Research Article - (2017) Volume 0, Issue 0
Shweta Chauhan* and Seema Singh Parmar
Department of Psychiatry, Teerthanker Mahaveer Medical College & Research Centre, Teerthanker Mahaveer University, Moradabad, Uttar Pradesh, India
*Corresponding Author:
Shweta Chauhan
Post-graduate Student
Department of Psychiatry
Teerthanker Mahaveer Medical College & Research Centre
Teerthanker Mahaveer University
Moradabad, Uttar Pradesh-244001, India
Tel: 096587 92858
E-mail: shwetachauhan29@gmail.com
Received Date: October 19, 2017; Accepted Date: November 06, 2017; Published Date: November 13, 2017
Citation: Chauhan S, Parmar SS (2017) Attitudes and Beliefs of Medical Students towards Individuals with Mental Illness: A Multice ntric, Cross Sectional Study. Acta Psychopathol 3:80. doi: 10.4172/2469-6676.100152
Aims & Objectives: To determine the levels of stigma as perceived by medical students across various professional years and to compare the beliefs of medical students regarding mental illness between private and government universities.
Methodology: 100 students belonging to a government medical college and 100 students belonging to a private medical college in North India were asked to fill a questionnaire regarding the demographic details, etiology, symptomatology of psychiatric disorders and Belief Towards Mental Illness Scale. Results were tabulated using dependent and single sample t-tests.
Results: Significant differences were seen amongst the students belonging to both the institutes regarding Phobias, Anxiety, Alcoholism and Drug addiction, with students of private medical college showing more negative views. Lower levels of stigmatizing views were seen in students with a history of prior psychiatric teaching.
Conclusion: Significant levels of stigma and negative belief have been seen in students belonging to both government and private medical colleges especially in private setup and psychiatric teaching imparted as early as possible during the course of medical training can reduce the negative beliefs of students and thus further facilitate in treatment and care of people suffering from psychiatric illnesses.
Keywords
Stigma; Beliefs; Attitudes; Medical students
Introduction
Stigma is defined as a mark of disgrace or dishonour associated with a particular circumstance, quality or person. Amongst various illnesses, mental illnesses are considered to be the most widely stigmatized [1]. Global studies done on general population demonstrate the beliefs and attitudes of people towards mental illnesses especially Schizophrenia, Alcohol use disorder and substance use disorder, with the latter two being largely considered not illnesses but rather a personality trait or a life style choice [2].
Medical students are widely considered as the first contact a patient with any illness (be it psychiatric or non-psychiatric) has with a medical professional. Various studies have shown stigmatizing views of medical students towards the mentally ill, but a vast majority of this literature has originated in the western hemisphere, with only a handful of studies being conducted in South East Asia, especially India [3].
Our study aims to evaluate the stigmatizing views of medical students, in both government and private universities in India, towards mental illnesses – the necessity of diagnosis and the prognosis of such patients as perceived by the future health professionals of the nation, in varied setups.
Methodology
200 medical students across various years of medical curriculum, belonging to two different institutions, one a government university and the other a private university, were asked to fill a self-structured questionnaire regarding various demographic details of the participant and Beliefs towards Mental Illness Scale(BMI) [4] after obtaining due consent.
It was a cross sectional study conducted during the period of October 2016 – December 2016, and all the individuals not wishing to participate in the study or not willing to provide a written informed consent were excluded from the study.
Both the questionnaires were in English language as the study is only comprising of participants who are being educated in the same medium.
The following instruments were used in the study:
1. A self-structured questionnaire regarding the demographic details of the students, knowledge regarding mental illnesses, contact with mental illnesses and history of psychiatric posting.
2. Beliefs towards Mental Illness Scale (BMI) – which is a 21 item self-reporting measure of negative and stereotypical views towards mental illness.
SPSS v20 was used to analyse all the data collected and means were calculated using single sample t-test and independent sample t-tests.
Results
100 students each from a government and private medical college participated in the study. The mean age of the participating students was 21.14 ± 1.94 from the government institute and 21.15 ± 1.38 for those participating from the private institute. Out of the 100 participants from government institute, 61 were males and 39 were females. Gender wise distribution for the participants from private institution was equal.
The mean score of private university students on Belief Towards Mental Illness was 50.59 (Standard deviation 15.475, error mean 1.548), whereas those of government university students was 49.91 (Standard deviation 16.963, error mean 1.696). On independent sample T-test, the difference between the above two mean values did not come out to be significant (p=0.767 at 95% CI of the difference). However, when single sample T-test was applied to total Belief Towards Mental Illness Scale scores with the test value of 30, results were calculated at 95% CI and they showed significant deviation with lower limit of 17.99 and upper limit of 22.51 (Table 1).
| Test Value = 30 | |||||||
|---|---|---|---|---|---|---|---|
| t | Df | Sig. (2-tailed) | Mean difference | 95% confidence interval of the difference | |||
| Lower | Upper | ||||||
| Total | 17.679 | 199 | 0.000 | 20.250 | 17.99 | 22.51 | |
Table 1: One-sample test of all 200 students comparing the total scores on belief towards mental illness.
The total number of males participating in the study was 112 compared to 88 females. The mean score for Belief Towards Mental Illness Scale did not vary significantly when compared with the gender of the participating students (p=0.813 at 95% CI).
Students were inquired as to which of the following 10 disorders, according to them, were psychiatric in nature: Phobias, Anxiety, Mania, Depression, Schizophrenia, Mental Retardation, Epilepsy, Obsessive Compulsive Disorder, Alcoholism and Drug Addiction. Significant results were obtained for Phobias, Anxiety, Alcoholism and Drug Addiction, with majority of the students of private institute believing that these four disorders were not psychiatric in nature and hence did not need psychiatric attention or treatment (Table 2 and Figure 1).
| Independent Samples Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Levene’s test for equality of variances | t-test for equality of means | |||||||||
| F | Sig. | t | df | Sig. (2-tailed) | Mean difference | Std. error differences | 95% confidence interval of the difference | |||
| Lower | Upper | |||||||||
| Phobia MI or not | Equal variances assumed | 14.178 | 0.000 | -2.911 | 198 | 0.004 | -0.200 | 0.069 | -0.335 | -0.065 |
| Equal variances not assumed | -2.911 | 197.075 | 0.004 | -0.200 | 0.069 | -0.335 | -0.065 | |||
| Anxiety MI or not | Equal variances assumed | 45.231 | 0.000 | -4.291 | 198 | 0.000 | -0.280 | 0.065 | -0.409 | -0.151 |
| Equal variances not assumed | -4.291 | 191.382 | 0.000 | -0.280 | 0.065 | -0.409 | -0.151 | |||
| Mania MI or not | Equal variances assumed | 2.384 | 0.124 | 0.769 | 198 | 0.443 | 0.040 | 0.052 | -0.063 | 0.143 |
| Equal variances not assumed | 0.769 | 195.981 | 0.443 | 0.040 | 0.052 | -0.063 | 0.143 | |||
| Depression MI/not | Equal variances assumed | 0.170 | 0.681 | 0.206 | 198 | 0.837 | 0.010 | 0.049 | -0.086 | 0.106 |
| Equal variances not assumed | 0.206 | 197.807 | 0.837 | 0.010 | 0.049 | -0.086 | 0.106 | |||
| Schizophrenia MI/not | Equal variances assumed | 3.955 | 0.048 | 0.986 | 198 | 0.325 | 0.040 | 0.041 | -0.040 | 0.120 |
| Equal variances not assumed | 0.986 | 190.295 | 0.325 | 0.040 | 0.041 | -0.040 | 0.120 | |||
| MR MI/not | Equal variances assumed | 14.829 | 0.000 | 1.919 | 198 | 0.056 | 0.120 | 0.063 | -0.003 | 0.243 |
| Equal variances not assumed | 1.919 | 194.052 | 0.056 | 0.120 | 0.063 | -0.003 | 0.243 | |||
| Epilepsy MI/not | Equal variances assumed | 0.886 | 0.348 | 0.564 | 198 | 0.573 | 0.040 | 0.071 | -0.100 | 0.180 |
| Equal variances not assumed | 0.564 | 197.995 | 0.573 | 0.040 | 0.071 | -0.100 | 0.180 | |||
| OCD MI/not | Equal variances assumed | 14.990 | 0.000 | 1.901 | 198 | 0.059 | 0.110 | 0.058 | -0.004 | 0.224 |
| Equal variances not assumed | 1.901 | 191.161 | 0.059 | 0.110 | 0.058 | -0.004 | 0.224 | |||
| Alcoholism MI/not | Equal variances assumed | 45.241 | 0.000 | -3.714 | 198 | 0.000 | -0.240 | 0.065 | -0.367 | -0.113 |
| Equal variances not assumed | -3.714 | 190.575 | 0.000 | -0.240 | 0.065 | -0.367 | -0.113 | |||
| Drug addiction MI/not | Equal variances assumed | 8.422 | 0.004 | -2.010 | 198 | 0.046 | -0.140 | 0.070 | -0.277 | -0.003 |
| Equal variances not assumed | -2.010 | 197.671 | 0.046 | -0.140 | 0.070 | -0.277 | -0.003 | |||
Table 2: Independent sample T-test of all 200 students to assess which illness is considered as a psychiatric disorder by medical students.
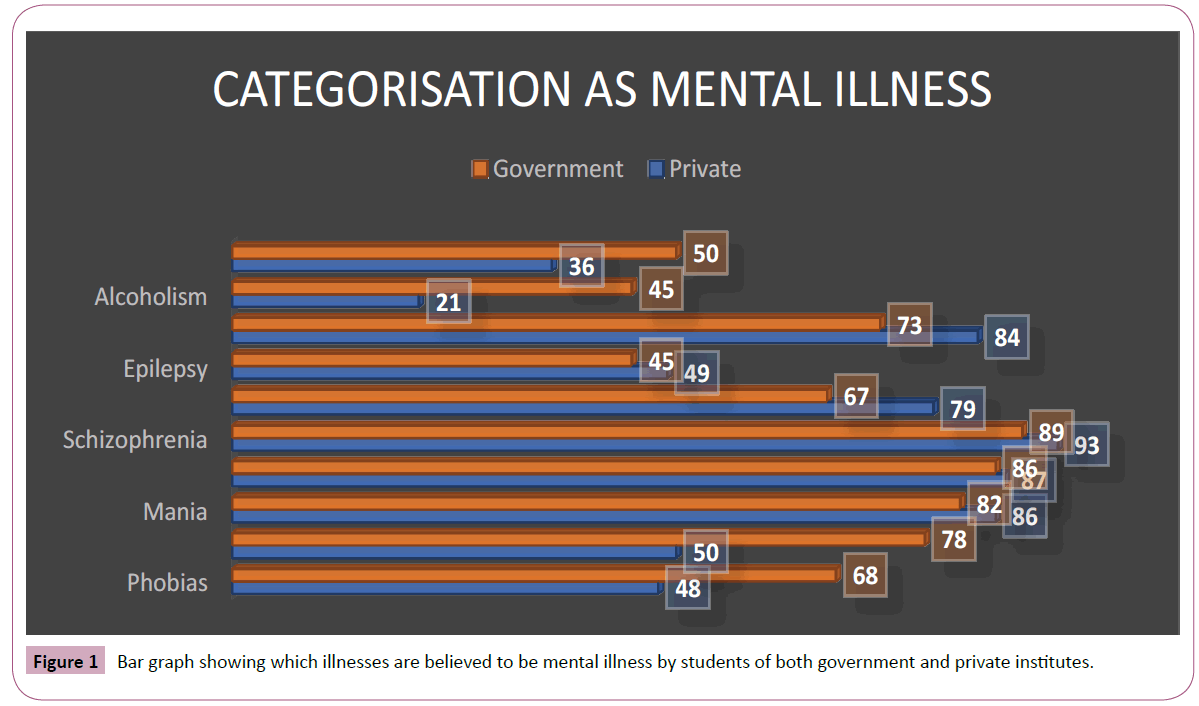
Figure 1: Bar graph showing which illnesses are believed to be mental illness by students of both government and private institutes.
When questioned regarding the etiological factors implicated in the causation of psychiatric illnesses, significant values were not obtained for any one variable, but more than half of the students both in government and private institutes, believed that infections could not be causally linked to any psychiatric disorder (Table 3 and Figure 2).
| Independent Samples Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Levene’s test for equality of variances | t-test for equality of means | |||||||||
| F | Sig. | t | df | Sig. (2-tailed) | Mean difference | Std. error difference | 95% confidence interval of the difference | |||
| Lower | Upper | |||||||||
| Genetic | Equal variances assumed | 7.327 | 0.007 | 1.344 | 198 | 0.181 | 0.080 | 0.060 | -0.37 | 0.197 |
| Equal variances not assumed | 1.344 | 195.045 | 0.181 | 0.080 | 0.060 | -0.37 | 0.197 | |||
| Life Events | Equal variances assumed | 8.557 | 0.004 | -1.434 | 198 | 0.153 | -0.050 | 0.035 | -0.119 | 0.019 |
| Equal variances not assumed | -1.434 | 175.105 | 0.153 | -0.050 | 0.035 | -0.119 | 0.019 | |||
| Personality | Equal variances assumed | 14.376 | 0.000 | -1.897 | 198 | 0.059 | -0.120 | 0.063 | -0.245 | 0.005 |
| Equal variances not assumed | -1.897 | 194.541 | 0.059 | -0.120 | 0.063 | -0.245 | 0.005 | |||
| Environmental Upbringing | Equal variances assumed | 9.498 | 0.002 | -1.525 | 198 | 0.129 | -0.090 | 0.059 | -0.206 | 0.026 |
| Equal variances not assumed | -1.525 | 193.999 | 0.129 | -0.090 | 0.059 | -0.206 | 0.026 | |||
| Drugs | Equal variances assumed | 11.215 | 0.001 | 1.659 | 198 | 0.099 | 0.100 | 0.060 | -0.019 | 0.219 |
| Equal variances not assumed | 1.659 | 193.949 | 0.099 | 0.100 | 0.060 | -0.019 | 0.219 | |||
| Infections | Equal variances assumed | 0.076 | 0.783 | 0.141 | 198 | 0.888 | 0.010 | 0.071 | -0.130 | 0.150 |
| Equal variances not assumed | 0.141 | 198.000 | 0.888 | 0.010 | 0.071 | -0.130 | 0.150 | |||
| Injury | Equal variances assumed | 5.322 | 0.022 | -1.149 | 198 | 0.252 | -0.070 | 0.061 | -0.190 | 0.050 |
| Equal variances not assumed | -1.149 | 196.149 | 0.252 | -0.070 | 0.061 | -0.190 | 0.050 | |||
| Structural Brain Damage | Equal variances assumed | 0.703 | 0.403 | -0.419 | 198 | 0.676 | -0.020 | 0.048 | -0.114 | 0.074 |
| Equal variances not assumed | -0.419 | 197.155 | 0.676 | -0.020 | 0.048 | -0.114 | 0.074 | |||
Table 3: Independent sample T-test of all 200 students to assess which variable is considered as an etiological factor of psychiatric disorders by medical students.
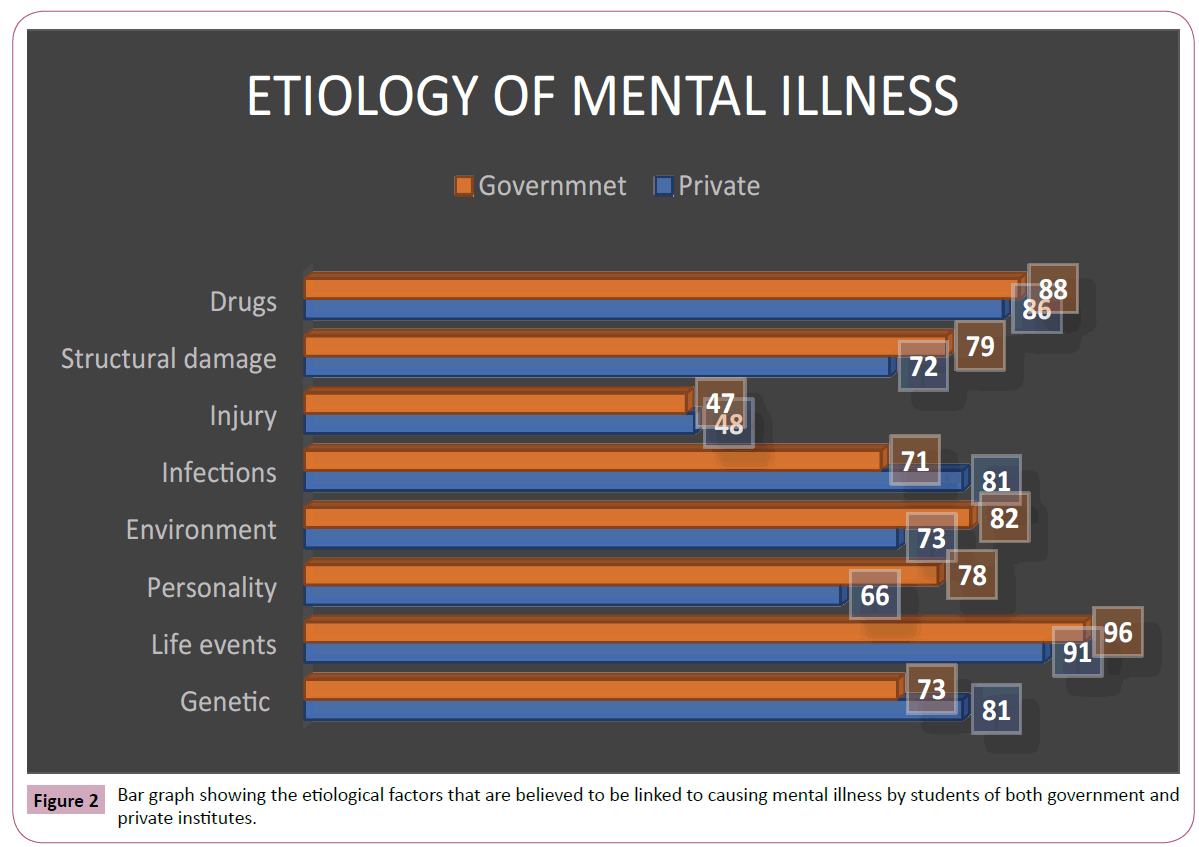
Figure 2: Bar graph showing the etiological factors that are believed to be linked to causing mental illness by students of both government and private institutes.
Students were also inquired as to which according to them were symptoms of a psychiatric illness. Following eight items were assessed: Unkemptness, Hallucinations, Delusions, Sadness, altered sleeping or eating habits, Feelings of Guilt, Poor concentration and Irrational fear. Significant values were obtained for only for guilt feelings (p=0.031), which according to almost half the students of private university, was not a feature of psychiatric illness. Though the difference was not significant, but more than half the students of both government and private colleges believed that unkemptness was not a feature of psychiatric illness (Table 4 and Figure 3).
| Independent Samples Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Levene’s test for equality of variances | t-test for equality of means | |||||||||
| F | Sig. | t | df | Sig. (2-tailed) | Mean difference | Std. error differences | 95% confidence interval of the difference | |||
| Lower | Upper | |||||||||
| Unkempt | Equal variances assumed | 9.845 | 0.002 | -1.744 | 198 | 0.083 | -0.120 | 0.069 | -0.256 | 0.016 |
| Equal variances not assumed | -1.744 | 197.374 | 0.083 | -0.120 | 0.069 | -0.256 | 0.016 | |||
| Hallucinations | Equal variances assumed | 7.005 | 0.009 | -1.305 | 198 | 0.194 | -0.060 | 0.046 | -0.151 | 0.031 |
| Equal variances not assumed | -1.305 | 189.036 | 0.194 | -0.060 | 0.046 | -0.151 | 0.031 | |||
| Delusions | Equal variances assumed | 0.884 | 0.348 | -0.469 | 198 | 0.639 | -0.020 | 0.043 | -0.104 | 0.064 |
| Equal variances not assumed | -0.469 | 196.444 | 0.639 | -0.020 | 0.043 | -0.104 | 0.064 | |||
| Sadness | Equal variances assumed | 4.109 | 0.044 | 1.032 | 198 | 0.303 | -0.070 | 0.068 | -0.064 | 0.204 |
| Equal variances not assumed | 1.032 | 197.608 | 0.303 | -0.070 | 0.068 | -0.064 | 0.204 | |||
| Eating/ Sleeping problems | Equal variances assumed | 3.190 | 0.076 | -0.900 | 198 | 0.369 | -0.060 | 0.067 | -0.192 | 0.072 |
| Equal variances not assumed | -0.900 | 197.576 | 0.369 | -0.060 | 0.067 | -0.192 | 0.072 | |||
| Guilt feelings | Equal variances assumed | 12.391 | 0.001 | -2.175 | 198 | 0.031 | -0.150 | 0.069 | -0.286 | -0.014 |
| Equal variances not assumed | -2.175 | 197.277 | 0.031 | -0.150 | 0.069 | -0.286 | -0.014 | |||
| Poor concentration | Equal variances assumed | 0.335 | 0.564 | -0.290 | 198 | 0.772 | -0.020 | 0.069 | -0.156 | 0.116 |
| Equal variances not assumed | -0.290 | 197.979 | 0.772 | -0.020 | 0.069 | -0.156 | 0.116 | |||
| Irrational fear | Equal variances assumed | 4.216 | 0.041 | -1.022 | 198 | 0.308 | -0.060 | 0.059 | -0.176 | 0.056 |
| Equal variances not assumed | -1.022 | 196.101 | 0.308 | -0.060 | 0.059 | -0.176 | 0.056 | |||
Table 4: Independent sample T-test of all 200 students to assess which variable is considered as a symptom of a psychiatric disorder by medical students.
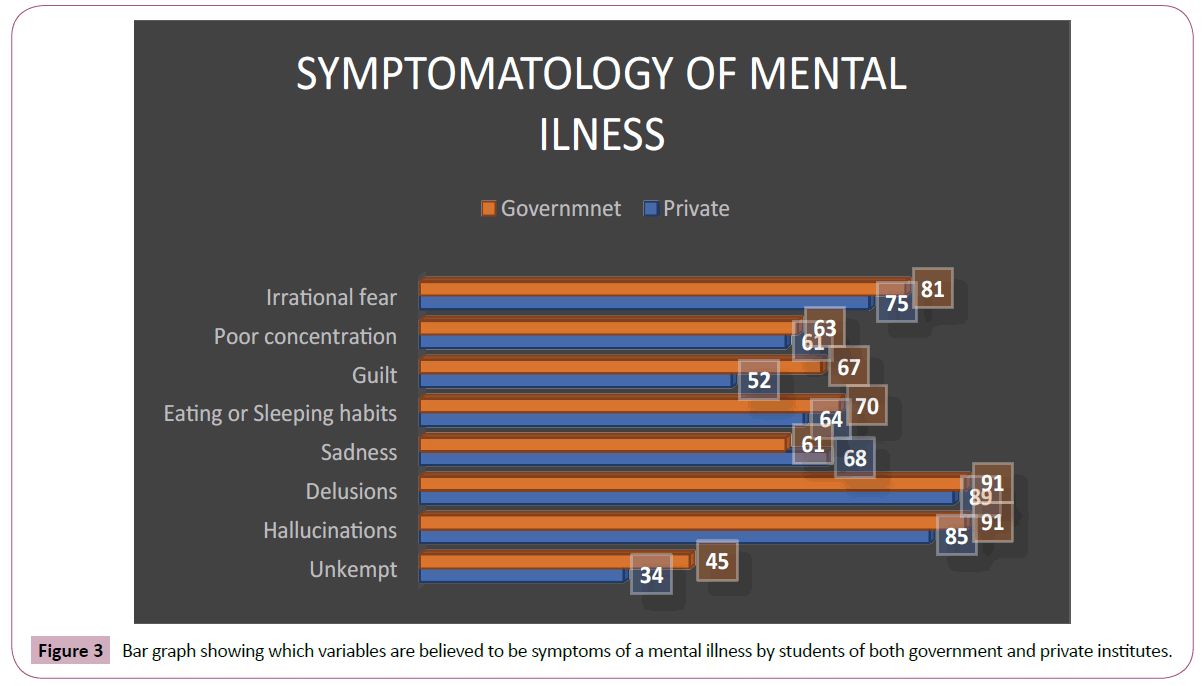
Figure 3: Bar graph showing which variables are believed to be symptoms of a mental illness by students of both government and private institutes.
Significant difference was also seen when total scores of Belief Towards Mental Illness Scale was compared with whether the students had undergone any sort of psychiatric teaching, be it clinical postings or theoretical lectures (Table 5).
| Independent Samples Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Levene’s test for equality of variances | t-test for equality of means | |||||||||
| F | Sig. | t | df | Sig. (2-tailed) | Mean difference | Std. error differences | 95% confidence interval of the difference | |||
| Lower | Upper | |||||||||
| H/O Psychiatric teaching | Equal variances assumed | 25.423 | 0.000 | 4.841 | 198 | 0.000 | 0.320 | 0.066 | 0.190 | 0.450 |
| Equal variances not assumed | 4.841 | 194.551 | 0.000 | 0.320 | 0.066 | 0.190 | 0.450 | |||
Table 5: Independent sample T-test of all 200 students comparing total score on belief towards mental illness scale with history of psychiatric teaching received by the students.
Discussion
According to the World Health Report published in 2001, 450 million individuals worldwide suffer from mental or behavioural disorders [5]. Despite this vast number, very few of these individuals seek medical help or get medical attention which can largely be attributed to the myths and misconceptions that are associated with psychiatric illnesses. It is also worthy of noting that while it is widely believed that these false notions might primarily be rooted in the developing world, most of the studies have been done in developed nations [6]. The association of stress and Depression has long been recognized but recent emerging evidences show that this takes place via the modulation of immune system and the Hypothalamo-Pituitary- Adrenal (HPA) axis. Abnormal response on both Dexamethasone Suppression Test and Corticotrophin Releasing Factor (CRF) administration reveal an upregulated HPA axis in depressed individuals. Furthermore, similar abnormalities have been seen in individuals exposed to significant early life stress [7]. Studies have also shown decreased CRF receptors, decreased CRF mRNA and elevated levels of CSF-CRF in brains of depressed patients [8]. It has been noted that the administration of TNFα in various infective and oncogenic disorders tends to produce a depression like syndrome in these patients, thus TNFα is considered to be the quintessential depressive cytokine [9].
According to a study conducted at a teaching hospital in London [10], more than 50% felt that people suffering from Schizophrenia or drug or alcohol addiction were dangerous and unpredictable, but the stigma appeared to be lessened as the experience of the medical professional increased. This finding has been corroborated in our study with most of the students giving higher scores on the questions related to dangerousness of the patient on the Belief Towards Mental Illness Scale.
In a survey circulated amongst the doctors of three medical colleges in Pakistan in 2006 [11], more than half of the respondents held negative attitudes towards people with mental illness, namely Schizophrenia, Depression and Alcohol or substance Use Disorder. Our study showed significant difference in stigmatising beliefs of government and private institute, with majority of the students of private medical college not regarding Phobias, Anxiety, Alcoholism and Drug addiction as psychiatric disorders. Students of both institutes did not show significant negative beliefs towards Depression or Schizophrenia as seen in the study conducted in Pakistan.
In a study conducted in New Delhi in 2012 [12] to assess the attitude and belief system of medical students across various years of medical curriculum, lower levels of negative beliefs were seen amongst intern as compared to the rest of the students. Our study also reports a similar finding as the levels of stigma were significantly lesser in students with a history of psychiatric teaching – clinical or theoretical. Similar trends in less negative belief with a history of psychiatric education were seen in students of both government and private institute. This finding is further affirmed by a follow up study conducted in Sri Lanka [13], in which significant decrease in stigmatising views of medical students was seen after a 6-week posting in Psychiatry.
A pioneering online survey which was conducted on 760 medical students in U.K [14] showed the students highest regard for patients with pneumonia and lowest for patients with long standing somatoform complaints. This shows that stigma regarding psychiatric illnesses is prevalent even in developed countries as opposed to less educated, developing nations.
Not much work has been done in comparing the stigmatising views of students belonging to government and private institutes and our study shows significant differences in beliefs of students towards all the aspects of psychiatric disorders, be it classification, etiology, symptomatology or attitude towards people with psychiatric illnesses.
Conclusion
There is paucity of available literature on the subject of stigma in psychiatric illnesses especially the studies conducted to assess the negative beliefs and attitudes of medical students towards people suffering from psychiatric illness. The few studies that have been done on the subject have shown alarming levels of stigmatising views in medical students of both developed and developing nations. This shows that the belief system of medical students belonging to both the kinds of nations is not limited by the general levels of education and awareness of the society they belong to. This trend shows that psychiatric teaching imparted as early as possible during the course of medical training can reduce the negative beliefs of students and thus further facilitate in treatment and care of people suffering from psychiatric illnesses.