Keywords
Maternal health; Indigenous population; Delivery of healthcare; Culturally competent care; Healthcare disparities
Abbreviations
CPS: Child Protective Services; GDM: Gestational Diabetes Mellitus; HCPs: Healthcare providers; NU: Nunavut; NT: Northwest Territories
Introduction
Maternal health is defined by the World Health Organization as being comprised of “women’s health during pregnancy, childbirth and the postpartum period”[1]. Complications in pregnancy and childbirth, such as hemorrhage, infections, high blood pressure, ectopic pregnancy, preterm birth, unsafe abortion and obstructed labor, are recognized as threats to maternal health[1] while factors such as access to family planning services, counseling, and appropriate antenatal, obstetric, and postpartum care are identified as being positive contributing factors to maternal health2. Maternal mortality rates are used as a proxy measure to indicate access to and the quality of maternal care[2]. With a maternal mortality rate of 7.8 per 100,000 live births between 2008 and 2010, it is evident that many Canadians can easily access maternal health services of exceptional quality[3]. There are, however, notable differences between Indigenous and non-Indigenous Canadians for many indicators of maternal health; Indigenous women in Canada have a two times higher risk of maternal mortality in comparison to the general Canadian population[4-6].
Indigenous women also experience higher rates of adverse outcomes including stillbirth and perinatal death, and, in some cases, low-birth-weight infants, prematurity and infant death[4-6]. While Inuit women of childbearing age experience higher rates of low-birth-weight babies, First Nations and Métis women experience elevated incidences of both low- and high-birthweight babies compared to the general Canadian population; these can have adverse implications for the babies’ health[4-9]. Nunavut (NU), the Northwest Territories (NT) and Yukon are located in northern Canada and have the highest percentage of the population identifying as Indigenous compared to other Canadian provinces and territories[10]. In Canada, the greatest proportion of women who received inadequate prenatal care, deÃÆÃâÃâïÃÆââ¬Å¡ÃâìÃÆââ¬Å¡ÃâÃÂned as having four or fewer visits during pregnancy, was in NU (7.7%)[11]. In 2006-2007, NT had the greatest proportion of women not receiving prenatal care (27%) and NU had the greatest proportion of late prenatal care (after the first trimester) (17.3%)[12]. In 2011, NU had Canada’s highest infant mortality rate, more than 3 times the next highest rate[13]. NT had the third highest infant mortality rate in 2011 and had the first, second and third highest rates for three of the five years between 2007 and 201113. In 2004, NU reported the highest teenage pregnancy rate in the country where 24% of live births were to mothers under the age of 19 years, compared to the national average of 5%[14]; teenage pregnancy is associated with low birth weight and prematurity among new-borns[15]. In 2004, the preterm births rate in NU was 12% compared with 8% in other regions in Canada[16]. Moreover, the rate of neonatal hospital readmission was higher in NU than in Canada (5.5% vs. 3.5%). In addition, Indigenous women in some regions experience elevated rates of human immunodeficiency virus[17], cervicovaginal infections such as human papillomavirus[18,19] and the presence of bacterial vaginosis and organisms such as Chlamydia trachomatis, group B Streptococcus, Mycoplasma hominis or Ureaplasma urealyticum during gestation[20].
Various historical events associated with colonial policies have impacted Indigenous Canadians negatively, including the destruction of lands which are vital to Indigenous ways of life, forced placement and separation from families through residential schooling, marginalization of languages and spiritual beliefs, assaults on dignity and autonomy through the introduction of assimilation policies, and multiple forms of racial discrimination[21]. Many Indigenous people who experienced colonialism have suffered from trauma[22] and the resulting effects of the trauma, such as mental illness, anxiety, depression, suicide, violence, low self-esteem, anger, feelings of hopelessness, challenges in recognizing and expressing emotions and sexual, alcohol and drug-related vulnerabilities[23-27]. For decades, these residual effects of trauma have been sustained as a form of trans-generational trauma[28] and have served as key contributors to many of the inequities in health and well-being among indigenous peoples around the globe[23-25]. Historically, Indigenous women and particularly older women, exerted significant influence in communities and played crucial roles in advising younger community members and relaying important cultural and spiritual teachings; with colonialism their roles diminished and a more patriarchal society emerged[29]. These shifts significantly altered Indigenous women’s identities and responsibilities[30]. The newly formed patriarchal society not only decreased feminine power, agency and autonomy, it may have exposed women to increased levels of violence and sexism[31]. These events have had consequences not only for women’s health, but also for the families and communities[30].
Some previous studies have identified factors which may potentially exacerbate adverse maternal and infant health outcomes among Canadian Indigenous populations[32]. These factors include socio-cultural and socio-economic status, which may affect diet and lifestyle[32-42], accessibility to healthcare services[43-46], incidence of gestational infections and illnesses[47,48], prevalence of smoking and alcohol consumption during pregnancy[49-51], as well as presence of hazardous environmental contaminants[52-56], which all directly and indirectly impact the health and wellness of Indigenous Canadian women. However, there is a knowledge gap that precludes a comprehensive understanding of maternal health among indigenous women in Canada. Prior to the development and implementation of health promotion policies and actions that address maternal health disparities, an in-depth understanding of the perspectives of Indigenous Canadian women regarding maternal health is essential. In this article, we included all of the published literature that examined experiences and perspectives of Indigenous Canadian women during pregnancy, childbirth, and the postpartum period towards maternal health. This review highlighted some of the main contributors to maternal health disparities from Indigenous Canadian women’s perspectives and documented the knowledge gaps and maternal health areas requiring further examination. This information can be used to inform future policies and intervention programs which influence maternal healthcare services and reduce the financial and emotional costs associated with complications during pregnancy and adverse maternal health outcomes.
Methods
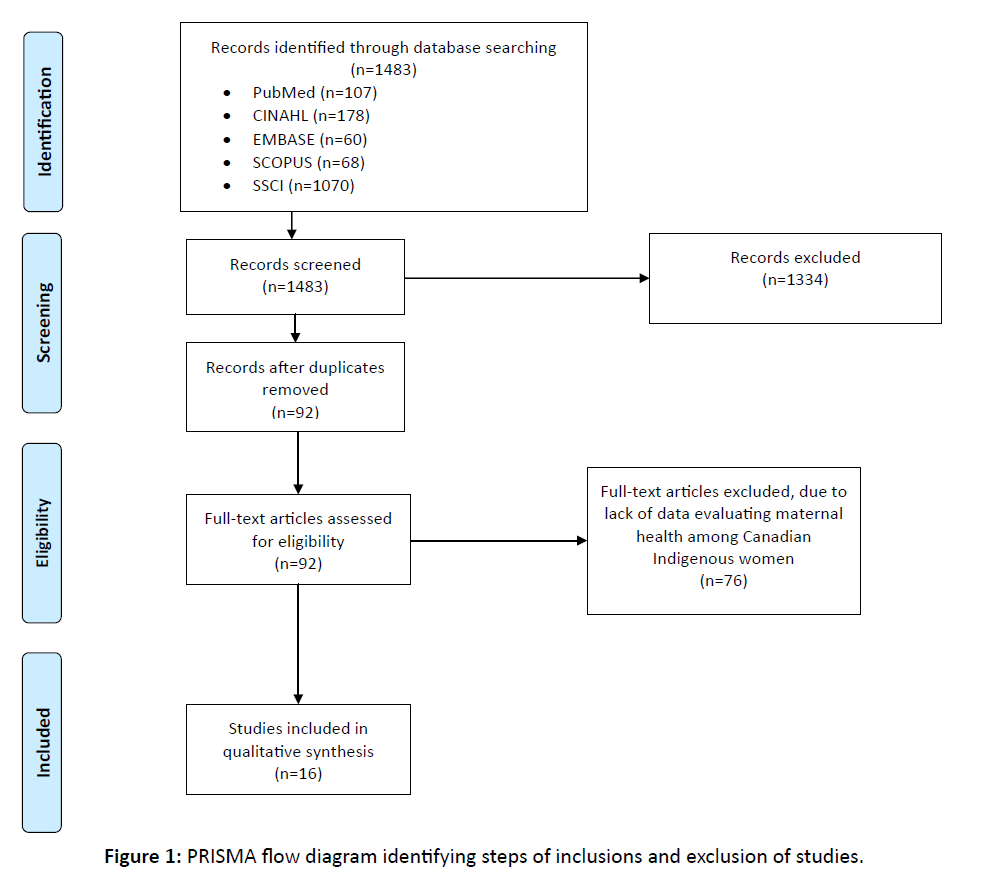
The systematic review followed the protocol, Preferred Reporting Items for Systematic Reviews and Meta-Analysis. It systematically searched English full articles published between January 1990 and March 2015 in main electronic databases (i.e., PubMed, CINAHL, EMBASE, SCOPUS and SSCI) for topics related to maternal health of Indigenous Canadian women. Subject descriptors were the following MeSH terms/or text word(s): “maternal,” “health/healthcare” and “Canada” as well as “Indigenous” or “Aboriginal.” Additional studies were identified by searching the reference lists of identified articles. Two reviewers (FK, KJY) screened the titles and abstracts of all identified sources to remove duplicates and irrelevant records and evaluated the full-text of selected sources. The quality appraisal criteria for observation and/or intervention studies including clear presentation of research goal, participants, methods and results were used to ensure reviewers’ reliability. Lastly, information including the first author’s name, published year, population group, participants, outcomes, and results was extracted from the selected sources.
Results
The literature search identified 1483 potentially relevant publications from the scientific databases (PubMed n=107, CINAHL n=178, EMBASE n=60, SCOPUS n=68 and SSCI n=1070) (Figure 1). The title and abstracts were reviewed, and a total of 149 records were selected. Duplicates (n=57) were removed and a total of 92 articles retrieved for further review, of which 16 studies presented data that evaluated maternal health among Canadian Indigenous women: one article on perceptions, assumptions and recommendations for maternal healthcare57;seven articles on experiences of birthing and maternal healthcare[57-63]; and eight articles that presented data relevant to both categories[64-68] (Table 1). These articles were further classified by the primary area of research described in the study: eight articles on maternal healthcare and/or medical evacuation65-[68]; three articles on the impact of policies on maternal health[59-63]; three articles on gestational diabetes mellitus (GDM)[61,62]; and two articles on maternal weight changes and/or breastfeeding[66-68]. The included studies described 1043 participants, of which 918 were identified as being Indigenous peoples or from an Indigenous community. The remaining 125 participants were either non-Indigenous or their identity was not provided. The specific Indigenous identities mentioned were Inuit, Métis, Salteaux, Haida, Nuxalk, Cree, Ojibway and KwakwaÃÆÃâÃâ¦Ã¢â¬â¢ÃÆââ¬Å¡ÃâñkaÃÆÃâÃâ¦Ã¢â¬â¢ÃÆââ¬Å¡Ãâñ'wakw. Participants were included as mothers or pregnant women (n=814), healthcare providers (HCPs) or workers in a health-related field (n=132) and fathers, Elders or other community members (n=97).
Maternal healthcare and/or medical evacuation
Medical evacuation was described in five studies[65-69]. Medical evacuation was often due to the limited maternity care options available in remote communities. Pregnant and postpartum women who left their communities to give birth experienced emotional, physical and financial stress, and women did not feel in control of their birthing experiences[65-69]. Mothers felt disconnected and isolated from their family, community, and culture; they were required to give birth in an unfamiliar environment without the support of their families and often expressed concern about children left at home[65-69]. Some medical costs of birthing outside the community are covered by the government or band councils, but additional financial burdens included the cost of childcare, loss of income if their partner had to miss work to take care of children, and the cost of travelling for their partner to be present at the birth[65-69]. For some women, the increased financial burden made it difficult to afford appropriate food and affected prenatal nutrition[ 65-69]. The combination of stressors was perceived to be a factor in experiences of depression[65-69].
Figure 1: PRISMA flow diagram identifying steps of inclusions and exclusion of studies.
| Study Design |
Findings |
|
| Location |
Participants |
Perceptions, assumptions and recommendations about maternal health |
Experiences of birthing and maternal healthcare |
| Maternal healthcare/Medical evacuation |
| Inuit community in Canadian Arctic |
Mothers (n=20)
Fathers (n=3)
Community members (n=5) |
|
-Women experienced emotional, physical and economic stressors due to traveling away from their community to give birth.
-Women were given little choice or support for the place of birth and method of delivery.
-The community birthing center provided psychosocial benefits including reduction in family disruption, greater parent satisfaction, and greater father involvement with the baby. |
| British Columbia |
Key informantsA:•Indigenous people
(n=44)
•Non-Indigenous
(n=29)
|
-Pregnancy was perceived as an important opportunity for an individual to make life changes. Participants indicated that pregnancy was often a time when prospective parents examined their own past, and considered healthier choices to provide a better future for their children. |
-Participants reported safety and responsiveness as important aspects of healthcare during pregnancy and parenting. Safety included healthcare environments that were non-judgemental, supportive and allowed healthcare providers and patients to build relationships. Responsive care was holistic, client-directed and integrated a patient’s experiences and cultural knowledge. |
| Bella Bella/Waglisla, British Columbia |
First Nations women (n=67) |
-From the perspective of losing local services, participants expressed the importance of a local birth in reinforcing the attributes that contributed to their identities including the importance of community and kinship ties, and the strength of ties to their traditional territory. |
-Positive aspects of maternal care in the community involved trusting relationships with local healthcare providers.
-Loss of antenatal services in a community was followed by a decrease in prenatal and postpartum care services |
| Herk KA, Smith D, Andrew C (2010) |
A Canadian City |
Healthcare providers and Indigenous family members:•First Nations
(n=9)
•Inuit (n=4)
•Non- Indigenous (n=8)
|
-Healthcare service providers’ perception of Indigenous women as mothers influenced the women’s experience of accessing care. |
-Negative experiences during pregnancy were related to racism, lack of local healthcare availability and economic issues.
- Indigenous healthcare issues must be examined with understanding of historical context. |
| O’Driscoll T, Kelly L, Payne L, et al. (2011) |
Sioux Lookout, Ontario |
First Nations women (n=13) |
-Participants were receptive to suggestion of a culturally appropriate doula program and in-hospital visits by First Nations Elders.
-Participants were less interested in tele-visitation with families in their communities. |
-Women who travelled to access intrapartum maternity care experienced loneliness and missed their families.
-Positive experiences at the hospital were due to feeling of safety
-Most participants received prenatal information from family members instead of from healthcare providers
-The study’s systematic review found mostly negative experiences for women who travelled to access intrapartum maternity care |
| Brown H, Varcoe C, Calam B (2011) |
Remote, coastal British Columbia communities |
Mothers (n=102)
Fathers (n=3)
Youth (n=5)
Elders (n=11)
Healthcare Providers (n=4) |
-Community histories, resources and women’s feeling of choice, power and control resulted in expectations of the birthing experience. |
-Pregnancy and birthing experiences were impacted by: limited economic resources; loss of traditional knowledge; need to travel for maternity care; and culturally sensitive maternity care.
-The participants’ experiences in each community were shaped by: distinct histories, traditions, economics, politics and geography; the impacts of colonization and medical paternalism; and the struggle for control of women’s bodies during birth. |
| Varcoe C, Brown H, Calam B, et al. (2013) |
Remote, coastal British Columbia communities |
Mothers (n=108)
Fathers (n=3)
Youth (n=5)
Elder (n=11)
Healthcare providers/leaders (n=9) |
|
-Most participants described distressing experiences during pregnancy and birthing as they grappled with diminishing local maternity care choices, racism and challenging economic circumstances.
-Positive experiences with healthcare providers were due to respect, understanding of cultural context and connection with communities
-Rural Indigenous women’s pregnancy and birthing experiences were impacted by the intersections among rural circumstances, the effects of historical and ongoing colonization, and concurrent efforts toward self-determination and more vibrant cultures and communities. |
| Lallo SD (2014) |
Wetaskiwin, Alberta |
Pregnant Indigenous women (n=281) |
|
-Provision of culturally safe care by a multidisciplinary team and removal of transportation barriers resulted in increased participation in the prenatal care program
-Participants felt that care delivery was more efficient and supportive of their needs than mainstream healthcare |
| Gestational Diabetes Mellitus |
| Neufeld HT, Marchessault G (2004) |
Manitoba |
Indigenous mothers
(n=14)
Indigenous grandmothers (n=14) |
-Participants expected that diet and activity patterns were linked to GDMB.
- Participants linked sugar and processed foods with diabetes.
-Grandmothers tended to discuss decreasing activity patterns and increasing maternal size
-Mothers tended to discuss the role of stress in GDM
-Participants recommended increased consumption of wild meat and fresh foods as GDM prevention measures. |
|
| Neufeld HT (2011) |
Winnipeg, Manitoba |
Indigenous women with GDM experience (n=29) |
|
-Participants experienced fear, anxiety, frustration and negative relationships with food in association with GDM diagnosis.
-Participants felt socially isolated, had poor self-images, and had feelings of failure resulting from ineffective GDM management practices.
-Complex factors influenced women’s perceptions and reported behaviours, suggesting that the experience of living with GDM can be overwhelming. |
| Neufeld HT (2014) |
Winnipeg, Manitoba |
Maternal care providers/ community members (n=25)
First Nations/Métis women with GDM experience (n=29) |
|
-Pregnant women’s access and quality of prenatal care and diabetes education was limited by assumptions of blame regarding GDM diagnosis, and the burden of responsibility in dealing with GDM.
-Participants discussed the importance of establishing trust between patients and caregivers to improve communication and support for GDM clients
-Health professionals who attempted to use their position of power to leverage compliance caused distress and confusion for patients. |
| Maternal weight changes/Breastfeeding |
| Vallianatos H, Brennand EA, Raine K et al.(2006) |
James Bay, Quebec |
First Nations mothers (n=30) |
-Participants perceived that excessive weight gain during pregnancy could lead to negative health consequences.
-66% of participants stated that weight gain during pregnancy was normal. 30% of participants thought they gained too much weight. The health of the baby affected whether weight gain was seen as good or bad.
-Participants believed that weight gain during breastfeeding resulted in more milk production. Quantity and quality of mothers food intake was expected to affect the milk supply and health of the baby.
-Participants considered a healthy lifestyle to include physical activity, eating traditional foods and following the Canada Food Guide. |
-Participants had difficulty losing weight gained during pregnancy due to individual constraints, cultural beliefs, and community constraints.
-Individual constraints included: lacking energy or time for healthy behaviors; social isolation; lack of knowledge about achieving a healthy lifestyle; and difficulty breaking established habits.
-Cultural beliefs inhibited postpartum weight loss due to beliefs that breastfeeding women should eat frequently to aid milk production.
-Community constraints included a lack of available services for new mothers such as child care or exercise facilities, in addition to financial or transportation barriers that prevented access of existing services. |
| Eni R, Philips-Beck W, Mehta P (2014) |
British Columbia, Manitoba, and Ontario |
First Nations mothers (n=65) |
-Participants discussed social factors including: perceptions of self; breastfeeding environments; and intimacy, including the contribution of fathers. |
-Environments can support or discourage breastfeeding
-Breastfeeding and bed-sharing were linked
-Obstacles to breastfeeding included: a history of residential school attendance, physical and psychological trauma, evacuations for childbirth, and teen pregnancy.
-Fathers played a pivotal role in a woman’s decision to breastfeed |
| Impact of policies on maternal healthcare |
| Borland T, Babayan A, Irfan S, Schwartz R (2013) |
Ontario |
Key informantsC (n=31)
Pregnant or postpartum, current or former smokers:•Indigenous peoples (n=11)
•Non- Indigenous (n=18)
|
-Participants recommended: a comprehensive cessation strategy to facilitate coordination; furthering tobacco control policies; and targeting the social determinants of health through poverty reduction, housing and education support.
-Key informants discussed the need for capacity building within tobacco control services and within reproductive, child and maternal health services.
-Participants recommended: providing incentives, transportation, childcare and meals/snacks; adopting woman-centred, harm-reduction and stigma reduction approaches; and promoting programs through a variety of local venues to address engagement and accessibility issues. |
-Key barriers to smoking cessation included: the absence of a provincial cessation strategy and funding; the absence of resources tailored to Indigenous women and adolescents; geographical challenges; capacity issues; and engagement issues. |
| Tait CL (2013) |
Saskatoon, Saskatchewan |
First Nations woman (n=1) |
|
-Lack of family support, disconnected government services and shot term addiction treatment programs with limited aftercare had negative impacts on the participant’s experiences of pregnancy, birth and parenting.
-The participant’s life experiences were shaped by a history of residential schooling, negative interactions with Child and Family Services, domestic violence, addiction and poverty. |
| Denison J, Varcoe C, Browne AJ (2014) |
Two urban Indigenous health centers in Canada |
Indigenous women and healthcare providers:•First Nations (n=14)
•Métis (n=1)
•Non-Indigenous (n=9)
|
|
- Indigenous women whose children are involved with the child protection system experience complex socio-political and economic challenges, which intersect with the threat of child apprehension.
-The threat of child apprehension did not impact women’s decisions to seek healthcare services for their children.
-Experiences of racism, prejudice and discrimination in mainstream healthcare agencies and the fear of child apprehension deterred women from seeking healthcare for themselves. |
AWorkers in maternal and child health fields, community members, service providers, and leaders from one urban and one rural Indigenous healthcare delivery organization
BGestational Diabetes Mellitus
CIndividuals with expertise in smoking cessation support for pregnant or postpartum women at local/provincial levels and/or insight into the needs of this population
Table 1:General characteristics of the studies included in perceptions, assumptions and recommendations about maternal health and experiences of birthing and maternal healthcare among Indigenous women of childbearing age in Canada.
“There is a breakdown in the traditional family structure, as the mom is away from her community and family while she is giving birth. The family is excluded from the joy of being at the birth- this is important to our community, to our families” [65-69].
“I went through the depression really bad, because I had to be in Vancouver so long by myself. I didn’t know anyone”[46].
A benefit of medical evacuation was the feeling of safety at a hospital69. However, local community births, in comparison to medical evacuations, were68 associated with more positive experiences[65-69]. A community birthing centre was found to provide greater parent satisfaction, greater father involvement with the baby, and a reduction in family disruption compared to medical evacuation[65-69]. Local births were important to Indigenous identity and community and helped to reinforce ties to community and traditional territories territories[65-69]. Local births provided opportunities for celebration and were important to provide balance to the observations of death in a community[70].
“…everyone is so happy to go and give to the baby…even if you are not closely related…because it is another member of the Haida Nation, and it just makes the community bigger and richer. In the long run it will make it stronger”[46].
“All we see is death...We are in a small community and it’s constantly death, death, death, death. When you don’t have birth here and they’re born outside, you know, it’s different. There has to be a balance. There’s end of life and beginning of life”[70].
Maternal healthcare within the community provided pregnant women the ability to build relationships with local HCPs [70]. Women preferred to have HCPs that they were familiar with during their birthing experiences46. Women were confident in the skills of their local HCPs and felt more comfortable around them46. Inability to develop relationships with HCPs, whether due to medical evacuation or because remote communities have difficulty retaining staff, introduced stress to the maternal healthcare experience[65-69].
“I’m sure I wouldn’t have been as scared if I’d had my own doctor around”[46].
Three studies[60,67,69] examined the introduction of culturally safe care—that is, an approach to maternal healthcare, focusing on being “relevant for and responsive to women’s and families’ needs, strengths, and desire for control and choice in the birthing experience”[65-69] pointed out that culturally “appropriate” or “competent” practice[60], “which focuses on the skills, knowledge and attitude of practitioners,”[46,65,60 ]“while necessary, is not sufficient”. For example, the Aboriginal Prenatal Wellness Program in Alberta was developed to serve Indigenous women who were not accessing prenatal care services[60]. This program offered culturally safe care and catered to patients by training staff to understand traditional practices, cultural history, and health disparities of indigenous peoples. After initiating the program, the percentage of women delivering in the hospital who had limited or no prenatal care decreased from 19.5% in 2002 to 13.5% in 2006[60]. Participants of the program indicated that the care they received was more efficient and supportive than mainstream healthcare[60]. A community based study of two Indigenous healthcare delivery organizations in British Columbia identified examples of culturally safe and responsive care[67] HCPs at these organisations made an effort to embrace local cultural values and make the patients feel safe in order to empower them to improve their health. Sioux Lookout Meno Ya Win Health Centre also provided culturally safe care[69]. Patients were in favour of having First Nations doulas and visits from First Nations Elders, but reported that they received most of their prenatal knowledge from their family instead of from HCPs[69]
“We’re trying to work with women to invite them to explore some of the traditional practices, like before they give birth, and try to incorporate it into a birth plan. And even through the pregnancy, to try to use some of those belief systems and have that guidance instead of white society telling you what you should and shouldn’t do”[67].
“I just feel more secure…I feel safe”, patient at the Sioux Lookout Meno Ya Win Health Centre69.
Impact of policies on maternal healthcare
Three studies investigated the impact that government policies have on the provision of services and programs in areas that affect maternal health[65-69]. One study examined barriers to smoking cessation among pregnant and postpartum women, one study interviewed HCPs and women being investigated by Child Protective Services (CPS), and one study explored the life history of an Indigenous woman who experienced the interference of multiple government policies into her life[65-69].
Inconsistent and non-comprehensive policies were found to impede maternal health and healthcare access. Pregnant and postpartum women who were current or former smokers had received inconsistent information; they were unsure whether smoking cessation during pregnancy was safe or stressful to the fetus and whether pregnant women were eligible for nicotine replacement therapy64. HCPs and women being investigated by CPS reported inconsistent policies and limited supportive services available to assist a mother in retaining custody of her child; several women had their children apprehended by CPS despite completing parenting programmes at the request of CPS[59,65]. The case study individual participated in an addiction treatment program during her first pregnancy[63], but this program was short-term and was unnsuccesful at connecting the participant with further resources to manage her addiction.
“…there’s no consistency in what [Child Protective Services] does, like from worker to worker”[59,62].
“I think it is very limited…sort of a patchwork of strategies that are loosely weaved together.” Key informant discussing the uncoordinated nature of smoking cessation resource[64].
These studies provided evidence that to address a health issue, policies need to consider the wider context in which the health issue exists. The current or former smokers identified other challenges in their lives such as substance abuse, unstable domestic situations, low socio-economic status, and attending pre/postnatal appointments that compromised their ability to attend smoking cessation programs[64]. A successful smoking intervention considered the potential socio-economic barriers of their participants and provided free transportation to the smoking cessation program and rewarding participants with a weekly grocery store gift card.
“…this is making me feel even better because after this I don’t need a cigarette. I can go to the grocery store and get healthy food ...”[64].
The case study demonstrated how the co-occurrence of poverty, mental illness, addiction, and unstable domestic situations made it challenging for a First Nations woman to access healthcare and maintain custody of her children[63]. Loss of custody can be harmful to a parent’s wellbeing, due to both the emotional loss of a child and the potential reduction in social welfare benefits63. Without proper counselling or support, parents who previously had addiction issues may turn to substance abuse as a coping mechanism[63]. Many women who were being investigated by CPS had themselves been apprehended by CPS as children[59-63]. These women may have had unstable childhoods, insufficient family support, and an absence of positive parenting models, but few received parenting support from CPS to asssist them with raising their children[59-63].
Gestational diabetes mellitus
Neufeld et al conducted three studies on Indigenous women and GDM (2004; 2011; 2014). One study explored beliefs about GDM causation and prevention; the other two studies explored the experiences of pregnant women with GDM and the experiences of HCPs. Some women believed that diabetes could be prevented by eating healthy foods, while others believed that if family members were diagnosed with diabetes then it would be unavoidable[57] . The distinction between inevitability or preventability was discussed by HCPs and GDM-diagnosed women in Manitoba[62]. The patients felt that HCPs blamed them for having GDM[62]. The importance of building trusting and supportive patient-provider relationships was mentioned by both HCPs and patients62. Relationships in which the provider had power over the patient made patients feel uncomfortable and afraid to ask questions for clarification[62]. Inconsistency in health advice and the inability to consistently be attended to by the same HCP was frustrating for participants[62]; some women preferred to listen to family members or their instincts instead of their HCPs[61].
“I don’t know what to think but I think that it’s because there’s so many different doctors seeing me, they all tell me something totally different”[63].
Participants were confused by GDM management advice when vegetables and fruits would make their blood sugar rise faster than chocolate bars or fries61. Women received contradictory and confusing information about GDM management, found it challenging to control their blood sugar levels and felt powerless[61,63]. Pregnant women were afraid of harming their fetuses due to their diet[61-63].
“…tomatoes and apples and whatever aren’t good for you, they’re high in sugar” [61].
“I’d eat, like, an apple, and my sugar would go up and up. Well why can’t I eat an apple?”[61]
“That stressed me out! In those 2 weeks I watched what I ate. Sometimes I didn’t eat at all. I would live on water.” The participant’s physician had told her that her baby would be stillborn if she did not control her blood glucose[61].
Maternal weight changes and/or breastfeeding
Two studies interviewed First Nations mothers about breast feeding experiences and beliefs[59-65]. Eni et al. reported factors that encouraged or deterred breastfeeding[59-65]. Vallianatos et al. reported barriers to achieving a healthy weight during breastfeeding68. Both studies revealed how personal and community factors impacted health behaviours. Participants in both studies reported a personal deficiency of time or energy to devote to healthy behaviours due to responsibilities of caretaking, household chores, or employment[59-65].
“It’s not like everything else around you stops and you can just breastfeed. It’s dealing with everything at the same time.”
Communities influenced health behaviours. Women who wanted to lose weight postpartum found that the community had limited affordable and accessible services to assist with nutrition and exercise. Breastfeeding-supportive communities increased the likelihood of breastfeeding by providing support services in the form of lactation experts, access to peer support, and home visits[66]. Social influence impacted whether women felt comfortable breastfeeding; women were more likely to breastfeed if breastfeeding was accepted and seen as normal behaviour among their friends, families and communities[66-69].
“The friends and the people that I was around they didn’t think it was right [to breastfeed]”[66-69]. “Well these (breasts) were not toys when I was growing up. These were for food” [66-69].
Discussion
Indigenous women face a unique set of challenges in accessing maternal health services. Small, rural and remote communities often provide limited healthcare especially for complex pregnancies[43,44]. Some pregnant women have to leave the communities and travel great distances to have their maternal health needs addressed and to deliver their babies [43,44]. This process causes a significant disruption in family life, separating women from their families and communities, and can lead to significant physical, emotional, and financial stresses[43,44]. In addition, the mother’s health needs are often further complicated by determinants of health, such as poverty, inadequate housing, compromised nutrition owing to a limited access to affordable and nutritious foods, language barriers, and cultural differences[32-42].
This review explored maternal health experiences and perspectives from the viewpoint of Indigenous women of childbearing age in Canada. These experiences and perspectives suggested that the main factors that impacted Indigenous women’s maternal health were limited local healthcare resources, healthcare services that did not consider co-existing socio-economic and lifestyle barriers to healt and the impact of colonization on the relationship between HCPs and Indigenous women.
Regardless of the location of care, relationships with HCPs were important for influencing maternal healthcare experiences. Maternal healthcare experiences were shaped by complex interactions between cultural traditions, geography and the impact of colonization in a community[59-65]. These forces affected the women’s expectations of their birthing experience and HCP’s perception of Indigenous women as mothers[59-65]. Culturally safe care programs were viewed as potential methods for improving the maternal healthcare experience of Indigenous women[69]. Positive experiences involved patient-provider interactions that were based on respect; free of judgment; holistic; and demonstrative of an understanding of the cultural context[67-71]. Negative experiences involved women experiencing racism, cultural insensitivity, and limited control over their care[72-74]. A study examining the attitude of family medicine residents towards providing healthcare to Indigenous peoples revealed that the majority were not educated on Canadian Indigenous history and, although willing, felt unprepared to work in Indigenous contexts[75]. Providing HCPs with education, which focuses on cultural responsiveness and HCPs’ critical selfreflection, could assist in building supportive and empowering relationships with patients.
This educational approach could also assist HCPs in understanding how culture influences health behaviours. Among a Cree community, breastfeeding women were encouraged to eat frequently which made it challenging to lose the weight gained during pregnancy[68]. This was due to a tradition based on previous generations who had a physically active lifestyle and a traditional diet; breastfeeding women had to eat frequently to prevent excessive weight loss that could decrease milk production68. The generation involved in the study had a more sedentary lifestyle and higher-calorie foods but cultural traditions continued to encourage them to eat68. A separate study found that a loss of cultural tradition resulted in fewer women breastfeeding their infants[66-69]. In addition to understanding cultural influences on health behaviours, it is necessary for HCPs to understand how Canadian government policies and actions have affected generations of Indigenous people’s health. Colonization, residential schools, the ‘60s Scoop’ and other initiatives have resulted in experiences of trauma and culture loss and contributed to high rates of low socio-economic status for many Indigenous peoples; these experiences impact maternal health and healthcare access [21-23,41]. A futher result of colonization was the forced acceptance of European medical practices and the interuption of traditional birthing methods[65-68]. When resources and trained staff became scarce, the availability of European medical services declined without allowing the reintroduction of traditional birthing methods, requiring pregnant women to leave their communities to give birth. A 2013 guideline provided 24 recommendations to facilitate the provision of culturally safe care, and advocated for the return of local births to remote and rural communities[69].
Culturally safe care to improve the healthcare experience of Indigenous peoples has been recommended and attempted in multiple countries, including Canada, Guatemala, Australia, Mexico, and the United States of America[70,71,76-85]. Some of these initiatives have resulted in reports of positive patient experiences, but futher areas of improvement have been identified to increase respect of Indigenous peoples and recognition of traditional knowledge[86-89]. Midwifery services and midwifery education programs are deemed culturally safe maternal healthcare options for remote communities[85]. Midwifery programs have provided maternal healthcare for indigenous populations in other countries, such as Australia, where an Indigenous midwifery program was associated with lower proportions of preterm babies, lower birthweight babies and a lower Caesarean section delivery rate than the regional average[89].
Unsuccessful implementations of culturally appropriate interventions in Guatemala[83-85] and Mexico highlight another important topic: community control. Interventions in Guatemala[83-85] attempted to integrate local Indigenous practices with biomedical care practices but did not sufficiently involve Indigenous community members in the design or implementation stages, which led to a birthing centre that was unused for three months and services that excluded Mayan midwives[83,90,91] and the United States of America[81,91] provide examples of successful culturally safe maternal healthcare programs that have been community controlled. These programs empowered participants, built trusting patient-provider relationships, improved preconception health knowledge and improved the health outcomes of mothers and babies[83,90,91]. To increase the likelihood of success, culturally safe programs should be developed with the input and participation of the target Indigenous community[83,90,91]. The existence of health inequities between Indigenous and non-Indigenous women in urban areas reinforces the need to address structural barriers to health. Several studies on birth outcomes have found that differences between Indigenous and non-Indigenous women were not statistically significant after adjusting for other socio-economic and demographic risk factors[91,92]. Provision of ample maternal healthcare services may not sufficiently improve maternal health without providing interventions into the socio-economic circumstances that unequally affect Indigenous peoples[93]. Inuit-inhabited areas have higher rates of pre-term birth, which is known to be associated with “low socio-economic status, high rates of cigarette smoking, psychological stress and poor nutrition”[94]. A Maternity Experiences survey conducted by the Public Health Agency of Canada found that women from NU reported having less information on pregnancy-related topics, but reported more smoking, more abuse, and more symptoms suggesting postpartum depression than other Canadian women[17]. Between 60% and 85% of pregnant women in NU reported smoking during pregnancy, five times the Canadian average[17,95]. Cigarette smoking is the single most important modiÃÆÃâÃâïÃÆââ¬Å¡ÃâìÃÆââ¬Å¡ÃâÃÂable cause of adverse pregnancy outcomes affecting infant mortality and morbidity[96]. Further, 26.2% of Inuit women in the Baffin region of NU consumed alcohol, illicit drugs, or both during pregnancy[97]. Studies on Indigenous peoples in Mexico[93] and Australia98 have recommended that policy interventions be applied to address historical, cultural, and socio-demographic barriers to healthcare access.
This review supports the need for initiatives and consistent policies that provide culturally responsive training to HCPs to enable them to support and empower patients, facilitate local births in remote communities, and account for the socioeconomic and socio-cultural factors that impact maternal health. This review advocates for the provision of patient-centered maternity healthcare services within Indigenous communities.
“Aboriginal women in remote and rural communities should not have to choose between their culture and their safety”[99].
The limitation to this review is the limited availability of peer-reviewed data regarding Indigenous maternal health in Canada; however, this review provides some insights for moving towards culturally safe and responsive maternal healthcare services for Canadian Indigenous women. It is critical to reinforce respectful relationships between HCPs and Indigenous women in order to restore women’s sense of power and control over their own health. This can be done by educating HCPs to understand Indigenous history and by valuing Indigenous maternal traditions and prenatal knowledge[60-69]. The integration of Indigenous birthing practices can promote Indigenous mothers self-determination, leadership, choice, and control[65-68].
“Attention is too often focused on marginalised populations and how to help them get the care they deserve, without realizing that this will not be possible without health care providers... being attentive to what it is about us that make it difficult for people to feel safe to access care”[67].
Furthermore, it is crucial to acknowledge the importance of valuing Indigenous land and sense of place100 emphasizes the importance of community and place in Indigenous identities, as opposed to the importance of independence in Euro-Canadian identities. Acknowledging the value of the location of a community is necessary in considering allocation of maternal healthcare resources, and allowances must be made to enable women to receive maternal healthcare in their communities whenever possible[73]. Finally, policies and interventions that affect maternal healthcare require collaboration with local Indigenous communities. Maternal healthcare services must be informed by Indigenous community members to ensure that these practices best meet local needs[65-70].
Conclusion
This review documents significant public health concerns with respect to maternal health among Indigenous populations in Canada, and supports the idea that there are opportunities to enhance maternal health outcomes. The knowledge acquired from the literature should be utilized in the development of community driven studies, which may allow for further comprehension of the topic. This will provide opportunities to collaborate with members of Indigenous communities who are seeking to improve the status of maternal health. Therefore, with enhanced understanding of the challenges and community collaboration, woman-centered and culturally safe maternal health programs and initiatives may be developed to reduce the existing disparities and achieve greater maternal health equity for Canadian Indigenous peoples. Further study in the maternal healthcare field could include evaluations of policies and strategies that correspond with the suggestions highlighted in this review.
Ethical Approval
Research ethics approval was not necessary for this systematic review.
Acknowledgement
The authors gratefully acknowledge Dr. André Corriveau, Chief Public Health Officer, Department of Health and Social Services, Government of the Northwest Territories, and Dr. Wadieh Yacoub, Director of Health Protection, First Nations and Inuit Health Branch – Alberta Region, Health Canada, who reviewed the manuscript and offered critical comments.
Source Of Funding
This study was funded by the Canadian Institute of Health Research.
Conflict of Interest
The authors declare that there is no potential competing or conflicting interests.
References
- World Health Organization (2014a) Health topics: Maternal health.
- World Health Organization (2014b) Accountability for women's and children's health recommendations 2:Healthindicators.
- Public Health Agency of Canada. (2013) Maternal mortality in Canada.
- Luo ZC, Senecal S, Simonet F (2010) Birth outcomes in the Inuit-inhabited areas of Canada(Research). CMAJ.182:235-242.
- Oliveira AP, Kalra S, Wahi G (2013) Maternal and new-born health profile in a first nations community in Canada. Journal of Obstetrics and Gynaecology Canada.35:905-913
- Trevors TM, Gray-Donald K. (2001) Neonatal morbidity among macrosomic infants in the James Bay Cree population of northern Quebec.
- Heaman MI, Chalmers K (2005) Prevalence and correlates of smoking during pregnancy: A comparison of aboriginal and non-aboriginal women in Manitoba. Birth.32:299-305
- Stout R,Harp R (2009) Aboriginal maternal and infant health in Canada: Review of on-reserve programming. Prairie Women's Health Centre of Excellence (PWHCE) and the British Columbia Centre of Excellence for Women’s Health.
- Shah PS, Zao J, Al-Wassia H (2011) Pregnancy and neonatal outcomes of aboriginal women: A systematic review and meta-analysis. Womens Health Issues. 21:28-39
- Statistics Canada. Aboriginal identity population by age groups, median age and sex, percentage distribution for both sexes, for Canada, provinces and territories - 20% sample data.
- Canadian Institute for Health Information (2006) Giving birth in Canada: The costs.
- Public Health Agency of Canada (2009) What mothers say: The Canadian maternity experiences survey.
- Statistics Canada. Infant mortality rates, by province and territory (Both sexes). Statistics Canada.
- Public Health Agency of Canada (2008) Canadian perinatal health report.
- Mayo Clinic(2013) Tween and teen health.
- Government of Nunavut Department of Health and Social Services (2010) Nunavut maternal and new-born health care strategy.
- Public Health Agency of Canada (2010) HIV/AIDS Among aboriginal people in Canada.
- Hamlin-Douglas LK, Coutlee F, Roger M (2010) Determinants of human papillomavirus infection among Inuit women of northern Quebec, Canada. Sexually Transmitted Diseases.37:377-381
- Healey SM, Aronson KJ, Mao Y (2001) Oncogenic human papillomavirus infection and cervical lesions in aboriginal women of Nunavut, Canada. Sexually Transmitted Diseases.28:694-700
- Wenman WM, Joffres MR, Tataryn IV (2004) A prospective cohort study of pregnancy risk factors and birth outcomes in Aboriginal women. CMAJ.171:585-589
- Reading CL, Wien F (2009) Health inequalities and social determinants of aboriginal peoples' health. National Collaborating Centre for Aborginal Health.
- Briere JN, Scott C (2006) Principles of trauma therapy: A guide to symptoms, evaluation and treatment Thousand Oaks, CA, SAGE.
- Duran E (2006) Healing the soul wound: Counseling with American Indians and other Native peoples New York, NY, Teachers College Press.
- Heart M (2003) The historical trauma response among Natives and its relationship with substance abuse: A Lakota illustration. Journal of Psychoactive Drugs.35:7-13
- Kirmayer LJ, Brass GM, Tait CL (2000) The mental health of Aboriginal peoples: Transformations of identity and community. Canadian Journal of Psychiatry.45: 607-616
- Morrissette PJ (1994) The holocaust of First Nation people: Residual effects on parenting and treatment implications. Contemporary Family Therapy.16:381-392
- Strickland CJ, Walsh E, Cooper M. (2006) Healing fractured families: Parents' and elders' perspectives on the impact of colonization and youth suicide prevention in a pacific northwest American Indian tribe. Journal of Transcultural Nursing.17:5-12
- Evans-Campbell T (2008) Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families and communities. Journal of Interpersonal Violence.23:316-338
- Dickson G (2000) Aboriginal grandmothers' experience with health promotion and participatory action research. Qualitative Health Research.10:188-213
- Medved MI, Brockmeier J, Morach J (2013) Broken heart stories: Understanding Aboriginal women's cardiac problems. Qualitative Health Research.23:1613-1625
- LaRocque E (2007) "Métis and feminist: Ethical reflections on feminism, human rights and decolonization," In Making Space for Indigenous Feminism, Fernwood.
- Batal M, Gray-Donald K, Kuhnlein H (2005) Estimation of traditional food intake in indigenous communities in Denedeh and the Yukon. International Journal of Circumpolar Health.64:46-54
- Blanchet C, Dewailly E, Ayotte P (2000) Contribution of selected traditional and market foods to the diet of Nunavik Inuit women. Canadian Journal of Dietetic Practic and Research.61:50-59
- Dewailly E, Blanchet C, Lemieux S (2001) n-3 Fatty acids and cardiovascular disease risk factors among the Inuit of Nunavik. American Journal of Clinical Nutrition.74:464-473
- Hopping BN, Erber E, Mead E (2010) Socioeconomic indicators and frequency of traditional food, junk food and fruit and vegetable consumption amongst Inuit adults in the Canadian Arctic. Journal of Human Nutrition and Dietetitcs.23:51-58
- Kuhnlein HV, Receveur O (2007) Local cultural animal food contributes high levels of nutrients for Arctic Canadian Indigenous adults and children. JNutr.137:1110-1114.
- Kuhnlein H, Chan H, Leggee D (2002) Macronutrient, mineral and fatty acid composition of Canadian Arctic traditional food. Journal of Food Composition Arctic Traditional Food. 15: 545-566
- Messer E (1989) Methods for studying determinants of food intake. Food and Nutrition Bulletin.11:1-33.
- Sharma S, Cao X, Roache C (2010) Assessing dietary intake in a population undergoing a rapid transition in diet and lifestyle: The Arctic Inuit in Nunavut, Canada. British Journal of Nutrition.103:749-759.
- Sharma S, De RE, Cao X (2009) Dietary intake in a population undergoing a rapid transition in diet and lifestyle: The Inuvialuit in the Northwest Territories of Arctic Canada. Canadian Journal of Public Health.100:442-448
- Wein EE (1995) Evaluating food use by Canadian aboriginal peoples. Canadian Journal of Physiology and Pharmacology.73:759-764
- Willows N, Veugelers P, Raine K (2011) Associations between household food insecurity and health outcomes in the Aboriginal population (excluding reserves). Health Reports. 22:15-20
- Birch J, Ruttan L, Muth T (2009) Culturally competent care for aboriginal women: A case for culturally competent care for aboriginal women giving birth in hospital settings. The Journal of Aboriginal Health.4:24-33
- Bird P; National Aboriginal Health Organization (2006) Exploring models for quality maternity care in First Nations and Inuit communities: A preliminary needs assessment, National Aboriginal Health Organization, editor.
- Herk KA, Smith D, Andrew C (2010) Identity matters: Aboriginal mothers' experiences of accessing health care. Contemporary Nurse.37:57-68
- Varcoe C, Brown H, Calam B (2013) Help bring back the celebration of life: A community-based participatory study of rural Aboriginal women's maternity experiences and outcomes. BMC: Pregnancy and Childbirth. 13.
- Hamlin-Douglas LK, Coutlee F, Roger M (2008) Prevalence and age distribution of human papillomavirus infection in a population of Inuit women in Nunavik, Quebec. Cancer Epidemiology, Biomarkers & Prevention.17:3141-3149.
- Messier V, Levesque B, Proulx JF (2009) Seroprevalence of Toxoplasma gondii among Nunavik Inuit (Canada). ZoonosesPublic Health.56:188-197.
- Kolahdooz F, Mathe N, Katunga LA (2013) Smoking and dietary inadequacy among Inuvialuit women of child bearing age in the Northwest Territories, Canada. Nutrition Journal.12:27.
- Robinson G, Conry J, Conry R. (1987) Clinical profile and prevalence of fetal alcohol syndrome in an isolated community in British Columbia. Canadian Medical Association Journal.137:203-207.
- Square D (1997) Fetal alcohol syndrome epidemic on Manitoba reserve. Canadian Medical Association Journal.157:59-60.
- Boucher O, Bastien CH, Saint-Amour D (2010) Prenatal exposure to methylmercury and PCBs affects distinct stages of information processing: An event-related potential study with Inuit children. Neurotoxicology.31:373-384.
- Butler WJ, Houseman J, Seddon L (2006) Maternal and umbilical cord blood levels of mercury, lead, cadmiumand essential trace elements in Arctic Canada. Environmental Research.100:295-318.
- Despres C, Beuter A, Richer F (2005) Neuromotor functions in Inuit preschool children exposed to Pb, PCBs and Hg.Neurotoxicology and Teratology.27:245-257.
- Fraser S, Muckle G, Despres C (2006) The relationship between lead exposure, motor function and behaviour in Inuit preschool children. Neurotoxicology and Teratology.28:18-27.
- Plusquellec P, Muckle G, Dewailly E (2010) The relation of environmental contaminants exposure to behavioral indicators in Inuit preschoolers in Arctic Quebec. Neurotoxicology.31:17-25.
- Neufeld H, Marchessault G (2004) Perceptions of 2 generations of Aboriginal women on causes of diabetes during pregnancy. Canadian Journal of Diabetes.28:1-8.
- Chamberlain M, Barclay K (2000) Psychosocial costs of transferring indigenous women from their community for birth. Midwifery. 16:116-122.
- Denison J, Varcoe C, Browne AJ (2014) Aboriginal women's experiences of accessing health care when state apprehension of children is being threatened. Journal of Advanced Nursing.70:1105-1116.
- Di Lallo S (2014) Prenatal care through the eyes of Canadian aboriginal women. Nursing for Women’s Health. 18:38-46.
- Neufeld HT (2011) Food perceptions and concerns of aboriginal women coping with gestational diabetes in Winnipeg, Manitoba. Journal of Nutrition Education and Behavior.43:482-491.
- Neufeld HT (2014) Patient and caregiver perspectives of health provision practices for First Nations and Metis women with gestational diabetes mellitus accessing care in Winnipeg, Manitoba. BMC Health Services Research.14: 440.
- Tait CL (2013) Resituating the ethical gaze: Government morality and the local worlds of impoverished Indigenous women. International Journal of Circumpolar Health. 72.
- Borland T, Babayan A, Irfan S (2013). Exploring the adequacy of smoking cessation support for pregnant and postpartum women. BMC Public Health.13:472.
- Brown H, Varcoe C, Calam B (2011). The birthing experiences of rural Aboriginal women in context: implications for nursing. Canadian Journal of Nursing Research.43:100-117.
- Eni R, Phillips-Beck W, Mehta P (2014) At the edges of embodiment: Determinants of breastfeeding for first nations women. Breastfeeding Medicine.9:203-214.
- Smith D, Edwards N, Varcoe C (2006) Bringing safety and responsiveness into the forefront of care for pregnant and parenting aboriginal people. Advances in Nursing Science. 29:E27-E44.
- Vallianatos H, Brennand EA, Raine K (2006) Beliefs and practices of First Nation women about weight gain during pregnancy and lactation: Implications for women's health. Canadian Journal of Nursing Research.38: 102-119.
- Wilson D, de la Ronde S, Brascoupe S (2013) Health professionals working with First Nations, Inuit and Metis consensus guideline. Journal of Obstetrics and Gynaecology Canada.35:550-558.
- Baker PR, Shipp JJ, Wellings SH (2012) Assessment of applicability and transferability of evidence-based antenatal interventions to the Australian indigenous setting. Health Promotion International.27:208-219.
- Campbell D, Pyett P, McCarthy L (2007) Community development interventions to improve Aboriginal health: building an evidence base. Health Sociology Review.16:304-314.
- O'Driscoll T, Kelly L, Payne L (2011) Delivering away from home: The perinatal experiences of First Nations women in northwestern Ontario. Canadian Journal of Rural Medicine.16:126-130.
- Kornelsen J, Kotaska A, Waterfall P (2010) The geography of belonging: The experience of birthing at home for First Nations women. Health & Place.16:638-645.
- Adler AI, Boyko EJ, Schraer CD (1994) Lower prevalence of impaired glucose tolerance and diabetes associated with daily seal oil or salmon consumption among Alaska Natives. Diabetes Care.17:1498-1501.
- Bersamin A, Luick BR, Ruppert E (2006). Diet quality among Yup'ik Eskimos living in rural communities is low: The Center for Alaska Native Health Research: Pilot Study. Journal of the American Dietetic Association.106:1055-1063.
- Ebbesson SO, Adler AI, Risica PM (2005) Cardiovascular disease and risk factors in three Alaskan Eskimo populations: the Alaska-Siberia project. International Journal of Circumpolar Health.64:365-386.
- Sheehy T, Kolahdooz F, Roache C (2014) Changing dietary patterns in the Canadian Arctic: Frequency of consumption of foods and beverages by inuit in three Nunavut communities. Food and Nutrition Bulletin.35:244-252.
- Larson B, Herx L, Williamson T (2011) Beyond the barriers: Family medicine residents' attitudes towards providing Aboriginal health care. Medical Education.45:400-406.
- Kendall E, Barnett L (2014) Principles for the development of Aboriginal health interventions: Culturally appropriate methods through systemic empathy. Ethnicity & Health.1-16.
- Lowell A, Kildea S, Liddle M (2015) Supporting aboriginal knowledge and practice in health care: lessons from a qualitative evaluation of the strong women, strong babies, strong culture program. BMC Pregnancy.
- Richards J, Mousseau A (2012) Community-based participatory research to improve preconception health among Northern Plains American Indian adolescent women. American Indian and Alaska Native Mental Health Research.19:154-185.
- Ruiz MJ, van Dijk MG, Berdichevsky K (2013) Barriers to the use of maternity waiting homes in indigenous regions of Guatemala: A study of users' and community members' perceptions. Culture, Health & Sexuality.15:205-218.
- Tucker K, Ochoa H, Garcia R (2013) The acceptability and feasibility of an intercultural birth center in the highlands of Chiapas, Mexico. BMC Pregnancy and Childbirth. 13: 94.
- Van DM, Ruiz MJ, Letona D (2013) Ensuring intercultural maternal health care for Mayan women in Guatemala: A qualitative assessment. Culture, Health & Sexuality. 15: S365-S382.
- Van WV, Epoo B, Nastapoka (2007) Reclaiming birth, health, and community: Midwifery in the Inuit villages of Nunavik, Canada. JMidwifery Womens Health.54:384-391.
- Hole RD, Evans M, Berg LD (2015) Visibility and voice: Aboriginal people experience culturally safe and unsafe health care. Qualitative Health Research.
- Homer CS, Foureur MJ, Allende T (2012) 'It's more than just having a baby' women's experiences of a maternity service for Australian Aboriginal and Torres Strait Islander families. Midwifery.28:E449-E455.
- Van WV, Osepchook C, Harney E (2012) Remote midwifery in Nunavik, Quebec, Canada: Outcomes of perinatal care for the Inuulitsivik health centre. Birth.39:230-237.
- Wong R, Herceg A, Patterson C (2011) Positive impact of a long-running urban Aboriginal medical service midwifery program. Australian Journal of Public Health.51:518-522.
- Jan S, Conaty S, Hecker R (2004) An holistic economic evaluation of an Aboriginal community-controlled midwifery programme in Western Sydney.Journal of Health Services Research & Policy.9:14-21.
- Prater SL, Davis CL (2002) A perinatal intervention program for urban american indians part 2: The story of a program and its implications for practice. Journal of Perinatal Education.11:23-32.
- Panaretto KS, Muller R, Patole S (2002) Is being Aboriginal or Torres Strait Islander a risk factor for poor neonatal outcome in a tertiary referral unit in north Queensland? Journal of Paediatrics and Child Health.38:16-22.
- Gamlin B, Hawkes J (2015) Pregnancy and birth in an indigenous Huichol community: From structural violence to structural policy responses. Culture, Health & Sexuality.17:78-91.
- Muggah E, Way D, Muirhead M (2004) Preterm delivery among Inuit women in the Baffin Region of the Canadian Arctic. International Journal of Circumpolar Health.63:242-247.
- Arbour L, Gilpin C, Millor-Roy V (2004) Heart defects and other malformations in the Inuit in Canada: A baseline study. International Journal of Circumpolar Health.63:251-266.
- Cnattingius S (2004) The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics and pregnancy outcomes. Nicotine & Tobacco Research.6:S125-S140.
- Mehaffey K, Higginson A, Cowan J (2010) Maternal smoking at first prenatal visit as a marker of risk for adverse pregnancy outcomes in the Qikiqtaaluk (Baffin) Region. Rural and Remote Health.10:1484.
- Najman JM, Williams GM, Bor W (1994) Obstetrical outcomes of aboriginal pregnancies at a major urban hospital. Australian Journal of Public Health.18:185-189.
- Couchie C, Sanderson S (2007) A report on best practices for returning birth to rural and remote aboriginal communities. Journal of Obstetrics and Gynaecology Canada.29:250-260.
- Wilson K (2003) Therapeutic landscapes and First Nations peoples: An exploration of culture, health and place. Health & Place.9:83-93.