Daoud BE1*, He L2, Miller R1, Chang CLN1 and Meng ML3
1Columbia University Medical Center, Department of Anesthesiology, New York, USA
2Columbia University Medical Center, Department of Obstetrics and Gynecology, New York, USA
3Duke University Medical Center, Department of Anesthesiology, Durham, USA
- Corresponding Author:
- Daoud BE
Columbia University Medical Center
Department of Anesthesiology 622 West 168th Street New York
NY 10032, USA
Tel: 212-342-2028
E-mail: BD2369@columbia.edu
Received Date: March 24, 2020; Accepted Date: May 04, 2020; Published Date: May 08, 2020
Citation: Daoud BE, He L, Miller R, Chang CLN, Meng ML (2020) Anaphylaxis to Cefazolin in the Second Trimester: A Case Report. Gynecol Obstet Case Rep Vol.6 No.2:15 doi:10.36648/2471-8165.6.2.96
Keywords
Anaphylaxis; Second trimester; Pregnancy; Cefazolin; Allergy
Key Highlights
• Anaphylaxis in pregnancy carries a high risk of fetal
morbidity and mortality.
• Immediate management is similar to that of non-pregnant
women.
• Epinephrine is the first line supportive medication.
• A multidisciplinary approach is needed in the maternal
resuscitation.
• There is no allergic cross reactivity between cefazolin and
penicillin.
Introduction
Anaphylaxis is a rare complication during the second trimester of
pregnancy. Like many diseases, pregnancy should not influence
maternal treatment. Most reported cases of anaphylaxis in
pregnancy occur around the time of delivery and fetal heart rate
changes distress secondary to maternal hypotension often results
in emergency delivery. We report the first case of maternal
anaphylaxis occurring in the setting of laser photocoagulation
for twin-twin transfusion syndrome (TTTS), and the third known
case during the second trimester of pregnancy with good
maternal and fetal outcomes [1,2]. This is a case of a woman
with a monochorionic, diamniotic (MCDA) twin gestation in the
second trimester of pregnancy who experienced anaphylaxis due
to cefazolin administration prior to the start of fetoscopic laser surgery for TTTS. The patient provided written consent for the
publication of the case.
Case Report
Our patient is a 37-year-old otherwise healthy, G4P3 at 19 weeks
5 days gestational age with a MCDA twin pregnancy complicated
by TTTS who presented for fetoscopic laser photocoagulation
of pathological placental anastomoses. Baseline maternal heart
rate was 113 beats per minute, blood pressure 90/59 mmHg, and
oxygen saturation 98% on room air. Combined spinal epidural
anesthesia technique was used (intrathecal doses: fentanyl
15mcg and hyperbaric bupivacaine 7.5mg). Cefazolin 2g infusion
was initiated. Five minutes into the infusion (1g of cefazolin
given) the patient experienced itching on the face and hives were
noted. Diphenhydramine 50mg IV was given. Two minutes later,
the patient experienced shortness of breath, with facial edema
and wheezing was appreciated on auscultation. Dexamethasone
10mg IV and epinephrine 10mcg IV were given followed by an infusion of epinephrine 0.5mcg/min. Heart rate remained at
baseline of 120 beats per minute, blood pressure was 105-125/50-
60 mmHg and oxygen saturation remained 98-100% on room air.
Ultrasound assessment of fetal heart rates were adequate but
the donor fetal heart was noted to be hypercontractile with an
irregular rhythm during the first 10 minutes of recognition of the
anaphylactic response and initiation of epinephrine. Vital signs
were observed for 40 minutes after the antibiotic was dosed
and since she remained stable on the epinephrine infusion.
As the laser procedure was urgent, the decision was made to
proceed with the procedure once the patient was stabilized. The
45-minute procedure was uneventful. The hives resolved by the
end of the case.
Post-operatively, epinephrine was decreased to 0.25mcg/min
two hours after antibiotic dosing but the patient experienced
recurrent shortness of breath, so the infusion was resumed
at 0.5mcg/min for 8 more hours. The epinephrine was
then reduced to 0.25mcg/min for another 4 hours. Other
medications administered during recovery included famotidine
20mg IV, nalbuphine 5mg IV, diphenhydramine 50mg IV, and
hydrocortisone 100mg IV. Postoperative tryptase levels were
<2.0 ug/L. Epinephrine was ultimately discontinued, and the
patient was observed overnight before being discharged home in
the morning in stable condition.
Discussion
Anaphylaxis during pregnancy jeopardizes the life of the mother and fetus, as profound hypotension can result in maternal
and fetal hypoperfusion and premature delivery that can be
emergent. This is the first reported case of maternal anaphylaxis
occurring in the setting of laser photocoagulation for twin-twin
transfusion syndrome (TTTS). Anaphylaxis in the second trimester
increases fetal morbidity. This is the third reported cases of
anaphylaxis during the second trimester of pregnancy with good
maternal and fetal outcomes (Tables 1 and 2) [1,2]. Compared
to the general perioperative population in which neuromuscular
blockers are the most common cause of anaphylaxis, antibiotics
are the most common cause of anaphylaxis during pregnancy
[3]. Other less common causes of anaphylaxis during pregnancy
are listed in Tables 1 and 2. This patient was previously exposed
to cefazolin during a laparoscopic cholecystectomy without any
allergic reactions. Re-exposure to an allergen can precipitate
anaphylaxis. This can be worsened in pregnancy with the
postulated mechanism being an increased TH2 response, a
known inducer of IgE synthesis [4].
| Non-Steroidal Anti-Inflammatory Medications |
| Intravenous Vitamins and Iron |
| Neuromuscular Blockers |
| General Anesthetics |
| Latex Products |
| Antiseptic Agents e.g. Chlorhexidine |
Table 1: Causes of anaphylaxis during pregnancy.
| Author |
Agent |
Gestational age at anaphylaxis event (weeks) |
Management |
Maternal Outcome |
Neonatal Outcome |
| Entman et al. (1984) [16] |
Snakebite antivenin |
28 |
Ephinephrine, steroids, isoproterenol, diphenhydramine |
Good |
Neurological damage |
| Luciano et al. (1997) [17] |
Iron |
27 |
Not described |
Good |
Neurological damage |
| Suri et al. (1999) [18] |
Suxamethonium |
23 |
Delivery at 35 weeks |
Good |
Neurologic damage |
| Cole et al. (2000) [19] |
Laminaria |
21 |
Antihistamines, steroids, B-agonists |
Good |
Death (elective abortion) |
| Vercauteren et al. (2003) [1] |
Pentastarch |
28 |
Ephedrine, ranitidine, promethazine, steroids, aminophylline; Cesarean delivery next day |
Good |
Good |
| Biermann et al. (2005) [20] |
Suxamethonium |
26 |
Not described |
Not described |
Not described |
| Berenguer et al. (2013) [15] |
Amoxicillin |
28 |
Fluids, steroids antihistamines
indomethacin, magnesium & pre-term delivery |
Good |
Neurologic damage followed by death day of life 11 |
| Truong et al. (2015)21 |
Suxamethonium |
19 |
Epinephrine |
Good |
Death |
| Tsuzuki et al. (2017) [2] |
Food Allergy (Soba noodles) |
25 |
Fluids, Epinephrine,
Antihistamine, Steroid |
Good |
Good (no neurologic deficiency) |
Table 2: Cases of anaphylaxis reported in second trimester and management and outcome.
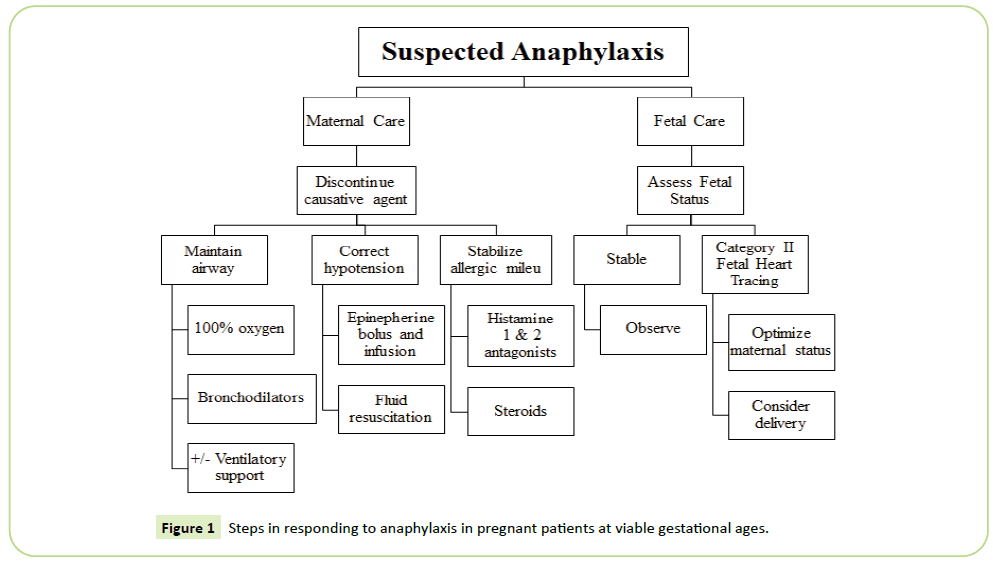
Management of anaphylaxis in pregnant women should be
similar to that of non-pregnant women with a few additional
caveats (Figure 1) [5]. The first step is recognition of anaphylaxis
and cessation of the triggering agent followed by airway and
hemodynamic support, oxygen supplementation and fluid
resuscitation. Anesthesiologists and obstetricians should be
called to assist in the maternal resuscitation. Epinephrine is
the vasopressor of choice in anaphylaxis because it provides
bronchodilation, decreases upper airway mucosal edema, treats hypotension, provides cardiac inotropic as well as chronotropic
support and suppresses further mediator release from mast
cells and basophils [5]. Advanced cardiac life support should be
performed if indicated regardless of pregnancy status. In contrast
to non-pregnant patients, left uterine displacement is required
during resuscitation or the patient should be in left tilt position to
remove aortocaval compression. Endotracheal intubation may be
challenging in the setting of pregnancy due to associated edema
of the upper airway, tongue swelling and obscured landmarks.
Figure 1: Steps in responding to anaphylaxis in pregnant patients at viable gestational ages.
At the time of allergic reaction, the American Academy of Allergy,
Asthma, and Immunology recommends collection of serum
tryptase levels, plasma histamine, 24-hour urinary histamine
metabolites, or urinary prostaglandin to assist in establishing a
diagnosis of anaphylaxis [6]. Tryptase has a 72% sensitivity and
72% specificity, but mast cell tryptase value alone cannot be
used to establish the diagnosis of anaphylaxis [7]. In our case,
the tryptase value was not positive - likely because the blood
sample was not sent to the lab on ice and may not have been
processed properly. For women who report an allergy history,
the American College of Obstetricians and Gynecologists now
supports penicillin allergy skin testing in pregnancy [8].
Appropriate antibiotic prophylaxis against surgical site infection is
imperative. Antibiotic stewardship will help prevent the increased
side effects, poor bacterial coverage, and increased bacterial
resistance to antibiotics due to alternative antibiotic choices.
Suboptimal antibiotic choice due to incompletely investigated or
inappropriately documented or allergies is causing an increase in
maternal infection on a population level. It behooves providers to
delineate true allergies and make plans for testing as necessary
and plan for appropriate second line antibiotics.
The overall prevalence of anaphylactic reaction to cephalosporin
is around 0.1% to 0.0001% [9]. Initial studies of cross reactivity
between penicillin and cephalosporins is suggested to be as
high as 10%, but these studies were performed with early
cephalosporins possibly with trace amounts of penicillin [10,11].
While penicillin and cephalosporin share a beta-lactam ring,
cross reactivity is primarily determined by R1 side chain that is
attached to the beta-lactam ring. There is no cross-reactivity
between penicillin and cefazolin as they do not share similar R side
chains [12]. Therefore, this patient could safely receive penicillin
if needed without skin testing. If this patient were to need a
cesarean delivery, cefazolin could be substituted by another
first-generation cephalosporin with dissimilar R side chains to
cefazolin, preventing cross reactivity while maintaining optimal
surgical site infection prophylaxis [13]. Ceftezole is the only firstgeneration
cephalosporin with similar R side chain to cefazolin
and should therefore be avoid in this patient. Additionally,
gentamycin with clindamycin would also be appropriate
antibiotics for cesarean delivery [14]. Inappropriate alternative
antibiotics are clindamycin only, gentamicin only, vancomycin or
ampicillin only. Clindamycin has poor gram-negative coverage
and can contribute to Clostridium difficile infection. Vancomycin
can cause infusion-related red man syndrome and it has poor
coverage of MSSA. Anesthesiologists play an important role in
allergy assessment and management during the perioperative
period and should be mindful of antibiotic stewardship and
optimal antimicrobial coverage.
The importance of treating allergic reactions with epinephrine and close maternal fetal monitoring is demonstrated by the
adverse outcome in a case of a pregnant woman with anaphylaxis
to amoxicillin in the second trimester. She was treated with
steroids and antihistamines, but not with epinephrine. Days
later she delivered a severely neurologically impaired neonate
who ultimately died [15-21]. Our emphasis on treating with
epinephrine and maintaining maternal blood pressure and preventing maternal hypotension likely assisted in our good fetal
outcome.
Conclusion
Prompt recognition and treatment of anaphylaxis resulted in
complete resolution of anaphylaxis. Although uncommon, when
anaphylaxis occurs during pregnancy prompt recognition and
treatment is required to prevent maternal and fetal morbidity.
References
- Vercauteren MP, Coppejans HC, Sermeus L (2003) Anaphylactoid reaction to hydroxyethylstarch during cesarean delivery in a patient with HELLP syndrome. Anesth Analg 96: 859-861
- Tsuzuki Y, Narita M, Nawa M, Nakagawa U, Wakai T (2017) Management of maternal anaphylaxis in pregnancy: A case report. Acute Med Surg 4: 202-204.
- Chaudhuri K, Gonzales J, Jesurun CA, Ambat MT, Mandal-Chaudhuri S (2008) Anaphylactic shock in pregnancy: A case study and review of the literature. Int J Obstet Anesth 17: 350-357.
- Sheikh J (2007) Intrapartum anaphylaxis to penicillin in a woman with rheumatoid arthritis who had no prior penicillin allergy. Ann Allergy Asthma Immunol 99: 287-289.
- Simons FE, Ardusso LR, Bilo MB (2011) World allergy organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J 4: 13-37.
- Lieberman P, Camargo CA Jr, Bohlke K (2006) Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol 97: 596-602.
- Francis A, Fatovich DM, Arendts G (2018) Serum mast cell tryptase measurements: Sensitivity and specificity for a diagnosis of anaphylaxis in emergency department patients with shock or hypoxaemia. Emerg Med Australas 30: 366-374.
- ACOG Committee (2019) Prevention of Group B Streptococcal Early-Onset Disease in Newborns: ACOG Committee Opinion Summary, Number 782. Obstet Gynecol 134: 206-210.
- Vorobeichik L, Weber EA, Tarshis J (2018) Misconceptions Surrounding Penicillin Allergy: Implications for Anesthesiologists. Anesth Analg 127: 642-649.
- Romano A, Gueant-Rodriguez RM, Viola M (2005) Diagnosing immediate reactions to cephalosporins. Clin Exp Allergy 35: 1234-1242.
- Kelkar PS, Li JT (2001) Cephalosporin allergy. N Engl J Med 345: 804-809.
- Romano A, Gueant-Rodriguez RM, Viola M, Pettinato R, Gueant JL (2004) Cross-reactivity and tolerability of cephalosporins in patients with immediate hypersensitivity to penicillins. Ann Intern Med 141: 16-22.
- Zagursky RJ, Pichichero ME (2018) Cross-reactivity in beta-Lactam Allergy. J Allergy Clin Immunol Pract 6: 72-81 e1.
- Kawakita T, Huang CC, Landy HJ (2018) Choice of Prophylactic Antibiotics and Surgical Site Infections After Cesarean Delivery. Obstet Gynecol 132: 948-955.
- Berenguer A, Couto A, Brites V, Fernandes R (2013) Anaphylaxis in pregnancy: a rare cause of neonatal mortality. BMJ Case Rep.
- Entman SS, Moise KJ (1984) Anaphylaxis in pregnancy. South Med J 77: 402.
- Luciano R, Zuppa AA, Maragliano G, Gallini F, Tortorolo G (1997) Fetal encephalopathy after maternal anaphylaxis: Case report. Biol Neonate 71: 190-193.
- Suri S, Salfield S, Baxter P (1999) Congenital paraplegia following maternal hypotension. Dev Med Child Neurol 41: 273-274.
- Cole DS, Bruck LR (2000) Anaphylaxis after laminaria insertion. Obstet Gynecol 95: 1025.
- Biermann C, Tosin S, Bayoumeu F, Savoye E, Bouaziz H (2005) Anaphylactic shock and uterine atony: must we use sulprostone. Ann Fr Anesth Reanim 24: 69-70.
- Truong HT, Browning RM (2015) Anaphylaxis-induced hyperfibrinolysis in pregnancy. Int J Obstet Anesth 24: 180-184.