Research Paper - (2010) Volume 18, Issue 4
1Assistant Professor, Department of Family Medicine, Medical University of South Carolina, Charleston, USA
2President, Delaware Valley Outcomes Research, Newark, Delaware, USA and Associate Professor, Department of Family and Community Medicine, Thomas Jefferson University, Philadelphia, Pennsylvania, USA
3Professor and Director of Research, Department of Family Medicine, Medical University of South Carolina, Charleston, USA
4Research Associate, Department of Family Medicine, Medical University of South Carolina, Charleston, USA
5Assistant Professor, Department of Family and Community Medicine, University of Missouri, Columbia, USA
6Research Professor, Department of Family and Community Medicine, Thomas Jefferson University, Philadelphia, Pennsylvania, USA
7Director, Medical Quality Improvement Consortium, GE Healthcare
8Data Manager and Statistical Analyst, Delaware Valley Outcomes Research, Newark, Delaware, USA
Received date: 22 December 2009; Accepted date: 25 May 2010
BackgroundGastro-esophageal reflux disease (GERD) is common in primary care but is often underdiagnosed and untreated. GERD can also present with atypical symptoms like chronic cough and asthma, and physicians may be unaware of this presentation. We aimed to implement and evaluate an intervention to improve diagnosis and treatment for GERD and atypical GERD in primary care.MethodThis was a randomised controlled trial in primary care office practice using a national network of US practices (the Medical Quality Improvement Consortium – MQIC) that share the same electronic medical record (EMR). Thirteen offices with 53 providers were randomised to the intervention of EMRbased prompts and education, and 14 offices with 66 providers were randomised to the control group totalling over 67 000 patients and examining outcomes of GERD diagnosis and appropriate treatment. Results Among patients who did not haveGERDat baseline, new diagnoses of GERD increased significantly in the intervention group (3.1%) versus the control group (2.3%) (P0.01). This remained significant after controlling for clustering with an odds of diagnosis of 1.33 (95% CI 1.13–1.56) for the intervention group. For patients with atypical symptoms, those in the intervention group had both higher odds of being diagnosed with GERD (OR 2.02, 95% CI 1.41–2.88) and of being treated for GERD (OR 1.40, 95% CI 1.08–1.83) than those in the control group. ConclusionsGERD diagnosis and treatment in primary care, particularly among patients with atypical symptoms, can be improved through the use of an EMR-based tool incorporating decision support and education. However, significant room for improvement exists in use of appropriate treatment.
atypical symptoms, electronic medical record, gastro-esophageal reflux disease
How this fits in with quality in primary care
What do we know?
Gastro-esophageal reflux disease (GERD) is a common problem with classic symptoms in primary care settings. Although many patients self-treat, atypical symptoms such as asthma, laryngitis, and chronic cough are known to be related to GERD as well. Patients and providers may not recognise these atypical symptoms and thus, some patients remain under-diagnosed and improperly treated.
What does this paper add?
This paper demonstrates that improvements in disease management including education about, as well as diagnosis and treatment of certain medical problems can be achieved in primary care settings using interventions based within the daily use of an electronic medical record (EMR) system. The improvements in diagnosis and treatment of GERD, particularly for those patients with atypical symptoms is encouraging and provides insights into quality improvement strategies for the management of other conditions using EMRbased methods
Gastro-esophogeal reflux disease (GERD) is a common problem in the USA with over 40% of adults reporting monthly heartburn symptoms and 14% with weekly symptoms.[1] Patients often present to primary care physicians when symptoms do not resolve or diagnosis is uncertain. Although diagnosis would appear to be straightforward, diagnosis and treatment are made particularly complicated when patients present with atypical symptoms.
It is of interest that GERD may not present with typical symptoms like heartburn. Atypical symptoms include asthma, laryngitis and chronic cough. Research shows that GERD is commonly associated with asthma. A study by Kiljander et al showed that a third of asthmatics had reflux on pH monitoring.[2] Classic symptoms ofGERDhave been shown to be absent in 40% to 60% of patients with asthma.[3] When treatment of symptoms such as chronic cough or laryngitis does not help,GERDandGERDtreatment should be considered. Because of these atypical symptoms, however, GERD may be under-diagnosed in these patients.
One promising approach to improving care in clinical practice is through information technology such as EMRs. An EMR can make guidelines and education available to physicians and provide clinical decision support at the point of care. The purpose of this study was to examine the impact of augmented, provider-coordinated care executed via an EMR for the diagnosis and treatment of classical symptom GERD and atypical symptom GERD.
Setting and population
This randomised controlled study was conducted within the MedicalQuality Improvement Consortium (MQIC), a national network of outpatient offices all of which use the Centricity1EMR. At the time the study began, MQIC included approximately 5000 providers (approximately two-thirds of them primary care) from 34 states and the District of Columbia, practicing in a wide range of settings including private solo practices as well as single- and multi-specialty group practices. EMR data from MQIC members are deidentified at the practice site and then aggregated centrally. At the initiation of the study, the MQIC database contained information for 6.3 million patients. MQIC has been used for previous studies examining quality of care.[4,5]
Participating offices were recruited from MQIC offices that had been using the Centricity Office EMR for at least one year. Inclusion criteria included being physicians or mid-level providers (nurse practitioners or physician assistants) in adult primary care practice (general internal medicine, family medicine or general practice) for at least eight hours per week. Twenty-seven offices were randomised to the intervention or control group. The unit of randomisation was the provider office. We employed a block randomisation scheme that takes into account the type and size of practices; 13 offices with 53 providers were randomised to the intervention group, and 14 offices with 66 providers were randomised to the control group. Practice size varied from one to 16 providers in the intervention group, with a median of two providers and a mean of five providers. In the control group, practices ranged from one to 13 providers, with median of three and a mean of five providers in each practice.
Patients with diagnosed GERD were identified using the EMR. GERD patients were defined as patients with ICD-9 codes corresponding to diagnoses of oesophageal reflux 530.81, and to oesophagitis 530.1x (includes oesophagitis unspecified 530.10, reflux oesophagitis 530.11 and other oesophagitis 530.19). Patients with potential atypical symptoms of GERD included those with uncontrolled asthma, chronic cough, hoarseness and chronic laryngitis. Uncontrolled asthma was defined as asthma plus current use of a controller medication. A diagnosis of asthma was defined according to the ICD-9 code 493.xx. We identified chronic cough, hoarseness and chronic laryngitis through the EMR using the ICD-9 codes 786.2, 784.49 and 476.1, respectively. Chronic cough was defined as cough for longer than eight weeks.[6,7] The ICD-9 code 786.2 does not distinguish cough from chronic cough. Therefore, chronic cough was defined as the presence of this diagnosis code and its presence on the problem list for more than eight weeks.
Intervention
The main intervention was an encounter form that was embedded into the EMR. The form provided tools to assist in management of two gastroenterologic conditions: GERD and symptoms that may indicate an atypical presentation of GERD. These tools were based on nationally recognised guidelines for the disease states being studied. For GERD, we used the 2005 Guidelines for the Diagnosis and Treatment of Gastroesophageal Reflux Disease, by the American College of Gastroenterology.[8]
The algorithms and prompted care were tailored according to the disease/problem state of the patient. The prompts were developed by the physician investigators independently based on established GERD diagnosis and treatment guidelines from the American College of Gastroenterology. One group was persons diagnosed with GERD (including both those on and not on GERD medications). A second group included personswith symptoms suggestive ofGERD(e.g. asthma or chronic cough) who are not diagnosed with GERD. These patient groups were automatically identified by data in the EMR. For each group, a tailored set of recommendations was triggered and provided to the clinician, based on guidelines andEMRdata. For those with no diagnosis of GERD, but with symptoms suggestive of GERD, the clinician was prompted to consider a diagnosis of GERD. For example, for patients with diagnosed GERD, the first page of the EMR form stated that the patient has a diagnosis of GERD and allowed the provider to ask further questions about symptoms and treatment. Likewise, for patients with atypical symptoms of GERD, the first page of the form alerted the provider that the patient had a diagnosis, such as laryngitis, that might suggest an atypical presentation of GERD. In either case the provider could then move to a second page of the form in which more detailed questions could be asked to clarify symptoms. These questions included symptomatic information (pain behind breastbone, acid taste in mouth and burning in upper stomach), frequency of symptoms and timing of symptoms, such as symptoms at night.
The third page of the EMR form included access to prescribing a new GERD medication from an alphabetical listing of all available proton pump inhibitor (PPI) and histamine 2 receptor antagonists (H2RA – H2-blocker medications) by generic name and/or adding a diagnosis of GERD if the provider decided this was appropriate. The form also allowed documentation of alarm symptoms such as weight loss and dysphagia. In addition, this form included both patient and provider education about GERD, GERD treatment and atypical symptoms of GERD. The handouts had educational material for the patient which included a link to an interactive educational website.
Additional education to the intervention providers included clinical education for study providers and their clinical staff regarding guidelines for the two disease states. This education was provided in two ways. First, there was education prior to the implementation of the EMR-based tools. Each provider in the study arm was provided with a packet that included print materials as well as instructions for accessing an educational module on the web. Other clinical staff who worked in the office of the study providers were also provided with a similar preintervention training packet.
The secondmethod of provider/staff education was through ‘point of care learning’. Providers were able to access educational materials directly from the EMR tool interventions. Participating providers were alerted to available educational materials at the conclusion of a specific patient encounter and invited to participate via a custom education website. The education modules were delivered in a case-based format of short duration.
Outcomes and analysis
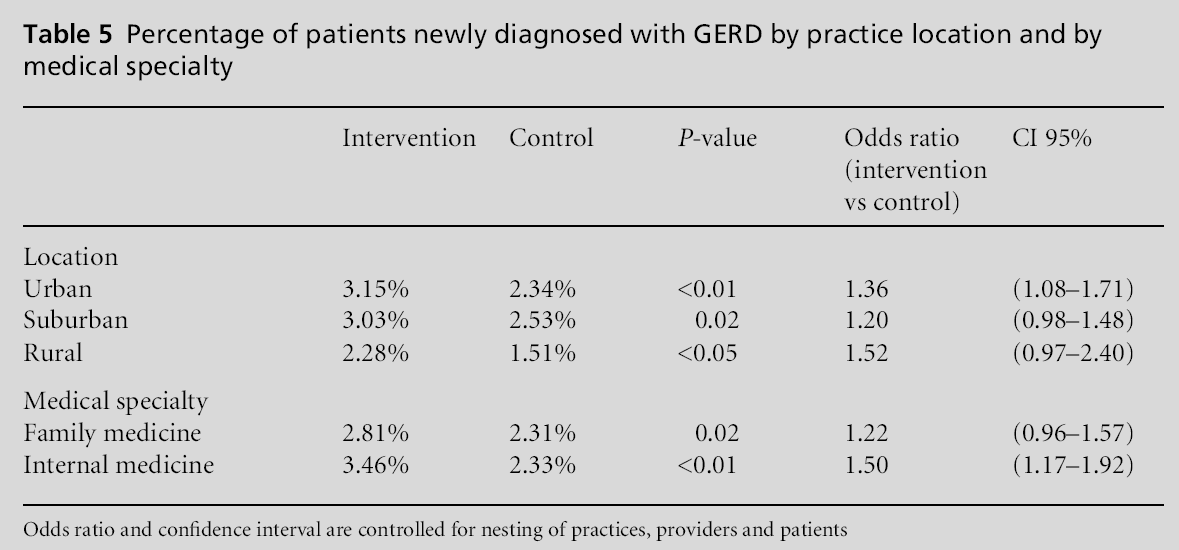
The main outcomes were diagnosis of GERD, diagnosis of GERD for those with atypical symptoms and prescriptions for GERD medications among individuals with GERD. GERD medications were defined as both the PPIs andH2RAs. The outcome was defined as proportion of GERD patients using PPI and H2RA medications. Use of medications for GERD was defined as at least one prescription for medication during the period of observation. In addition to determining the overall percentage of patients newly diagnosed with GERD, we performed a stratified analysis stratifying by practice location (urban, suburban and rural) and by the most prevalent medical specialties (family medicine and internal medicine).
A second outcome was diagnosis of GERD in persons with atypical symptoms of GERD or diseases that can be triggered by GERD (e.g. asthma), who are not already diagnosed with GERD. These patients had had atypical symptoms of GERD during the baseline year prior to the beginning of the year-long study period, or atypical GERD symptoms during the study period, and had not been on GERD medications during the baseline year. The outcome was defined as proportion of patients with these conditions who are diagnosed with GERD during the study period. And finally there was the outcome use of GERD medications in persons with atypical GERD who do not have a diagnosis of GERD. GERD medications were again medications in the PPI and H2RA classes. The outcome was defined as proportion of patients with atypical GERD symptoms who had not been diagnosed with GERD, but were using PPI and H2RA medications. Use of medications for GERD was defined as at least one prescription for medication during the period of observation. The outcome was defined as persons who had symptoms who were taking medication.
The primary analysis compared these three outcomes for the intervention and control groups using the Chi-square test with P<0.05 as the cut-off for statistical significance. Logistic regressions and determination of odds ratios and 95% confidence intervals were performed for each outcome, accounting for nesting (or clustering) of patients within providers and nesting of providers within practices in the design. We controlled for two levels of clustering: the physician level and the practice level, since patients are not independent of these.
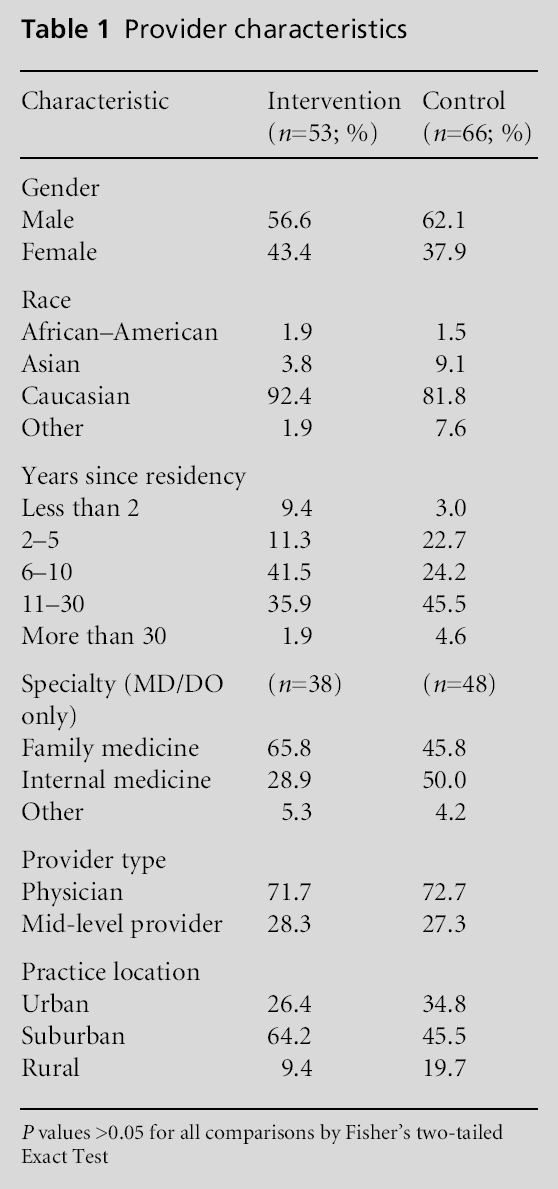
Table 1 shows the characteristics of the providers in the study. The providers were predominantly physicians with more than five years of practice experience, and were mostly male and Caucasian. The intervention offices were somewhat more likely to be in suburban locations and their physicians were somewhat more likely to be in family medicine, but these differences were not statistically significant. At the start of the study there were 30 448 active adult patients in the intervention group and 37 095 in the control group.
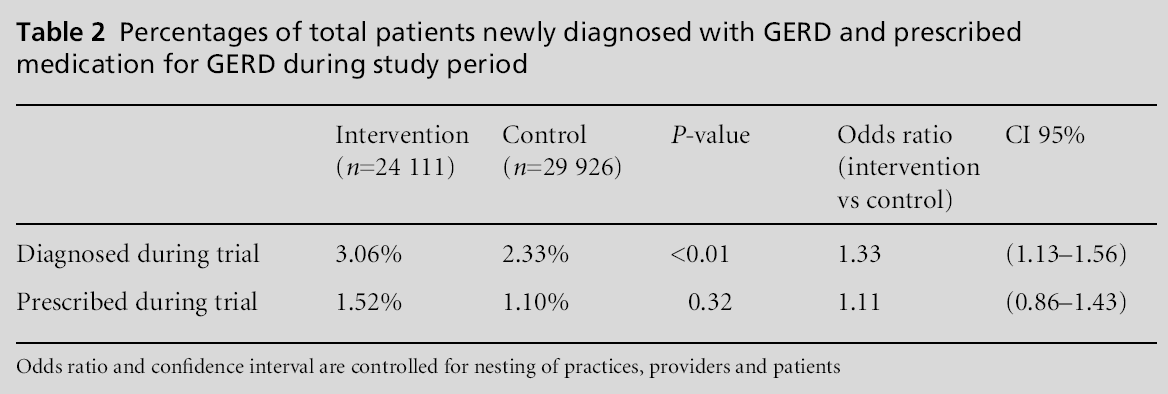
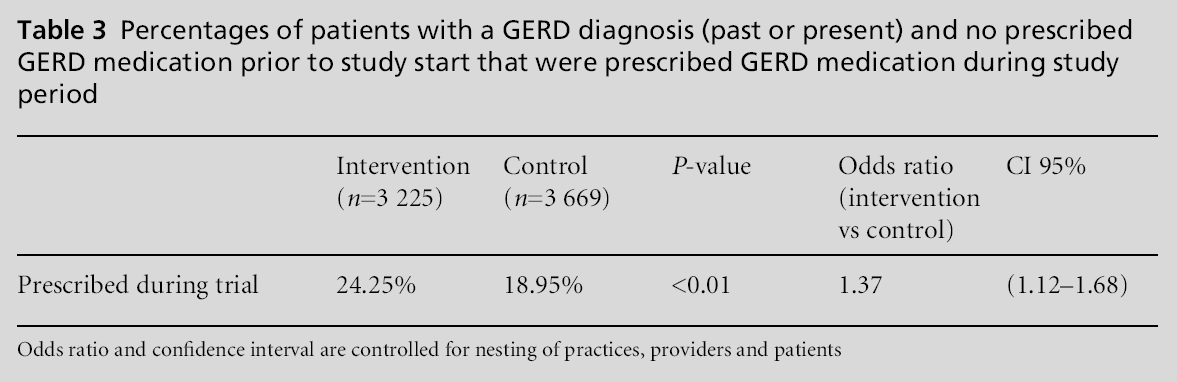
The proportion of patients having GERD during the study period was substantial, 20.87% for the control group and 23.09% for the intervention group. Among those without a diagnosis of GERD at the start of the study, 2.33% in the control group and 3.06% in the intervention group were newly diagnosed with GERD in the during the study period (Table 2). The difference between the two groups was significant at P<0.01 and the odds of being newly diagnosed were higher for the intervention group after adjusting for clustering effects (OR 1.33, 95% CI 1.13–1.56). There was no significant difference in treatment for those newly diagnosed with GERD (Table 2). Looking specifically at new prescriptions for those with a GERD diagnosis who were not on PPI or H2RA medications during baseline, 24.3% of the intervention group and almost 19% of the control group received new treatment. The intervention group had higher odds of treatment compared to the control group (OR 1.37, 95% CI 1.12–1.68; Table 3).
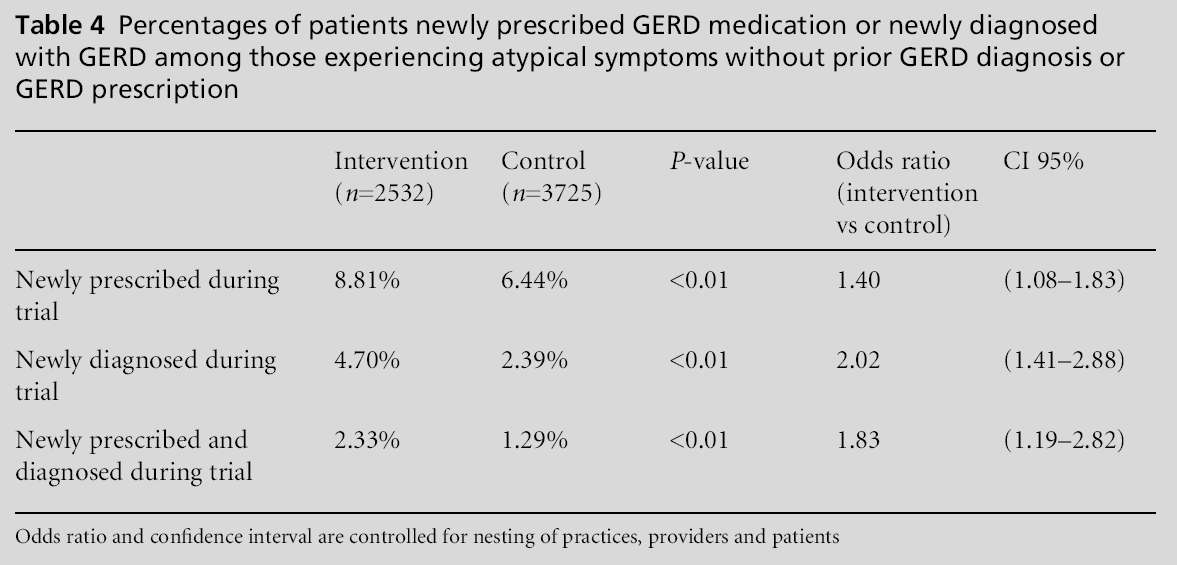
Results for atypical GERD symptoms are presented in Table 4. Looking at patientswith atypical symptoms and no prior diagnosis or treatment for GERD, there were 2532 patients in the intervention group and 3725 in the control group. Those in the intervention group were more likely to receive treatment for GERD (8.8%) than the control group (6.4%) with an odds of treatment of 1.40 (95% CI 1.08–1.83) after controlling for clustering. These include patients who received treatment but may or may not have been given an actual GERD diagnosis. However, patients’ with atypical symptoms in the intervention group were also more likely to be diagnosed with GERD in the study, with 4.7% versus 2.4% in the control (P<0.01). The odds of new diagnosis for the treatment group remained significant after adjustment for clustering (OR 2.02, 95% CI 1.41–2.88). When considering those with atypical symptoms who were both newly diagnosed withGERDand newly treatedwithGERDmedication, the intervention group was more likely to be diagnosed and prescribed medication than the control group (2.3% versus 1.3%) and the difference remained significant after adjustment for clustering (OR 1.83, 95% CI 1.19–2.82; Table 4).
Stratifying by practice location showed that the intervention group in urban practices had significantly more patients newly diagnosed with GERD than the control group in urban practices (OR 1.36, 95% CI 1.08–1.71). Similarly, some differences were seen by medical specialty. Patients seen by internal medicine providers in the intervention group had a significantly higher odds of being newly diagnosed with GERD compared to control internal medicine providers (OR 1.50, 95%CI 1.17–1.92; Table 5). Therewas no difference seen between intervention and control providers in family medicine (OR 1.22, 95% CI 0.96–1.57).
This educational, quality improvement intervention for GERD and atypical symptoms of GERD showed a modest increase in GERD diagnosis and GERD specific treatments for the intervention group. For patients with atypical symptoms of GERD, patients in the intervention group were significantly more likely to be prescribed GERD medications compared to patients in the control group. Most of this increase was due to newly prescribed GERD medications. In addition, for patients with atypical symptoms, those in the intervention group were more likely to be diagnosed with GERD during the course of the study. They were almost twice as likely as those in the control group to be newly diagnosedwithGERD, given atypical symptoms at baseline. These improvements in diagnosis and treatment in real world physician offices for patients with atypical symptoms are encouraging in the light of previous literature suggesting these associations and the role of GERD treatment for atypical symptoms.[9,10]
Although there was a significant increase in diagnosis and treatment in the intervention group, these findings show that we have a long way to go before we reach optimal quality in diagnosis and treatment.
The results of this study should be interpreted in the light of certain limitations. As with any study using office records, data would not be captured if they were not available to the physician using the EMR (e.g. medications prescribed by a specialist but not known to the primary care physician). Also, diagnoses or medications that are recorded only on paper or in EMR text notes would be underestimated since they are not within structured EMR data fields. One example might be if a physician gives a sample PPI or recommends a non-prescription PPI but does not record this in the medication list. Conversely, medications may be overestimated if they are discontinued but not removed from the medication list. However, these data limitations would be unlikely to substantially affect the main results since the methods of entering data in theEMRare unlikely to differ between the intervention and control providers.
Also, there are limitations as to how the results can be generalised. The study included only users of one particular EMR who also participate in the Medical Quality Improvement Consortium. One study found the MQIC population to be similar to the general US population in terms of disease prevalence.[11] However, studies have not examined differences between the MQIC population and other outpatient populations in terms of quality of care.
Diagnostic accuracy and misclassification are potential limitations for both typical and atypical symptoms of GERD. Those who received a GERD diagnosis may not truly have GERD, but we can assume that diagnostic accuracy in this study is similar to that of providers in general practice. Our study shows that EMR prompts can increase diagnoses and prescriptions. However, we have not followed the patients to see if they improve due to treatment. The increase in the diagnosis of GERD and increase in prescribing a PPI or H2RA may not result in better patient outcomes.
Despite these limitations, this study has significant implications for helping physicians to properly diagnose and treat various medical problems and specifically those that may be less common, such as atypical presentation of GERD.
Although undiagnosed atypical GERD is not uncommon, even with an EMR-based decision support and education intervention appropriate diagnosis improved but remained low. Future initiatives may need to focus on a better understanding of barriers and facilitators to this diagnosis.
Marty S Player MD MS (corresponding author) had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was supported in part by GE Healthcare.
Authors confirm that all research completed for this article was approved by the Medical University of South Carolina Independent Review Board.
Not commissioned; externally peer reviewed.
None.