Research Article - (2025) Volume 33, Issue 2
Received: 07-Jun-2024, Manuscript No. IPQPC-24-20406; Editor assigned: 11-Jun-2024, Pre QC No. IPQPC-24-20406 (PQ); Reviewed: 25-Jun-2024, QC No. IPQPC-24-20406; Revised: 20-Mar-2025, Manuscript No. IPQPC-24-20406 (R); Published: 27-Mar-2025, DOI: 10.36648/1479-1064.33.2.53
Background: The utilization of healthcare services is low across developing nations. It is very challenging to provide healthcare services to the entire population, regardless of the development. In a given location, access to health care is influenced by various factors, including the availability of health services in the area (supply) and, the population of that location (demand). Therefore, this study identifies the shortfalls of PHCs in the district and its decline in coverage areas according to the variations in altitude as per the norm given by the National Rural Health Mission (NRHM).
Materials and methods: Voronoi map analysis and Euclidean buffer model were used to measure the coverage of the Primary Health Centre (PHC) and its catchment area in both the hilly districts of Uttarakhand i.e., Rudraprayag and Chamoli.
Results: Though Uttarakhand has achieved 85% institutional delivery, it is way behind the target set by the National Population Policy 2000 to achieve 100% institutional delivery by 2010 in India. An apparent disparity in the coverage of healthcare services is observed. In some pockets of the Chamoli district, the population pressure on PHCs was as high as 50000 populations per PHC which is definitely due to the shortfall of PHCs.
Conclusions: Uttarakhand's healthcare coverage is low despite achieving 85% of institutional delivery. Population pressure on Primary Health Centres (PHCs) is high in Chamoli, causing a shortfall. Based on the terrain and elevation of the region, a dynamic population threshold for setting up PHCs, focusing mainly on coverage should be adopted. The findings of the study will be helpful for the government stakeholders, and policymakers in developing infrastructures to improve coverage and identification of optimal locations as well as population for setting up more PHCs.
Drug-drug interactions; Knowledge; Medication; Pharmacy professionals
India's public health services are developing. Furthermore, the regional disparities in the distribution of health facilities are enormous. Regardless of the level of development, human health is an essential element for the sustainable development of society. Like other developing countries, India faces challenges in providing adequate health services and ensuring optimal access to them across the population. Many health facilities and Primary Health Centres (PHCs) are underutilized because they provide poor services, are difficult to access, and are unprepared for critical emergency services [1].
The population is considered to be very dynamic in terms of spatial arrangement and distribution as well as cultural and behavioral characteristics. Therefore, access to health services can be expressed as the ability of people to use health services when they need them, and access to health services is related to supply variables such as population pressure and distance from centers [1-5].
Rapid access to primary care can avoid additional health service costs because travel time is the simplest measure of access when public transportation is available. Keeping these realities in mind, the National Rural Health Mission (NRHM), under the 12th Plan of the Planning Commission of India, aims to provide high-quality healthcare to people from rural areas, especially groups in remote and most disadvantaged areas.
The majority of India's rural population belongs to the economically weaker group and it is difficult for them to afford private healthcare services. Therefore, most people in rural areas go to primary health facilities to meet their health needs. The use of GIS has allowed researchers to use a diversity of methodological options to measure accessibility. In India, despite economic development, morbidity in infants and mothers is still a major concern. India's rural health infrastructure is designed as a three-tiered system: Sub Centres (HCs), Primary Health Centres (PHCs), and Community Health Centres (CHCs) (Ministry of Health and Family Welfare, 2012). Sub-Centre (SC) is the most peripheral unit constrained by minimal medical facilities and hence people tend to turn to PHCs.
Facility-based childbirth is an essential intervention to reduce preventable childbirth-related maternal and child mortality. From 1990 to 2015, more than 10 million women died worldwide from complications related to pregnancy or childbirth [2]. Globally, 2.6 million new-borns died in 2016, or about 7,000 every day, and most (99%) of these preventable deaths occurred in low-income and Low-Middle-Income Countries (LMIC) [3]. Pregnancy-related complications that can lead to maternal death may occur during or shortly after birth.
In LMICs, direct obstetric complications during childbirth are responsible for 70% of maternal deaths. Timely access to facility births has saved the lives of many mothers and newborns. In high-income countries, maternal mortality could be further reduced through increasing birth rates in health facilities. Low utilization of the organization's service offerings in many Low and Middle-Income Countries (LMICs) may be due to cultural concerns and geographic constraints that prevent women from accessing the services. As a result, women are more likely to give birth at home [6-10].
To ensure equitable and accessible institutional service delivery, identifying vulnerable groups and populations within countries is critical so that interventions can be developed and implemented, personalized intervention (Table 1).
| Districts | Place of delivery | |
| Non-Institutional | Institutional | |
| Dehradun | 3.44 | 96.56 |
| Almora | 8.24 | 91.76 |
| Uttarkashi | 11.15 | 88.85 |
| Rudraprayag | 11.41 | 88.59 |
| Tehri garhwal | 11.45 | 88.55 |
| Pithoragarh | 11.65 | 88.35 |
| Udham Singh nagar | 12.07 | 87.93 |
| Garhwal | 16.03 | 83.97 |
| Nainital | 17.38 | 82.62 |
| Champawat | 17.58 | 82.42 |
| Bageshwar | 17.66 | 82.34 |
| Haridwar | 28.29 | 71.71 |
| Chamoli | 29.03 | 70.97 |
| Total | 15.48 | 84.52 |
Table 1: Data regarding place of delivery according to national health and family survey 5 (2019-21).
However, we can figure out from the NFHS 5 data that Chamoli witnessed one of the lowest institutional delivery in Uttarakhand while Rudraprayag performed better although being a neighboring district and hilly in terrain. If compared with NFHS-4 data regarding Institutional delivery the dependency on private facilities has decreased significantly in both districts but a higher difference is seen in the Rudraprayag district. Both districts share a similar proportion of deliveries held in private institutions (Table 2).
|
|
NFHS-5 |
NFHS-4 |
||||||
|
Non-Institutional |
Institutional |
Public |
Private |
Non-Institutional |
Institutional |
Public |
Private |
|
|
Chamoli |
29.03 |
70.97 |
97.43 |
2.57 |
46.7 |
53.3 |
92.73 |
6.71 |
|
Rudraprayag |
11.41 |
88.59 |
97.03 |
2.97 |
33.49 |
66.51 |
89.88 |
10.12 |
Table 2: Data regarding place of delivery according to NFHS 4 and 5 focusing on the deliveries held in public and private facilities.
Earlier Studies in Healthcare Coverage and Mapping
In the Indian context, there is very little literature on this subject, despite its importance for human resources development. However, studies on healthcare equity in Low and Middle-Income Countries (LMICs) are reviewed below. According to recent data, some of these countries have improved access to health care to reduce disparities in healthcare use. Due to the expansion of primary health care and insurance coverage, disparities in the use of inpatient and outpatient care have decreased significantly in China in recent years [5].
Another example of a country whose health system has improved equity is Chile, where the implementation of a “health guarantee” strategy has ensured people's access to health care for most diseases. Although the use of hospital care was more concentrated in the affluent countries between 2001 and 2005, Thailand was the first non-OECD country to adopt Universal Health Coverage (UHC) and also saw a significant reduction in disparities in outpatient care utilization [10-15].
However, some countries still lag in achieving equality in health service utilization noting the virtual universal health coverage, the Philippines has seen increasing disparities in health service utilization between 1998 and 2007.
Furthermore, observed that although the burden of disease is higher for people whose income is low, the distribution of health benefits favors the rich in South Africa, Ghana, and Tanzania. India is no different. [15-20].
Study Area
The districts were selected with consideration for accessibility and spatial position, as both of them encompass a wide range of spatial characteristics, from densely populated areas to sparsely populated areas. The area features highly dispersed plateaus and hills due to the offshoots of hilly tracts covered in vegetation, as well as rugged and undulating terrain. A district in the Indian state of Uttarakhand is called Chamoli. The region is bordered to the north by Tibet, to the east by the districts of Pithoragarh and Bageshwar in Uttarakhand, to the south by Almora, to the southwest by Pauri Garhwal, to the west by Rudraprayag, and the northwest by Uttarkashi. Gopeshwar is home to the Chamoli district's administrative center. The district occupies an area of approximately 7,520 km³ (2,900 sq mi). 49 people are living in the district per square kilometer (130/sq mi). Between 2001 and 2011, its population increased at a pace of 5.6%. Chamoli has an 83.48% literacy rate and a sex ratio of 1021 females for every 1000 males. The populations of Scheduled Castes and Scheduled Tribes are 20.25% and 3.13%, respectively.
In the Indian state of Uttarakhand, the Rudraprayag district includes the cities and municipalities of Rudraprayag. Rudraprayag is the site where the Alaknanda and Mandakini rivers converge, one of the Panch Prayag (five confluences) of the Alaknanda River. Rudraprayag is situated 86 miles away from Kedarnath, a sacred Hindu city. It is 895 meters (2936 feet) above sea level on average. The population of Rudraprayag district is 242,285 (almost equivalent to the population of Vanuatu), according to the 2011 census. As a result, it is ranked 583rd out of 640 in India. 119 people are living in the district per square kilometer (310/sq mi). Between 2001 and 2011, the population growth rate was 4.14%. According to the 2011 census, Rudraprayag has the sixthhighest sex ratio in the nation, with 1120 girls for every 1000 males; the only place higher is Almora, which is also in Uttarakhand. Its literacy rate is 82.09%. The proportions of Scheduled Castes and Scheduled Tribes to the total population are 19.68% and 0.16%, respectively.
Data and Methods
This study used Institutional delivery data from the National Family and Health Survey-5 (2019-2021). It is conducted under the stewardship of the Ministry of Health and Family Welfare, Government of India. It proves a wide range of information on NFHS is a large-scale multi-round survey providing comprehensive information on population, health, and nutrition across India and each state/Union Territory (UT). The recent round, i.e., NFHS-5, the survey successfully interviewed 2,843,917 household members from 636,699 households, among which 724,115 women aged 15–49 years and 101,839 men aged 15-54 years, along with other age group people, using a multistage stratified sampling design. Detailed information on study design, sample, collection, and available findings are in the national report [7].
The health system is organized into primary, secondary, and tertiary levels. At the primary level, there are sub-centers and Primary Health Centers (PHCs). At the secondary level, there are Community Health Centers (CHCs) and smaller district hospitals. Finally, the highest level of public care provided by the government is the university level, which includes medical schools and general/district hospitals [8].
Primary health centers exist in more developed rural areas with populations of 30,000 or more (20,000 in remote areas) and serve as larger medical clinics staffed with doctors and medical staff. Patients may be referred from local sub-centers to the PHC for more complex cases. The big difference with sub-centers is that the state government funds the PHC and not the national government. PHC also functions to improve health education by placing more emphasis on preventive measures [9]. The information layers such as the road network have been digitised using the settlement Commissionerate and land record map from the Government of Uttarakhand.
Further, the Village level administrative boundary was digitized from the Chamoli and Rudraprayag district census map, Census of India 2011 and 17 PHC locations were marked referring to the Department of Medical Health and Family Welfare. The population of villages was computed from the village directory, census 2011. The Voronoi map analysis along with Euclidean Buffer analysis has been carried out in Arc GIS 10.4.
Analysis
With the help of Voronoi maps of the midpoints between neighboring PHCs, we have created the boundaries of these Voronoi cells. These boundaries form line segments and coverage areas of the health centers are prepared by taking the weighted mean of the points.
Primary Health Centre to population ratio (R):
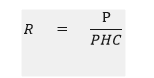
P=Population of the area
PHC=Primary Health Centre
Voronoi Map Analysis
A Voronoi diagram is a mathematical construct that partitions a plane into regions based on a given set of objects. These objects, often called seeds, sites, or generators, can be points in the plane. Each seed corresponds to a region known as a Voronoi cell, which consists of all points closer to that seed than to any other. The Voronoi diagram is dual to the Delaunay triangulation of the same set of points.
Construction: Given a finite set of points in the Euclidean plane, each site defines a Voronoi cell consisting of all points closer to that site than to any other. The boundaries of these cells are line segments, rays, or lines where neighboring cells meet. The vertices of the diagram represent points equidistant to three or more sites. Voronoi diagrams, also known as Thiessen polygons, are used to analyze spatially distributed data.
Geodesic Buffer Analysis
In the realm of Geographic Information Systems (GIS) and spatial analysis, buffer analysis involves determining a zone around a geographic feature that contains locations within a specified distance of that feature. This zone is commonly referred to as the buffer zone or simply buffer. Buffer zones are created around specific features (such as points, lines, or polygons) to represent areas of influence or proximity. These account for the shape of the Earth (an ellipsoid or geoid). Distances are calculated on the curved surface of the Earth. Geodesic buffers are appropriate when input features are dispersed (covering multiple UTM zones, large regions, or the entire globe).
The pursuit of equity in health and healthcare is a key element of health policy in India, with a commitment to improving access to quality healthcare for the poor and Disadvantaged people. This has been reiterated in almost all health-related policy documents, from the 'Bhore Commission' of 1946 to the latest 'Universal Health Care Bill' of 2009. Health systems in the majority of Indian states strive to remove barriers to healthcare utilization and work toward achieving equitable, routine access to health care, understood as people having equal needs for medical care and receiving equivalent treatment, regardless of their situation income, or socioeconomic status.
To achieve this goal, it is imperative to systematically assess current inequities in health service utilization, thereby identifying policy intervention points that can reduce these disparities in inequality in access to health care services. This task has so far not received serious attention from scholars and policymakers (Figure 1).
The Framework of the Study
Figure 1: Framework followed to relate institutional deliveries with PHC coverage area.
The framework utilized in the study is as follows: Accessibility, affordability, availability, appropriateness, and adequacy are the five main pillars of healthcare facilities, and they are generally impacted by accessibility and coverage, which includes the availability of PHCs and population pressure. Primary health centers offer a range of services, including treatment, preventive care, and emergency care. Emergency care includes care for unintentional injuries as well as difficulties related to mother and child health, including birth complications and newborn care. Institutional deliveries are among the most significant indicators of emergency care.
Although Chamoli district has eight PHCs, it is mostly overburdened as the PHC/population ratio is 2.5 times greater than the needed number of PHCs. Seventy percent of deliveries in the district took place in health institutions, while thirty percent did not take place in such settings. Additionally, it is discovered that a PHC's typical catchment area ranges from 20 to 25 square kilometers, which is a sizable amount for a hilly region with an average elevation of 3472 meters. Rudraprayag is doing better than Chamoli when it comes to conducting institutional deliveries. Chamoli is the state with the lowest performance. It is widely accepted that plain locations perform better in terms of Place of Delivery (PoD) indicators since they are easier to access. The place of delivery is a crucial metric for evaluating the state of the healthcare infrastructure. The NFHS 5 data for both districts shows that less than 3% of deliveries take place in private institutions, with the remaining 97% occurring in public institutions. This suggests that the public prefers public health facilities, indicating that the demand side is well-maintained, while the supply side is questionable, with almost every PHC having a burden that is 2.5 times higher than the average population threshold.
Despite having five PHCs and a similar PHC/population ratio, Rudraprayag district is doing slightly better than Chamoli district, where 88% of deliveries were institutional deliveries. The districts share nearly identical topography, except for the PHC's 10–13 sq. km. catchment area and 895 m average elevation above mean sea level (Figure 2).
Primary Health Centre Coverage Area
Figure 2: Map of Rudraprayag and Chamoli district with PHC locations, village boundaries, and coverage areas.
In the following paper, we have attempted to map the PHCs' coverage areas using the Theissen Polygon method, assigning equal weights to each PHC. As a result, the maps show that, as we approach the northern regions of both districts, the elevation gradually rises and the population becomes more dispersed, increasing the distance in time between the PHCs. Although Chamoli is a larger district than Rudraprayag and has a larger population, there are more PHCs in Chamoli due to this factor, yet the population pressure is the same in both districts (Figure 3).
Primary Health Centre Coverage Area with Population Pressure
Figure 3: Map of Rudraprayag and Chamoli district with Population pressure on particular PHCs according to their coverage areas.
From the following table, we can figure out the population pressure on the PHCs in both districts the range of variations in population pressure per PHC varies between 14768 to 106941 in Rudraprayag district whereas Chamoli district has a smaller range of population pressure ranging from 34411 to 58387 population per PHC. Although the average population pressure remains somewhat similar to 50000 (Figure 4).
Village-wise Population Distribution along with Road Network
Figure 4: Map showing village-wise population distribution in Chamoli and Rudraprayag district Census 2011.
Here the village boundaries of both districts were plotted according to the Survey of India`s demarcation of village boundaries which is integrated with the population data from the Census of India 2011, then the various sizes of villages along with their population are plotted with circles according to the size of the population (Figure 5).
Village-wise Population Distribution along with PHC and its Catchment Area
Figure 5: Map showing village-wise population distribution in Chamoli and Rudraprayag district Census 2011 and its dependence on particular PHCs.
Both the village-wise Population data are plotted along with the demarcated areas of the PHC which makes it better to assess the dependence of villages and their population on particular PHCs. Among the total number of 13 PHCs, it was found that 8 PHCs are mostly over-burdened as the PHC/ Population ratio is almost 2.5 times higher than the required no of PHCs (i.e., 1 PHC per 20000 populations in hilly areas) (Figure 6).
Primary Health Centre Coverage Area with Road Network
Figure 6: Map showing PHC-wise coverage areas in Chamoli and Rudraprayag district.
The coverage areas of the PHCs are shown in terms of Euclidean buffer zones showing areas within a radius of 5, 10, and 15 km respectively along with their functional coverage areas. Also, the road network is also demarcated and the time distance is calculated, with this technique, we have calculated the time distance according to the buffer areas i.e., the first circle is within 20-25 minutes of travel time then 55-60 minutes, and more than 100 minutes in the 3rd buffer zones (Figure 7).
Primary Health Centre Coverage area with Population Size
Figure 7: Map showing PHC wise coverage areas in Chamoli and Rudraprayag districts along with the village-wise population data.
We can compare both the maps directly and distinguish the difference in coverage areas. In Chamoli district, 23% of the population lives away from a 15 km radius of any PHC, whereas in Rudraprayag only 2% population which is a very contrasting result as almost both the districts have the same Population-PHC ratio and hence the difference in the outcomes in terms of healthcare utilization can be justified. As we move towards higher altitudes the mobility and road network become difficult which leads to longer travel time.
This study contributes to the broader literature linking environment and population health and to the literature on environmental effects on healthcare services coverage and accessibility in particular. Though Chamoli's average elevation is higher than Rudraprayag's, both districts are situated in similar latitudinal zones. The average population-PHC ratio of both districts is approximately 50,000 per PHC, which is 2.5 times higher than the NRHM norms for hilly areas, that is 20,000 population per PHC. In the Chamoli District, 77% of the population lives within a 15 kilometer radius of any PHC, compared to 98% of the total population in Rudraprayag. These results converge with other studies conducted in similar rural and remote areas. Coverage for childbirth and hospital care is too low and is even lower than in the African region. In a study conducted in sub-Saharan Africa, it was found that only 7 out of 48 countries in sub-Saharan Africa had less than 50% of the population located within 2 hours of drive from a public emergency care hospital. The vast network of public health centers that currently exists is far from meeting the government's guidelines and covering the necessary population. In the absence of public primary health care services, many people either forego receiving any medical care at all and use it too little too late or opt to seek costly and unregulated care in the private sector. This is because the poor make up the majority of users of primary healthcare facilities, while the rich prefer to use private clinics and hospitals. Since independence, India's primary healthcare system has developed, and the country now boasts an intricate network of almost 200,000 Government Primary Health Care Facilities (GPHCFs), both in urban and rural areas. The limited range of services provided by the current GPHCFs is caused by several factors, including occasionally the unavailability of providers. Thus, in 2013–14, just 11.5% of rural and 3.9% of urban individuals in need of health services in India used the GPHCFs, which are severely underutilized aside from mother and child health services.
Because of the higher elevation and longer travel times, the population of the Chamoli district is more spread. The issue highlighted in this paper is almost applicable to all the hill districts of India where still majority of the population is not utilizing the health care facilities set up by the government.
The main limitation of the study is that it was not able to take the doctor availability and doctor-to-population ratio due to the data constraint, otherwise, it would have given us a clear picture of the demand for the services at ground level.
Although ambulance availability and doctor-to-patient ratio are not considered in the paper it would have been more efficient in figuring out the imbalance and figuring out the core issues from the supply side. Therefore, to serve the entire population, the government should create a dynamic PHC allocation system based on altitude. As elevation rises, the minimal threshold needed to build a PHC should decrease, as the population disperses more widely.
This study was conceptualized by GV and NAK. The analysis and interpretation of the results were carried out by NAK. The paper's initial draft was written by NAK. GV wrote part of the paper and reviewed and revised it. The final manuscript was read and approved by all authors.
No specific funding from any public, private, or nonprofit organization was given for this research.
All the data is available in the public domain at https:// dhsprogram.com/data/ dataset/India_Standard-DHS_2020.cfm? flag=0. The census of India population data is taken from https:// censusindia.gov.in/census.website/data/census-tables.
The location of primary health centres was taken from health facility maps: Department of medical health and family welfare, Government of Uttarakhand, India (uk.gov.in).
The study's data came from sources that are in the public domain. Therefore, getting ethical approval for this study was not required. The Demographic Health Survey (DHS) series includes NFHS-5. The ICF IRB and frequently the IRB of the host nation have examined and approved the protocols and questionnaires for standard DUS investigations. While the host country IRB makes sure the investigation complies with local laws and standards, the ICF IRB makes sure it complies with U.S. Department of health and human services regulations on human protection (45 CFR 46). In a similar vein, the Indian government makes the data from the census available to the general public. Throughout the investigation, written informed consent was obtained from each participant.
None.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Kalita NA, Vasishtha G. (2025) Analysis of Variations in Coverage of Primary Health Centre: A Comparative Study Based on Chamoli and Rudraprayag Districts. Qual Prim Care. 33:53.
Copyright: © 2025 Kalita NA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.