native population, in particular among recent migrants
and those who do not speak one of the official languages
(Wiking et al, 2004). One important limitation of our
study was the exclusion of immigrants who do not
speak one of the three official languages, namely German,
French or Italian. Undocumented immigrants, asylum
seekers and people who have recently moved to
Switzerland were also not represented in the study
population. The latter probably do not have a landline
telephone in the early months following their arrival.
A recent Swiss study showed that only a third of undocumented
immigrants in Geneva had ever had a
Pap smear (Wolff et al, 2005). We assume that if the
Swiss Health Survey had included a higher proportion
of immigrants who were less integrated, and if we had
also had access to clinical data on cervical cancer
screening, we would have found an even lower rate
of uptake of the Pap smear among the immigrant
population.
Conclusions
In our survey, five of the six immigrant groups had
lower self-reported rates of participation in cervical
cancer screening than the Swiss group. This is unacceptable
both in terms of cost-effective preventive
measures, and in terms of the goal of equity of access
to healthcare. The introduction of a systematic cervical
cancer screening programme tailored to specific
immigrant groups such as those from Portugal, the
former Yugoslavia and Italy would benefit immigrant
women and would be an important step towards the
reduction of health inequalities and towards equity in
the Swiss healthcare system.
CONFLICTS OF INTEREST
None.
References
- American Cancer Society (2005) What Causes Cancer of theCervix? Can it be Prevented? www.cancer.org/docroot/CRI/CRI_0.asp (accessed 20 June 2006).
- Anttila A, Ronco G, Clifford G et al (2004) Cervical cancerscreening programmes and policies in 18 European countries.British Journal of Cancer 91:935–41.
- Association of Swiss Cancer Registries (2006) ASCR Statistics;www.vskr.ch (accessed 21 June 2006).
- Aziza F and Cohen M (2006) Health beliefs and rates ofbreast cancer screening among Arab women. Journal ofWomen’s Health 15:520–30.
- Beres S (2008) Filling the gaps to fight cervical cancer.Journal of the National Cancer Institute 100:526–8.
- Bhopal R (ed) (2007) Ethnicity, Race and Health in MulticulturalSocieties. Foundations for better epidemiology, publichealth and health care, Oxford: Oxford University Press.
- Bhopal R (2009) Chronic diseases in Europe’s migrant andethnic minorities: challenges, solutions and a vision.European Journal of Public Health 19:140–3.
- Biedermann A (2005) Optimierung der Rahmenbedingungenfu¨r das Krebs Screening in der Schweiz. VorschlagzurDiskussion. VorarbeitenzurFormulierungeinernationalenStrategiefu¨r das Krebs Screening. Bern: Oncosuisse.
- Bischoff A and Wanner P (2003) Gesundheitsmonitoringfu¨rMigrantInnen: Sinnvoll? Machbar? Realistisch? Neuchaˆtel:Swiss Forum for Migration and Population Studies.
- Bischoff A and Wanner P (2008) The self-reported health ofimmigrant groups in Switzerland. Journal of Immigrantand Minority Health 10:325–35.
- Borras JM, Guillen M, Sanchez V et al (1999) Educationallevel, voluntary private health insurance and opportunisticcancer screening among women in Catalonia (Spain).European Journal of Cancer Prevention 8:427–34.
- Brunton M and Thomas DR (2002) Privacy or life: how dowomen find out about screening mammography services?New Zealand Medical Journal 115:U168.
- Centers for Disease Control and Prevention (2006) NationalBreast and Cervical Cancer Early Detection Program;www.cdc.gov/cancer/nbccedp (accessed 10 July 2006).
- Chan YH (2004) Biostatistics 201: linear regression analysis.Singapore Medical Journal 45:55–61.
- David M, Borde T and Kentenich H (2000) Knowledgeamong German and Turkish women about specificallyfemale bodily functions, contraception, preventative medicalexaminations and menopause. Ethnicity and Health5:101–12.
- De Alba I, Sweningson JM, Chandy C et al (2004) Impact ofEnglish language proficiency on receipt of Pap smearsamong Hispanics. Journal of General Internal Medicine19:967–70.
- De Alba I, Ngo-Metzger Q, Sweningson JM et al (2005) Papsmear use in California: are we closing the racial/ethnicgap? Preventive Medicine 40:747–55.
- Deutsche Krebshilfe (2008) Deutsche Krebshilfe; www.krebshilfe.de/gebaermutterhalskrebs.htm (accessed 22December 2008).
- European Commission (2006) Proposal for a Council Recommendationon Cancer Screening. Brussels: Commissionof the European Communities.
- Fiscella K (2002) Using existing measures to monitor minorityhealthcare quality. In: Improving Healthcare Qualityfor Minority Patients. Washington, DC: National QualityForum.
- Fiscella K, Franks P, Doescher MP et al (2002) Disparities inhealth care by race, ethnicity, and language among theinsured: findings from a national sample. Medical Care40:52–9.
- Fontana M and Bischoff A (2008) Uptake of breast cancerscreening measures among immigrant and Swiss womenin Switzerland. Swiss Medical Weekly 138:752–8.
- Garbers S and Chiasson M (2004) Inadequate FunctionalHealth Literacy in Spanish as a Barrier to Cervical Cancer
- Garner E (2003) Cervical cancer disparities in screening, treatment and survival. Cancer Epidemiology Biomarkers
- Giarratano G, Bustamante-Forest R and Carter C (2005) Amulticultural and multilingual outreach program forcervical and breast screening. Journal of Obstetric, Gynecologicand Neonatal Nursing 34:395–402.
- Goel MS, Wee CC, McCarthy EP et al (2003) Racial andethnic disparities in cancer screening: the importance offoreign birth as a barrier to care. Journal of GeneralInternal Medicine 18:1028–35.
- Graf E and Renfer J (2005) Enqueˆte Suisse sur la Sante´ 2002:plan d’e´chantillonnage, ponde´rationet estimation de lapre´cision. Neuchaˆtel: Swiss Federal Statistical Office.
- Growth from Knowledge Market Research (2008) GfKAustria; https://mediaresearch.orf.at/c_studien/Migranten_Fernsehen_2007.pdf (accessed 15 May 2009).
- Handelsblatt (2007) Mediennutzung von Einwanderern; www.handelsblatt.com/unternehmen/it-medien (accessed 17May 2009).
- Huwiler K, Bichsel M, Junker C et al (2002) SozialeUngleichheit und Gesundheit in der Schweiz. EineSpezialauswertungder SchweizerischenGesundheitsbefragung1997. Neuchaˆtel: Swiss Federal Statistical Office.
- Ingleby D (2008) Presentation on the Council of Europe’sCommittee of Experts on Mobility, Migration and Access toHealth Care. Meeting on Social Determinants and HealthInequalities, 1–2 December 2008, Luxembourg.
- Jacobs E, Agger-Gupta N, Chen HM et al (2003) LanguageBarriers in Health Care Settings: an annotated bibliographyof the research literature. Los Angeles, CA: The CaliforniaEndowment.
- Kesic V, Markovic M, Matejic B et al (2005) Awarenessof cervical cancer screening among women in Serbia.Gynecologic Oncology 99(Suppl.1):S222–5.
- Loerzel VW and Bushy A (2005) Interventions that addresscancer health disparities in women. Family and CommunityHealth 28:79–89.
- Markovic M, Kesic V, Topic L et al (2005) Barriers to cervicalcancer screening: a qualitative study with women inSerbia. Social Science and Medicine 61:2528–35.
- O’Malley AS, Kerner JF and Johnson L (1999) Are we gettingthe message out to all? Health information sources andethnicity. American Journal of Preventive Medicine 17:198–202.
- Page A, Morrell S, Tewson R et al (2005) Mammographyscreening participation: effects of a media campaigntargeting Italian-speaking women. Australian and NewZealand Journal of Public Health 29:365–71.
- Parikh S, Brennan P and Boffetta P (2003) Meta-analysis ofsocial inequality and the risk of cervical cancer. InternationalJournal of Cancer 105:687–91.
- Parkin DM, Bray F, Ferlay J et al (2005) Global cancerstatistics, 2002. CA: a Cancer Journal for Clinicians 55:74–108.
- People’s Health Movement (2008) Global Health Watch 2:an alternative world health report. London: Zed Books.
- Qi V, Phillips S and Hopman W (2006) Determinants ofa healthy lifestyle and use of preventive screening inCanada. BMC Public Health, 6:275.
- Quan H, Fong A, De CosterCet al (2006) Variation in healthservices utilization among ethnic populations. CanadianMedical Association Journal 174:787–91.
- Rausa F, Reist S, Capezzali E et al (2006) Ausla¨nderinnenund Ausla¨nder in der Schweiz. Bericht 2006. Neuchaˆtel:Bundesamtfu¨rStatistik (BFS).
- Raymond L, Bouchardy C and DroinN(1996) Participationdes femmes suisses au de´pistage du cancer du col ute´rin.SchweizerKrebsbulletin 16:27–30.
- Rodriguez MA, Ward LM and Perez-Stable EJ (2005) Breastand cervical cancer screening: impact of health insurancestatus, ethnicity, and nativity of Latinas. Annals of FamilyMedicine 3:235–41.
- Sabates R and Feinstein L (2006) The role of education in theuptake of preventative health care: the case of cervicalscreening in Britain. Social Science and Medicine 62:2998–3010.
- Saladin P, Buhlmann R, Dahinden D et al (2007) Diversityand Equality of Opportunity. Fundamentals for effectiveaction in the microcosm of the health care institution. Bern:Federal Office of Public Health in collaboration with theSwiss Hospital Association.
- Schopper D and Obrist R (2005) NationalesKrebsprogrammfu¨r die Schweiz 2005–2010. Bern: Oncosuisse.
- SchweizerischeGesellschaftfu¨rStatistik (2008) EthikReglement – OeffentlicheStatistik der Schweiz. Neuchaˆtel:Bundesamtfu¨rStatistik.
- Segnan N, Ronco G and Ciatto S (2000) Cervical cancerscreening in Italy. European Journal of Cancer 36:2235–9.
- Smedley BD, Stith AY and Nelson AR (2003) UnequalTreatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press.
- Stronks K, Kulu-Glasgow I and Agyemang C (2008) Theutility of ’country of birth’ for the classification of ethnicgroups in health research: the Dutch experience. Ethnicityand Health:1–14.
- Swan J, Breen N, Coates RJ et al (2003) Progress in cancerscreening practices in the United States: results from the2000 National Health Interview Survey. Cancer 97:1528–40.
- Swiss Federal Office of Public Health (2002) Migration andPublic Health: the Confederation’s strategic orientation 2002–2006; www.bag.admin.ch/themen/gesundheitspolitik/00394/00395/04393/index.html?lang=en (accessed 7 August2009).
- Swiss Federal Statistical Office (2003) SchweizerischeGesundheitsbefragung2002: Die Indices. Neuchaˆtel: Bundesamtfu¨rStatistik, Sektion Gesundheit.
- Swiss Federal Statistical Office (2004) Medienmitteilung:Einkommens- und Verbrauchererhebung 2002. Neuchaˆtel:Bundesamtfu¨rStatistik.
- Swiss Society of Obstetrics and Gynecology (2004) GuidelinezumVorgehenbeisuspektem und positivemzytologischemAbstrich der Cervix uteri. U¨ berarbeiteteFassung,Version 4. Schweizerische A ¨ rztezeitung 85:2305–21.
- Tammemagi CM (2007) Racial/ethnic disparities in breastand gynecologic cancer treatment and outcomes. CurrentOpinion in Obstetrics and Gynecology 19:31–6.
- Taylor RJ, Mamoon HA, Morrell SL et al (2001) Cervicalscreening in migrants to Australia. Australian and New Zealand Journal of Public Health 25:55–61.
- Taylor RJ, Morrell SL, Mamoon HA et al (2003) Cervical cancer screening in a Vietnamese nominal cohort. Ethnicity and Health 8:251–61.
- Van Ballegooijen M, Van Den Akker-van Marle E, Patnick J et al (2000) Overview of important cervical cancer screening process values in European Union (EU) countries, and tentative predictions of the corresponding effectiveness and cost-effectiveness. European Journal of Cancer 36:2177–88.
- Vellozzi CJ, RomansMand Rothenberg RB (1996) Delivering breast and cervical cancer screening services to underserved women: Part II. Implications for policy. Women’s Health Issues 6:211–20.
- Vissandje´e B and Dupe´re´ S (2002) Comportementspre´ventifs pour de´pister le cancer du sein et du col de l’ute´rus. In: Sante´ et Bien-Etre, Immigrants Re´cents au Que´bec: une adaptation re´ciproque? Que´bec: Institution de la Statistique du Que´bec.
- Vitorino AV (2009) Migrations: opportunity or threat? Housing and health in the integration of immigrants. Lisbon: Principia.
- Vranjes N, Bisig B and Gutzwiller F (1996) Gesundheit der Ausla¨nder in der Schweiz. Bern: Bundesamtfu¨r Gesundheit.
- Wanner P, Bouchardy C and Raymond L (1998) Comportement des e´trangersen Suisse enmatie`red’alimentation, de consommationd’alcoolet de tabac et de pre´vention. De´mos 2:3–20.
- Wanner P, Raymond L and Bouchardy C (2001) Taux de participation au de´pistage du cancer du col ute´rind’apreˆsl’Enqueˆte Suisse de Sante´ conduiteen 1997. Bulletin Suisse de Cancer 2:86–9.
- Wiking E, Johansson SE and Sundquist J (2004) Ethnicity, acculturation, and self-reported health. A populationbased study among immigrants from Poland, Turkey, and Iran in Sweden. Journal of Epidemiology and Community Health 58:574–82.
- Wolff H, Stalder H, Epiney M et al (2005) Health care and illegality: a survey of undocumented pregnant immigrants in Geneva. Social Science and Medicine 60:2149– 54.
- World Health Organization (1998) HEALTH21: an introduction to the health for all policy framework for the WHO European Region. Copenhagen: World Health Organization Regional Office for Europe.
- World Health Organization (2004) Strategies to Improve and Strengthen Cancer Control Programmes in Europe. Report of a WHO Consultation. Geneva: World Health Organization.
- Zemp E (2000) Gesundheit der Frauen. In: Gesundheit und Gesundheitsverhalten in der Schweiz 1997. Neuchaˆtel: Swiss Federal Statistical Office.