Keywords
chronic pain, complexity, evidence base
Introduction
Healthcare practice is changing, and the foundations
of the paradigm shift lie in research developments
over the last four decades. It is no longer adequate to
provide healthcare grounded exclusively in clinical
experience, without a clear demonstration of a highquality
research evidence base. Evidence-based practice
(EBP) is the product of combining research evidence
with clinical knowledge and reasoning, professional
judgement and knowledge of patient characteristics
(Law and Baum, 1998). EBP evolved from evidencebased
medicine and now embraces the delivery of
all healthcare services. Sackett et al (1996) described
evidence-based medicine as ‘integrating clinical expertise
with the best available external clinical evidence
from systematic research’ (p. 71).
The movement towards EBP in the health service is
an issue that the present government of the UK has
highlighted in NHS reforms (NHS, 1997). Underpinning
EBP is the need to provide relevant training
for healthcare professionals enabling them to read and assimilate the evidence which is provided in the
literature, in order to make informed decisions about
their practice (Barnard and Wiles, 2001). To maintain
clinical effectiveness, all healthcare professionals should
engage in regular internal and external training programmes
to add to existing clinical skills, and to
offer scope for personal and professional development
(Dunning, 1995). However, this ongoing training is
not always evident, and there seem to be a number of
barriers to this process. With the condition of low back
pain, for example, physiotherapists tend to explore
their own personal training agendas, which leads to
a fragmented approach in relation to the condition
(Foster et al, 1999). Additionally, research has found
that most occupational therapists have very little
undergraduate knowledge of pain-related issues (see
for example Turnquist and Engel, 1994; Unrah, 1995;
Rochman, 1998; Rochman and Herbert, 1999; Strong
et al, 1999), and that also affects their readiness to
work with people who have chronic pain.
The process of change within clinical practice is a
fascinating area and rigorous, theory-driven research
of the area is still in its infancy. Some healthcare
professionals are slow to adopt clinical practice based
on scientific findings. Reasons include difficulties accessing
research literature (Dubouloz et al, 1999; Barnard
and Wiles, 2001), lack of time or knowledge required
to search for, read, interpret and evaluate relevant
reports (Pollock, 2000; Gervais et al, 2002; McCluskey,
2003), the belief that experience and expert opinion
are more important for competency than knowing the
results of research (Belanger, 1997), failure to recognise
the existence of guidelines based on evidence, and
institutional barriers to changing current practice (Funk
et al, 1995). More alarmingly, EBP is seen by some
clinicians as a potential threat to the routine ways of
analysing and carrying out therapeutic interventions
(Dubouloz et al, 1999). Some physiotherapy clinicians
believe that they solve clinical problems in practical
ways, and find it difficult to let go of the core skills that
they perceive as their domain, and change from current
practice to EBP (Pinnington, 2001). It has also been
reported that clinicians find the ‘current style of research
articles unhelpful and unreadable with recommendations
few of them are realistically able to work with
let alone understand’ (Mimms, 1996, p. 394).
For certain clinical conditions the literature is diverse,
extensive and, at times, contradictory. When this
happens the problem of accessing and evaluating the
‘evidence’ is compounded and presents a further barrier.
An example of this is chronic pain, and particularly
low back pain, a clinical condition frequently encountered
by therapists. Because of its multifaceted
presentation, many therapeutic approaches are used
in the management of chronic low back pain. Some
appear to be effective and some do not. Distinct
treatment approaches tend to target specific effects and outcomes. Manual therapy (mobilisation and/or
manipulation), for example, has been shown to be
effective in reducing pain levels (Andersson et al, 1999),
and specific exercise programmes have been shown
to be effective in reducing disability and increasing
performance (Klaber Moffett et al, 2000). However,
these approaches fail to directly address the psychosocial
aspects of chronic pain that are felt to be very
significant barriers to improvement.
An additional feature of chronic pain contributing
to the diversity of practice is the current preference
for a multidisciplinary team approach. Over the last
decade, there has been a significant move to manage
patients with chronic pain more actively and intensively
in multidisciplinary programmes (Frost, 1997).
Although the efficacy of this approach is widely
supported, there is significant variation in content
from one programme to another, creating a challenge
to the researcher in being able to isolate the strength of
the evidence for individual treatment components.
As Meijers et al (2006, p. 632) point out, ‘implementing
change, getting research into practice and
improving the quality of patient care are complex,
difficult, and demanding processes’. One of these
processes must be to identify key areas that are currently
under-researched, so that resources and energy
are focused where most needed. Chronic pain, because
it is a feature of so many chronic conditions, is such an
area for rehabilitation therapists.
Study aims and rationale
Delivering effective, evidence-based service is imperative
for therapists because of the large human and
economic cost of chronic pain. Chronic pain is recognised
as a significant problem within the industrialised
nations, and prevalence has been cited in European
and North American studies as between 12% and 35%
of the population at any one time, and 49–80%across
the life span (Elliott et al, 1999; Maniadakis and Gray,
2000). Research into the cost of illness arising from
back pain estimated the direct care costs in 1998 as
£1632 million. Including additional indirect costs,
such as carers and lost wages, the figure rose to
£10 668 million (Maniadakis and Gray, 2000). The
World Health Organization (WHO, 2002) reports
that chronic conditions like pain are increasing at an
alarming rate and will compose 60% of the global
disease burden by the year 2020. WHO stresses that
effective management of these conditions will require
a paradigm shift within both healthcare structures and
service providers. The question is to what extent
therapists have accurate information about chronic
pain interventions and what areas need attention to
allow that paradigm shift to occur? The aim of this
study is to provide a structured review of the evidence base for certain chronic pain interventions, and to
then determine to what extent occupational therapists’
and physiotherapists’ beliefs about these treatments
are grounded in this evidence. The findings are
discussed in relation to the current professional literature
pertaining to EBP, and will conclude with
recommendations for further study.
Methods
This study used existing survey data about the beliefs
held by occupational therapists and physiotherapists
regarding treatments for chronic pain. The therapists’
endorsements were examined in relation to the existing
evidence base for chronic pain treatments, as
itemised in a range of systematic reviews, to determine
whether therapists’ endorsements reflect the findings
of these reviews.
Therapists’ endorsements
Two sources of secondary data were accessed in order
to compare therapists’ endorsement patterns in relation
to the evidence base for chronic pain treatments.
The first, occupational therapist and physiotherapist
beliefs about what treatment components for chronic
pain are important, was extracted from a larger
multidisciplinary study (Brown, 2003) that examined
service provider and service user congruence of beliefs
regarding treatments for chronic pain. In Brown’s
study, participants were surveyed to identify which
treatment components they personally endorsed as
important or not important for people with chronic
pain. The survey also gathered basic demographic data
regarding age, gender, experience and training specific
to chronic pain. Beliefs about pain control were identified
using the Beliefs about Pain Control Questionnaire
(BPCQ; Skevington, 1990), and these findings
are reported elsewhere (Brown, 2003).
Source of evidence for treatment
effectiveness
The second item required for the comparison was an
overview of the existing evidence base for chronic
pain treatments. Again, secondary data were accessed
through a search for systematic reviews related to
specific treatments for chronic pain. The Health Technology
Assessment (HTA) report, Systematic Review of
Outpatient Service for Chronic Pain Control (McQuay
et al, 1997), served as a starting point to identify
treatment components for chronic pain where the
evidence base had been systematically reviewed. Electronic
databases were also reviewed for the period between the HTA publication and October 2002 when
therapists’ opinions about which treatments were
important were surveyed. Databases included AMED,
CINAHL and Medline. Search terms with variations
specific to the particular database included combinations
of professional practice, evidence base, systematic
review, occupational therapy, physiotherapy and physical
therapy. Chronic pain was not initially included as a
search term, as certain treatment components may
also be employed in other painful conditions. It was
thought that it would be useful to know what studies
on each treatment component had been carried out
regardless of diagnostic group. Occupational therapy,
physiotherapy and physical therapy were used as search
terms based on the assumption that therapists attend
to information within the discipline-specific literature
first.
The search, limited to English language publications,
retrieved seven hits relevant to the treatment
components identified in the survey. None of these
reviews were generalised to chronic pain overall.
However, they did focus on conditions where pain
of a chronic nature is a primary feature. These conditions
included fibromyalgia (Hadhazy et al, 2000),
osteoarthritis (Osiri et al, 2000), low back pain (van
Tulder et al, 2000b,c), shoulder pain (Green et al,
2000) and neck pain (White and Ernst, 1999).
To ensure comprehensiveness of the review a further
search was made on PsychInfo, IBSS and Medline
(between 1996 and 2002, English language only) with
the more general search terms of chronic pain and
systematic review. Seventeen additional hits were identified
after the duplicate references from the previous
searches were screened. These systematic reviews included
TENS (transcutaenous electrical nerve stimulation)
for people with phantom limb (Halbert et al,
2002), low back (Milne et al, 2001) and headache pain
(Vernon et al, 1999), gabapentin (anticonvulsant medication)
in neuropathic conditions (Mellegers et al,
2001), multidisciplinary service delivery (Guzman et al,
2001; Thomsen et al, 2001), homeopathy for headache
(Ernst, 1999b; Vernon et al, 1999), exercise for a
variety of pain sites (Mior, 2001), acupuncture (Ezzo
et al, 2000; Henderson, 2002), relaxation (Carroll and
Seers, 1998), topical non-steroidal creams (Moore et al,
1998), and antidepressants (McQuay et al, 1996).
Lastly, the British Medical Journal (BMJ) electronic
journal Clinical Evidence was searched for pain interventions
of interest within the musculoskeletal category.
The reviews of relevance to this paper included interventions
for shoulder pain (Speed and Hazleman,
2002), educational materials (Superio-Cabuslay et al,
1996), exercise, non-steroidal anti-inflammatories and
topical agents (Chard et al, 2002; Gotzsche, 2002; Scott
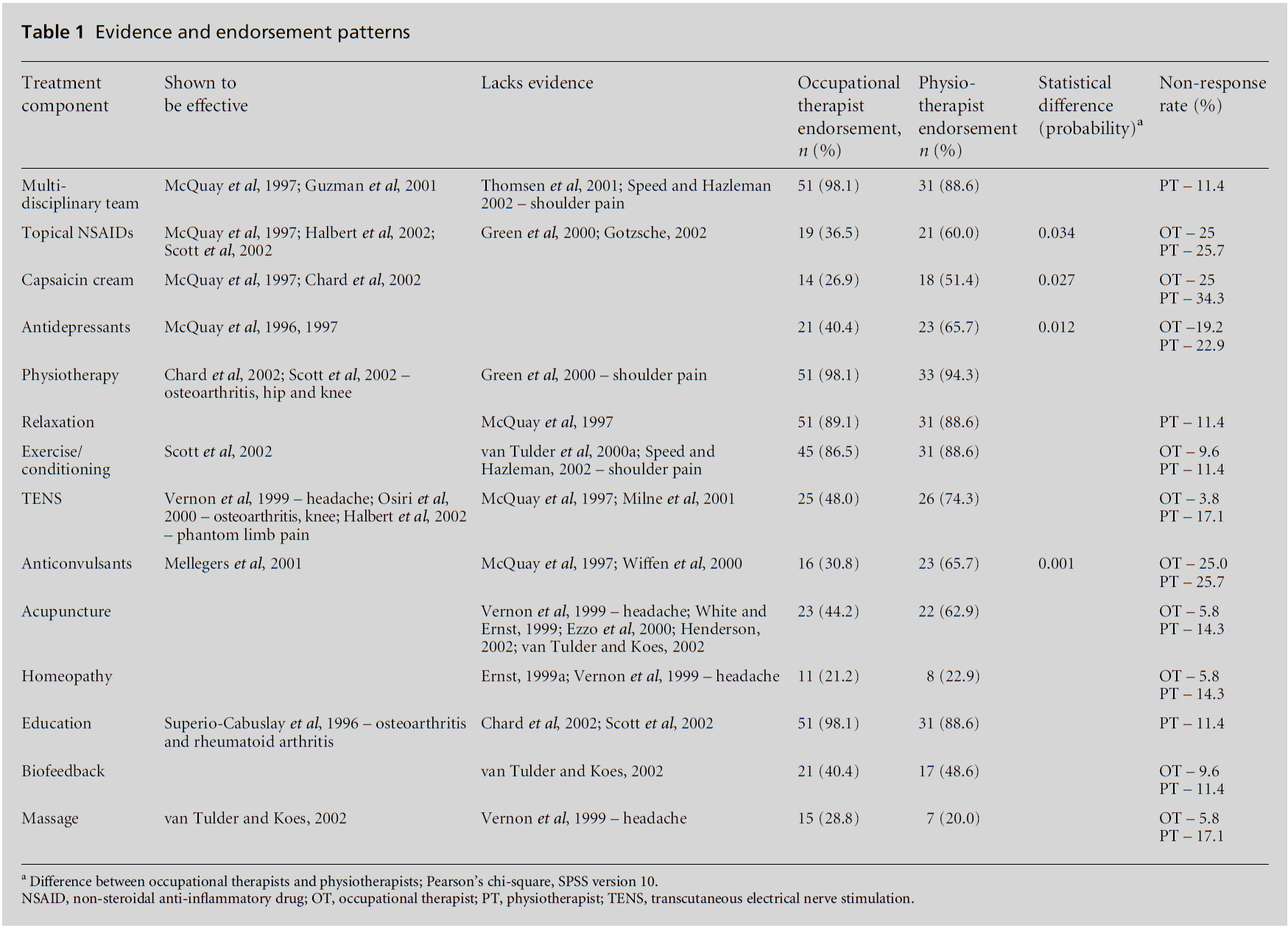
et al, 2002). Table 1 lists the 14 treatments for which
systematic reviews were obtained.
Table 1: Evidence and endorsement patterns.
Psychological interventions
The Health Technology Assessment carried out by
McQuay et al (1997) also attempted to review the
evidence related to components of psychological
approaches such as self-management education, goal
setting, problem solving, family involvement and coping
skills groups. However, because of the small number
of high-calibre studies and the lack of comparability,
they were unable to draw conclusions. A subsequent
systematic review (Morley et al, 1999) found that there
was sufficient evidence to conclude that active psychological
treatments based on the principles of cognitivebehavioural
therapy are effective interventions compared
to waiting list controls. However they, like
McQuay et al, were unable to comment on specific
treatment components delivered within highly variable
and complex treatment designs. They stressed the
importance of simple two-arm trials for future research
considerations. The search strategy outlined previously
identified additional systematic reviews covering a
range of cognitive-behavioural, psychological and
behavioural interventions for people with chronic
pain (Eccleston et al, 2002; Morley et al, 1999; van
Tulder et al, 2000b). However, the same problem with
being unable to isolate individual components of
psychological interventions was identified by the authors
of this paper. The occupational therapists and physiotherapists
in this study had been asked to comment on
specific treatment components such as assertiveness
training and art therapy, as opposed to the more
generic category of psychosocial interventions. So as to avoid misinterpreting and misrepresenting participants’
treatment endorsements, it was decided to
exclude these treatment components from the present
discussion.
Results
Therapists’ profile and endorsements
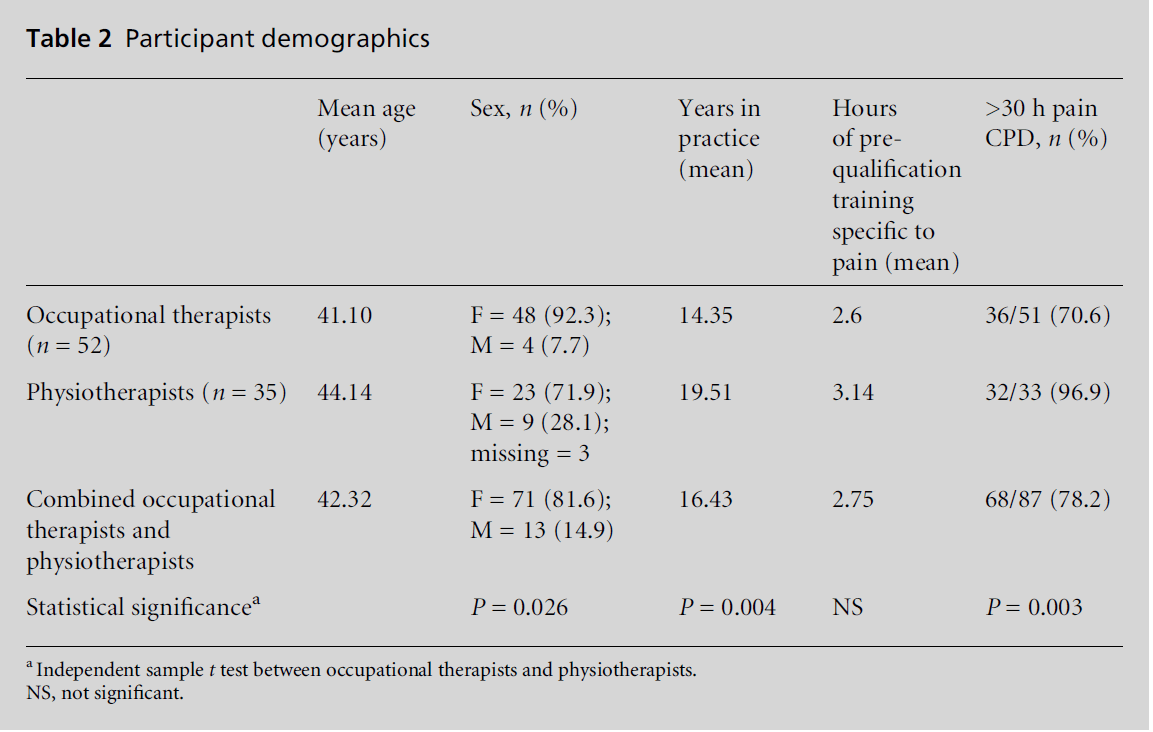
Sixty-two physiotherapists who were members of the
Pain Society-UK and 93 occupational therapists who
were members of the Pain Society and/or the National
Occupational Therapy Pain Association-UK received
a survey in the original study carried out by Brown
(2003). The response rate was 52 (55.9%) occupational
therapists and 35 (56.4%) physiotherapists,
with a demographic breakdown as illustrated in Table
2. No statistically significant differences were found
between occupational therapists and physiotherapists
for age, amount of undergraduate training and hours
of CPD related to chronic pain. The physiotherapy
respondents showed statistically significant differences,
identified through independent samples t test calculated
with SPSS version 10, from the occupational therapists
in both having a higher number of male respondents
(P = 0.026) and number of years in practice (P =
0.004).
Table 2: Participant demographics.
These British occupational therapy and physiotherapy
respondents had a wide range in hours of
undergraduate training, with 68.5% reporting that they had received no training in pain and pain management.
Only four (5.5%) of the total group had
received more than 20 hours of pain education at
undergraduate level. This finding is consistent with
other studies, where very low amounts of undergraduate
preparation for dealing with chronic pain
were identified (Unrah, 1995; Rochman, 1998; Strong,
et al, 1999). Interestingly, in contrast, only three therapists
(3.6%) reported having no additionalCPDtraining
in pain management, whereas 68 (78.2%) had participated
in over 30 hours of pain-related CPD.
The returned surveys were entered into SPSS Version
10 for descriptive statistical analysis. Because the
participants, through their membership in organisations
specialising in pain, were assumed to have
higher levels of knowledge than a general therapist,
the option of undecided was not available on the survey.
For certain treatment components the non-response
rate was high and needed to be taken into consideration
in statistical analysis. Where no selection was
made between important or not important, an entry
of non-response was made in the database. Complete
details of endorsements are published elsewhere (Brown,
2003).
The evidence base for chronic pain
treatments
When the available evidence for specific treatment
components was reviewed, capsaicin cream and antidepressants
were identified as treatments shown to be
effective through the systematic review process. The
systematic reviews of eight other treatment components
had mixed findings. Some concluded that the
treatment was effective; others determined that there
was a lack of evidence. These eight treatments include
multidisciplinary teams, topical non-steroidal antiinflammatory
drugs (NSAIDs), physiotherapy in certain
painful conditions, exercise/reconditioning activities,
TENS, anticonvulsant medication, and pain education.
Lastly, systematic reviews of the final four treatment
components (relaxation, acupuncture, homeopathy
and biofeedback) were found to lack an evidence base.
None of the 14 treatment component reviews concluded
that the treatmentwas showntobenot effective(Table1).
Comparing therapists’ endorsements
to the evidence base
This paper’s aim was to identify whether therapists
were evidence based in their endorsements for chronic
pain treatments. The findings are presented in Table 1,
comparing the two sources of secondary data discussed
above. Table 1 demonstrates whether a treatment
has been shown to be effective or if it lacks
evidence, and the percentage of therapists who endorsed each particular treatment. The second to last column
indicates any statistically significant difference (based
on Pearson’s chi-square) in the endorsement patterns
of occupational therapists and physiotherapists. The
final column shows the percentage of therapists who
failed to identify if they thought the treatment was
either important or not important.
A review of Table 1 indicates that both physiotherapists
and occupational therapists were evidence based
in their endorsements of the multidisciplinary team,
physiotherapy intervention, exercise/conditioning programmes
and the provision of education about pain. It
also appears that therapists were either not aware or
did not accept that topical NSAIDs, capsaicin cream,
antidepressants, TENS and anticonvulsants have been
demonstrated to be effective interventions. Neither
occupational therapists nor physiotherapists endorsed
the use of acupuncture, homeopathy and biofeedback.
This is consistent with the lack of evidence for these
interventions. However, therapists did quite strongly
endorse the treatment option of relaxation training,
despite a lack of evidence for its effectiveness.
As illustrated in Table 1, physiotherapists and occupational
therapists had statistically significant differences
in their endorsement for certain treatment
components. Cross-tabulation (based on Pearson’s
chi-square) of occupational therapists’ and physiotherapists’
endorsements for the three possible groupings
(important, not important, non-response) highlighted
statistically significant difference in beliefs about the
important of topical NSAIDs (P = 0.034), capsaicin
cream (P = 0.027), antidepressants (P = 0.012) and
anticonvulsants (P = 0.001). Physiotherapists, as opposed
to occupational therapists, were more likely to
select all of these treatment components as important.
Discussion
Limitations
The study is limited by the use of secondary data from
a study not originally intended to provide a comprehensive
systematic review of the evidence base for
interventions employed by therapists. Consequently
there are some interventions missing from the review.
Also the original endorsement data were gathered
several years prior to the review of the strength of
the evidence for these interventions, so it should be
assumed that the literature now might reflect different
strength ratings for certain interventions. These are all
reflective of how rapidly the information we all attempt
to base best practice upon can shift and reconfigure.
Also, the endorsement data were extracted from a
study with a small sample size and an inability to
determine demographic characteristics that may have influenced participation in the study. The respondents,
because of their membership in the Pain Society,
should be viewed as a subspecialist group that may
have a wider knowledge and experience base in chronic
pain than other therapists. Survey data do not capture
the full range of responses possible in exploring a
complex area such as pain, and it is possible that the
treatment components were not defined in sufficient
detail for some respondents and so assumptions about
a common meaning for some components cannot be
made. This postal survey focused on what therapists
endorsed, and so provided predominantly quantitative
data. As such, survey data are limited by both researcher
and respondent bias (Bowling, 1997) and
offer a limited range of information where the individual
voice can be lost in the aggregation of many
voices. The importance of exploring what values and
meanings the individual holds is reinforced by the
increasing focus on qualitative research methods in
highly regarded medical publications like the BMJ
(Mays and Pope, 1999, 2000). The findings reported
in this paper should be seen as a bridge into the more
specific examination of ‘why’ and not as definitive in
themselves. The second stage of this research is currently
being carried out and involves a Delphi process
in which both service users and service providers
explore what influences their decision making about
treatment importance, and also reflect on each other’s
opinions, beliefs and recommendations.
It seemed a simple question at
the time
The aim of this paper was to raise awareness of an
under-researched area through identifying whether
therapists were evidence based in their beliefs about
chronic pain treatments. ‘It seemed a simple question at
the time.’ However, the findings seem to raise more
questions than they answer. Why do therapists not
endorse some treatments despite a demonstrated
evidence base? Why do they continue to believe in
the importance of certain treatments that lack an
evidence base? Why are physiotherapists and occupational
therapists different in their endorsements,
and why do some therapists, despite membership
in pain specialist organisations, express no opinion
about certain treatments? Some possible influences
are explored in the following section.
Why are therapists not consistently
evidence based?
It is reassuring to discover that both physiotherapists
and occupational therapists readily endorse a multidisciplinary
format in the management of chronic
pain. The use of such a format to manage patients, where different professions bring individual skills to
patients with chronic pain, has been well recognised
among many for at least a decade. This format is well
supported in the literature (McQuay et al, 1997;
Guzman et al, 2001).
Anecdotal evidence, however, suggests that many
therapists not specialised in the management of chronic
pain continue to manage their patients with chronic
pain individually, in a non-multidisciplinary setting.
Reasons for this might include constraints in funding
and resources; there simply may not be enough multidisciplinary
programmes in existence.
Similarly, the treatment techniques that are traditionally
associated with multidisciplinary pain programmes
– physiotherapy, exercise and conditioning
programmes – and education about pain processes
and their effect on the body are all well endorsed by
both therapies, and are all supported to some extent
in the literature (Superio-Cabuslay et al, 1996; Chard
et al, 2002; Scott et al, 2002). Conversely, relaxation
techniques are also traditionally associated with chronic
pain management and were well endorsed by both
therapies in this survey, but the evidence to support
their use is lacking to date (McQuay et al, 1997).
Acupuncture, although less well endorsed by both
therapies than relaxation, is still seen to be an important
treatment for chronic pain by more than one-third
of physiotherapists despite a distinct lack of evidence
(White and Ernst, 1999; Ezzo et al, 2000).
This survey also highlighted some treatment components
for chronic pain that have varying degrees of
support in the literature, but are poorly endorsed by
the therapies. Topical NSAIDs (Halbert et al, 2002),
capsaicin cream (Chard et al, 2002), anticonvulsants
(Mellegers et al, 2001) and antidepressants (McQuay
et al, 1997) have all been shown to be effective treatments
for chronic pain. Despite the evidence, only
36% of occupational therapists and 60% of physiotherapists
support the use of topical NSAIDs, 27% and
51% respectively support the use of capsaicin cream,
31% and 66% respectively support the use of anticonvulsants,
and 40% and 65% respectively support
the use of antidepressants. These results suggest that a
significant number of physiotherapists and occupational
therapists don’t see a role for these treatment
components in chronic pain, but might also reflect
the possibility that they do not view these treatment
components as within their routine remit. It is interesting
that physiotherapists endorsed the use of these
particular components far more often than their
occupational therapy colleagues, reaching statistical
significance for each component. This trend suggests
that physiotherapists more strongly endorse biomedical
and medication-related treatment components, while
occupational therapists appear to adopt an approach
based on ‘self-management’.
We must acknowledge that all treatments are social
constructs of individual therapists. The decision to use
a particular treatment or not is, to a large degree, based
on historical developments of the individual’s belief in
their efficacy as opposed to any ‘evidence’, particularly
when the evidence is simply not available (lacking).
Decision making regarding treatment selection is governed
by what therapists are taught, what they are told,
what they observe and perhaps what employers expect
them or tell them to do. The high endorsement of
relaxation, for example, may be influenced by factors
such as the technique being taught during training as
an important and beneficial treatment for pain, by
individuals observing it as a commonly administered
treatment during clinical practice, by it being perceived
as a ‘low-risk’, non-invasive treatment that therapists
biomedicalise to justify its use, and by it fitting nicely
within the patient’s perceptions of their needs.
We must also recognise the difficulty in convincing
practitioners that sound, high-quality research findings
cannot be logically or ethically rejected because they
do not fit with their opinions, beliefs or experiences.
This is referred to as the research–practice gap, and
solutions to this dilemma have proposed that practitioners
become more aware of the judgemental
origin of their practice to enable them to more readily
introduce research findings, and that researchers communicate
their research results in a way that makes
them directly relevant to the decision-making process
of practitioners (Alsop, 1997). Although therapists have
embraced the need for evidence in shaping practice,
they are becoming increasingly sceptical of the value of
‘gold standard’ research. Contemporary theorists now
stress that while evidence arises from studying causality
and probability, it also comes from an equally
important examination of patterns and possibilities
(Tickle-Degnen and Bedell, 2003). Large-scale randomised
controlled trials (RCTs) are seen as flawed in their
attempt to identify a pre-specified and invariable
treatment for every patient (that can’t be physiotherapy
surely?). Cox (1999) reminds us that, with respect to
RCTs as best evidence for the therapies, ‘scientific
method focuses on one variable at a time across a
hundred identical animals to extract a single, generalisable
proof ... Clinical practice deals with a hundred
variables at a time within one animal in order to
optimise a mix of outcomes intended to satisfy the
particular animal’s current needs and desires’.
Dealing with a hundred variables at
a time
The World Health Organization’s caution that many
issues in healthcare, such as chronic illness conditions,
require an awareness of the complex interrelationships
between the person, society and the environment (WHO, 2002) is particularly pertinent in this study.
Examining the contextually diverse nature of chronic
pain treatment seems to have served to raise more
questions than it has answered, and this is a strong
indication that our reductionist linear approach using
a questionnaire was ineffective to address such a
complex question. Therapy literature is beginning to
explore these relationships between practice and theory,
and suggests that therapists’ decision making is
multidimensional, and that the evidence base as defined
by RCTs is only one in a wide range of influences.
Physiotherapists and occupational therapists are also
increasingly concerned with patient choice (Rogers,
2002), becoming more aware that the research constituting
the scientific evidence base is not always
defined by outcomes of relevance or importance to
patients (Davies and Nutley, 1999). Upton (1999)
proposes that nurses are slow to take up the evidence
base generated through RCTs because they perceive a
gap between this positivist approach to healthcare and
their professional ethos of holism. She further suggests
that new methods of generating ‘evidence’ need to be
developed before certain practices change. This proposal
seems relevant to therapists, given the strong
integration of patient-centred care within the two
professions. Rappolt (2003) offers an excellent argument
for the need to see evidence as emerging fromthe
interaction between research, professional experience
and the individual client.
The recent BMJ series on complexity and healthcare
has clearly illustrated that health and service provision
can no longer be relegated to simple cause and effect
equations (Fraser and Greenhalgh, 2001; Plsek and
Wilson, 2001; Wilson et al, 2001). Rather, services
must be provided with flexibility and within an
awareness of the dynamic interrelationships of political,
social and cultural environments experienced by
service users. The varied endorsement patterns seen in
this study could be taken as support that therapists are,
either tacitly or overtly, aware of this need to derive the
evidence base for practice from a wider range of
sources than the traditional RCT. The director of the
NHSModernisation Agency, David Fillingham, stated
that ‘the NHS is the epitome of a complex adaptive
system. Such systems do not always respond well to
mechanistic formulae’ (Fillingham, 2002). The Department
of Health (NHS, 2003) report, Achieving Real
Improvement for the Benefit of Patients: NHS Modernisation
Agenda Annual Report 2002/2003, went on to
highlight the importance of shifting the locus of
control to the local level and developing partnerships
between service providers and patients, to ensure
outcomes are relevant within the context of patients’
lives and occupational demands.
Occupational therapists and physiotherapists
have much to offer in promoting healthcare that
encompasses whole people as opposed to randomised participants in a controlled trial. The theory of complex
adaptive systems as it applies to healthcare may be
a significant tool in understanding how service providers
view treatment for chronic pain and in determining
what the evidence base is in relation to the services of
occupational and physiotherapists.
Acknowledgements
The authors wish to acknowledge the study participants
who generously gave of their time, and the
assistance of Professors Jacoby and Baker (University
of Liverpool), and DrMLeitner (InfotechUKResearch).
CONFLICTS OF INTEREST
None.
References
- Alsop A (1997) Evidence-based practice and continuingprofessional development. British Journal of OccupationalTherapy 60:503–7.
- Andersson GB, Lucente T, Davis AM et al (1999) A comparisonof osteopathic spinal manipulation with standardcare for patients with low back pain. New England Journalof Medicine 341:1426–31.
- Barnard S and Wiles R (2001) Evidence-based physiotherapy:physiotherapists’ attitudes and experiences inthe Wessex area. Physiotherapy 87: 115–24.
- Belanger A (1997) There are ‘continuing education alternatives’to ‘alternative continuing education’ in physiotherapy.Physiotherapy Canada 49:249–52.
- Bowling A (1997) Research Methods in Health: investigatinghealth and health services. Buckingham: Open UniversityPress.
- Brown C (2003) Treatment for patients with chronic pain:therapists’ beliefs. British Journal of Therapy and Rehabilitation10:46–52.
- Carroll D and Seers K (1998) Relaxation for the relief ofchronic pain: a systematic review. Advances in Nursing27:476–87.
- Chard J, Lohmander S, Smith C and Scott D (2002)Osteoarthritis. Clinical Evidence 8:1212–37.
- Cox K (1999) Doctor and Patient: exploring critical thinking.Sydney: University of New South Wales Press.
- DaviesHand Nutley S (1999) The rise and rise of evidence inhealth care. Public Money and Management January–March:9–16.
- Dubouloz C, Egan M, Vallerand J and von Zweck C (1999)Occupational therapists’ perception of evidence-basedpractice. Canadian Journal of Occupational Therapy 65:136–43.
- Dunning M (1995) Promoting Action on Clinical Effectiveness.London: King’s Fund.
- Eccleston C, Morley S, Williams A, Yorke L andMastroyannopoulou K (2002) Systematic review of
randomised controlled trials of psychological therapyfor chronic pain in children and adolescents, with a subsetmeta-analysis of pain relief. Pain 99:157–65.
- Elliott AM, Smith BH, Penny KI, Smith WC and ChambersWA (1999) The epidemiology of chronic pain in thecommunity [see comments]. The Lancet 354:1248–52.
- Ernst E (1999a) Homeopathic prophylaxis of headaches andmigraine? A systematic review.Journal of Pain and SymptomManagement 18:353–7.
- Ernst E (1999b) Massage therapy for low back pain: asystematic review. Journal of Pain and Symptom Management17:65–9.
- Ezzo J, Berman B, Hadhazy VA et al (2000) Is acupunctureeffective for the treatment of chronic pain? A systematicreview. Pain 86:217–25.
- Fillingham D (2002) Open space. Take five. Health ServicesJournal 112:27.
- Foster NE, Thompson KA, Baxter GD and Allen JM (1999)Management of nonspecific low back pain by physiotherapistsin Britain and Ireland. A descriptive questionnaireof current clinical practice. Spine 24:1332–42.
- Fraser SW and Greenhalgh T (2001) Coping with complexity:educating for capability. BMJ 323:799–803.
- Frost DP (1997) Medicine, postmodernism, and the end ofcertainty. Complex systems result in a new kind offundamental uncertainty. BMJ 314:1045.
- Funk SG, Champagne MT, Tornquist EM and Wiese RA(1995) Administrators’ views on barriers to researchutilization. Applied Nursing Research 8:44–9.
- Gervais I, Poirier A, van Iterson L, EganMand Tickle-DegenL (2002) Attempting to use a Cochrane Review: experienceof three occupational therapists. American Journal ofOccupational Therapy 56:110–13.
- Gotzsche P (2002) Non-steroidal anti-inflammatory drugs.Clinical Evidence 8:1203–11.
- Green S, Buchbinder R, Glazier R and Forbes A (2000)Interventions for shoulder pain (Cochrane Review). TheCochrane Library, Issue 2. Oxford: Update Software.
- Guzman J, Esmail R, Karjalainen K et al (2001) Multidisciplinaryrehabilitation for chronic low back pain:
systematic review. BMJ 322:1511–16.
- Hadhazy VA, Ezzo J, Creamer P and Berman BM (2000)Mind–body therapies for the treatment of fibromyalgia.A systematic review. Journal of Rheumatology 27:2911–18.
- Halbert J, CrottyMand Cameron ID (2002) Evidence for theoptimal management of acute and chronic phantom pain:a systematic review. Clinical Journal of Pain 18:84–92.
- Henderson H (2002) Acupuncture: evidence for its use inchronic low back pain. British Journal of Nursing 11:1395–403.
- Klaber Moffett JA, Newbronner E, Waddell G, Croucher Kand Spear S (2000) Public perceptions about low backpain and its management: a gap between expectations andreality? Health Expectations 3:161–8.
- Law M and Baum C (1998) Evidence-based occupationaltherapy practice. Canadian Journal of Occupational Therapy65:131–5.
- Maniadakis N and Gray A (2000) The economic burden ofback pain in the UK. Pain 84:95–103.
- Mays N and Pope C (1999) Qualitative Research in HealthCare. London: BMJ Publishing Group.
- Mays N and Pope C (2000) Qualitative research in healthcare. Assessing quality in qualitative research.BMJ320: 50–2.
- McCluskey A (2003) Occupational therapists report a lowlevel of knowledge, skill and involvement in evidencebasedpractice. Australian Occupational Therapy Journal50:3–12.
- McQuay HJ, Moore RA, Eccleston C, Morley S and WilliamsAC (1997) Systematic review of outpatient services forchronic pain control. Health Technology Assessment 1:1–135.
- McQuay HJ, Tramer M, Nye BA et al (1996) A systematicreview of antidepressants in neuropathic pain. Pain 68:217–27.
- Meijers JM, Janssen MA, Cummings GG et al (2006)Assessing the relationships between contextual factors
and research utilization in nursing: systematic literaturereview. Journal of Advanced Nursing 55:622–35.
- Mellegers MA, Furlan AD and Mailis A (2001) Gabapentinfor neuropathic pain: systematic review of controlled anduncontrolled literature. Clinical Journal of Pain 17:284–95.
- Milne S, Welch V, Brosseau L et al (2001) Transcutaneouselectrical nerve stimulation (TENS) for chronic low backpain (Cochrane Review). The Cochrane Library, Issue 2.Oxford: Update Software.
- Mimms J (1996) Research articles and the working therapist(Letter). British Journal of Occupational Therapy 59:394.
- Mior S (2001) Exercise in the treatment of chronic pain.Clinical Journal of Pain 17(4 suppl):S77–85.
- Moore RA, Tramer MR, Carroll D, Wiffen PJ and McQuayHJ (1998) Quantitative systematic review of topicallyapplied non-steroidal anti-inflammatory drugs. BMJ316:333–8.
- Morley S, Eccleston C and Williams A (1999) Systematicreview and meta-analysis of randomized controlled trialsof cognitive behaviour therapy and behaviour therapy forchronic pain in adults, excluding headache. Pain 80:1–13.
- NHS (1997) The New NHS: modern, dependable. London:Department of Health.NHS (2003) Achieving Real Improvement for the Benefit ofPatients: NHS Modernisation Agency Annual Review 2002/2003. London: Department of Health.
- Osiri M, Welch V, Brosseau L et al (2000) Transcutaneouselectrical nerve stimulation for knee osteoarthritis
(Cochrane Review). The Cochrane Library, Issue 4.Oxford: Update Software.
- Pinnington MA (2001) Why are we finding it so hard tochange our approach to low back pain? hysiotherapy
87:58–9.
- Plsek PE and Wilson T (2001) Complexity, leadership, andmanagement in healthcare organisations. BMJ 323:746–9.
- PollockA(2000) Barriers to achieving evidence-based strokerehabilitation. Clinical Rehabilitation 14:611–17.
- Rappolt S (2003) The role of professional expertise inevidence-based occupational therapy. American Journalof Occupational Therapy 57:589–93.
- Rochman DL (1998) Students’ knowledge of pain: a surveyof four schools. Occupational Therapy International 5:140–54.
- Rochman DL and Herbert P (1999) Rehabilitation Professionals’Knowledge and Attitudes Survey Regarding Pain.Boston: Boston School of Occupational Therapy. www.tyofhope.org/prc/html/rehab_professionals.htm
- Rogers WA (2002). Evidence-based medicine in practice:limiting or facilitating patient choice? Health Expectations5: 95–103.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB andRichardson WS (1996) Evidence based medicine: whatit is and what it isn’t. BMJ 312:71–2.
- Scott D, Smith C, Lohmander S and Chard J (2002)Osteoarthritis. Clinical Evidence 8:1212–37.
- Skevington SM (1990) A standardised scale to measurebeliefs about pain control (BPCQ): a preliminary study.Psychology and Health 4:221–32.
- Speed C and Hazleman B (2002) Shoulder pain. ClinicalEvidence 8:1271–89.
- Strong J, Tooth L and Unrah A (1999) Knowledge aboutpain among newly graduated occupational therapists:relevance for curriculum development. Canadian Journalof Occupational Therapy 66:221–8.
- Superio-Cabuslay E, WardMMandLorigKR (1996) Patienteducation interventions in osteoarthritis and rheumatoidarthritis: a meta-analytic comparison with nonsteroidalantiinflammatory drug treatment. Arthritis Care Research9:292–301.
- Thomsen AB, Sorensen J, Sjo¨gren P and Eriksen J (2001)Economic evaluation of multidisciplinary pain managementin chronic pain patients: a qualitative systematicreview. Journal of Pain and Symptom Management 22:688–98.
- Tickle-Degnen L and Bedell G (2003) Heterarchy andhierarchy: a critical appraisal of the ‘levels of evidence’as a tool for clinical decision making. American Journal ofOccupational Therapy 57:234–7.
- Turnquist K and Engel J (1994) Occupational therapists’experience and knowledge of pain in children. Physicaland Occupational Therapy in Pediatrics 14:35–51.
- Unrah A (1995) Teaching student occupational therapistsabout pain: a course evaluation. Canadian Journal ofOccupational Therapy 62:30–6.
- Upton DJ (1999) How can we achieve evidence-basedpractice if we have a theory-practice gap in nursing today?Journal of Advanced Nursing 29:549–55.
- vanTulder M, Malmivaara A, Esmail R and Koes B (2000a)Exercise therapy for low back pain: a systematic reviewwithin the framework of the Cochrane Collaboration backreview group. Spine 25:2784–96.
- vanTulder MW, Ostelo R, Vlaeyen JW et al (2000b)Behavioural treatment for chronic low back pain.
Cochrane Database of Systematic Reviews 2:CD002014.
- van Tulder MW, Ostelo R, Vlaeyen JW et al (2000c)Behavioural treatment for chronic low back pain: a
systematic review within the framework of the CochraneBack Review Group. Spine 25:2688–99.
- vanTulderMandKoes B (2002) Low back pain and sciatica:chronic. Clinical Evidence 7:1032–48.
- Vernon H, McDermaid CS and Hagino C (1999) Systematicreview of randomized clinical trials of complementary/alternative therapies in the treatment of tension-type andcervicogenic headache. Complementary Therapy in Medicine7:142–55.
- White AR and Ernst E (1999) A systematic review ofrandomized controlled trials of acupuncture for neck
pain. Rheumatology 38:143–7.
- Wiffen P, Collins S, McQuay H et al (2000) Anticonvulsantdrugs for acute and chronic pain (Cochrane Review). TheCochrane Library, Issue 3. Oxford: Update Software.
- Wilson T, Holt T and Greenhalgh T (2001) Complexityscience: complexity and clinical care. BMJ 323:685–8.
- World Health Organization (WHO) (2002) Innovative Carefor Chronic Conditions: building blocks for action. Geneva:World Health Organization.