- (2014) Volume 15, Issue 3
Joseph J. Noh1, Sung Hoon Choi2*, Ho Kyoung Hwang1, Chang Moo Kang1 and Woo Jung Lee1
1Division of Hepatobiliary and Pancreas, Department of Surgery, Yonsei University, College of Medicine, Seoul, Korea
2Division of Hepatobiliary and Pancreas, Department of Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
Received March 28th, 2014 – Accepted April 28th, 2014
Context Adrenal cavernous hemangioma is a rare type of tumor that is usually diagnosed post-operatively. There have only been approximately 63 cases reported in the literature to date. Case report We report a case of adrenal cavernous hemangioma in a 27-year-old pregnant woman. The mass was discovered on ultrasonography when she visited a gastroenterologist for vague epigastric discomfort and vomiting. The laboratory tests were within normal limits and did not show any features suggestive of adrenal endocrinologic dysfunction. Computed Tomography (CT) revealed a well-defined 7.8 × 7.8 oval mass in the right adrenal gland with speckled calcifications. The mass was removed by transabdominal laparoscopic surgery. Strong positive immunostaining for CD31 and CD34 with weakly positive staining for podoplanin/D2-40 confirmed the diagnosis of cavernous hemangioma. Conclusions We reviewed 52 case reports of adrenal cavernous hemangioma in an attempt to identify tumor characteristics. More than half of the patients reviewed showed a heterogeneous internal structure of the mass with peripheral patchy enhancement on CT. They also showed focal or speckled calcifications either on X-ray or CT. Nevertheless, many of these characteristics overlap with the imaging phenotypes of other common diseases of the adrenal gland and therefore do not seem to provide definite evidence for differential diagnosis. Laparoscopic approach is a feasible and safe modality to remove adrenal cavernous hemangiomas because they seem to form a rigid fibrotic capsule; hence the risk of bleeding due to surgical manipulation is relatively low.
Adrenal Glands; Adrenalectomy; Hemangioma, Cavernous; Laparoscopy
Adrenal cavernous hemangioma is a rare type of tumor that is usually diagnosed post-operatively. The first case report was published in 1955, [1] and there have only been approximately 63 cases reported in the literature to date. In the present report, we describe a case of adrenal cavernous hemangioma in a 27-year-old pregnant woman whose mass was removed by transabdominal laparoscopic surgery. In addition, we reviewed 52 cases of adrenal cavernous hemangioma reported in the English literature between 1955 and 2013 in an attempt to identify tumor characteristics.
A 27-year-old woman with no significant past medical history was referred to our institution for evaluation of an abdominal mass in the right upper quadrant. The mass was discovered on ultrasonography when she visited a gastroenterologist for vague epigastric discomfort and vomiting that had persisted for one month. At the time of presentation, she denied any possibility of pregnancy; therefore, further examinations proceeded without any obstetric concerns. On physical examination, the abdomen was soft and the mass was not palpable, but she complained of direct tenderness in the right upper quadrant. The laboratory tests were within normal limits, and the endocrinologic examinations did not show any features suggestive of adrenal endocrinologic dysfunction. Ultrasonography demonstrated a 7. 8 x 7. 8 cm clearly demarcated mass in the right adrenal gland with heterogeneous echogenicity and cystic portions (Figure 1).
Computed tomography (CT) revealed a well-defined oval mass with speckled calcifications suggesting multiple phleboliths (Figure 2). The left adrenal gland was unremarkable, and there was no lymph node enlargement. Her abdomen and pelvis seemed normal except for what seemed to be a cystic lesion in the uterus for which further gynecologic ultrasonography was scheduled. On magnetic resonance images (MRI), the mass showed a heterogeneous area with an internal hemorrhagic component suggesting pheochromocytoma or adrenal cortical carinoma. However, endocrinologic examination did not reveal any abnormalities. It was still ambiguous to identify the nature of the mass correctly and evidence with MRI and CT seemed insufficient to rule out malignancy. Therefore further evaluations were pursued and positron-emission tomography (PET) with 18F-fluorodeoxyglucose (18F-FDG) was carried out.
However, it did not show any demonstrable 18F-FDG uptake. Despite no evidence of malignancy or adrenal dysfunction, the tumor was scheduled to be removed surgically because of the symptoms caused by mass effect. She underwent laparoscopic adrenalectomy. At surgery, a round tumor was seen, encapsulated in a dense fibrotic tissue, which was easily dissected from the surrounding organs without invasion (Figure 3). The cut surface showed most of the mass to be spongy and yellowish with central areas of recent hemorrhage. Microscopically, the mass was composed of sinusoidal dilatation and fibrotic septa. Strong positive immunostaining for CD31 and CD34 with weakly positive staining for podoplanin/D2-40 supported the diagnosis of cavernous hemangioma (Figure 4). There was no evidence of malignancy.
During her post-operative recovery, a gynecologic ultrasound was performed to evaluate what had seemed to be a cystic lesion in the uterus on the pre-operative CT scan. On ultrasonography, it was found that the patient was pregnant at 17 weeks’ gestation. Because the patient had denied the possibility of pregnancy prior to the operation, it was not until we performed the gynecologic ultrasonography that the pregnancy was first diagnosed. She was discharged on post-operative day 2 with further obstetrical consultation scheduled.
The aim of the present review on the published case reports of adrenal cavernous hemangioma is to provide a summary of the clinical characteristics of this rare type of tumor. A PubMed search of the literature using the keywords “adrenal cavernous hemangioma” was undertaken, and pertinent journals were reviewed. Language restrictions were imposed to include reports in English only. Information from the case reports was extracted according to the predefined criteria and assessed by two independent reviewers.
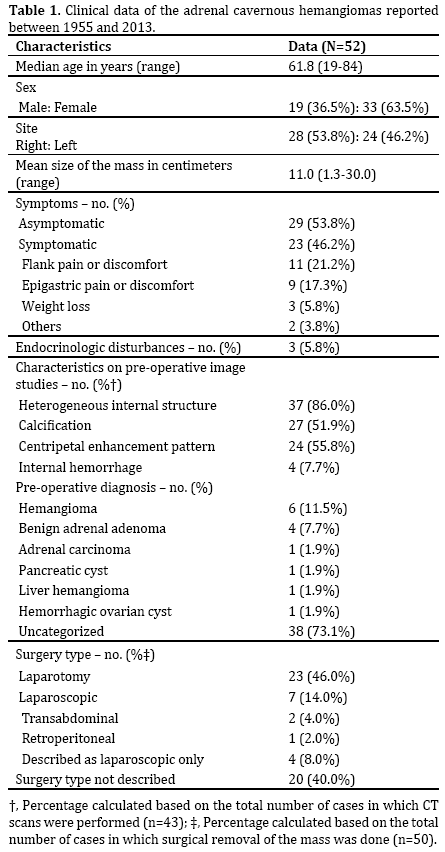
Fifty-two cases of adrenal cavernous hemangioma that were published between 1955 and 2013 were reviewed (Table 1). The median age of the patients at diagnosis was 61. 8 (range: 19-84 years old) years old. There were approximately 1. 7 times more female patients than male patients. Of the 52 patients reviewed, 23 patients (46. 2%) manifested clinical symptoms. The most common symptom was flank pain or discomfort (21. 2%), followed by epigastric pain or discomfort (17. 3%). Only three patients (5. 8%) were reported to show endocrinologic disturbances-one with subclinical Cushing’s syndrome and two with primary hyperaldosteronism. Among the 43 cases in which CT scans were performed, 37 patients (86. 0%) showed a heterogeneous internal structure of the mass and 24 patients (55. 8%) showed peripheral patchy enhancement or a centripetal pattern of enhancement of the mass when contrast was injected. Focal or speckled calcifications were present either on X-ray or CT scans in 27 patients (51. 9%), and internal hemorrhage was noted in four patients (7. 7%). The correct diagnosis was made preoperatively in only six cases (11. 5%). Thirty-eight cases (73. 1%) proceeded to operation without confirmatory diagnosis. Others proceeded to operation with incorrect pre-operative diagnoses. Surgical removal of the mass was performed in 50 cases. In two cases, surgical removal did not take place because one patient expired from an unrelated cause and another patient opted for follow-up due to the small size of the mass and the absence of clinical symptoms. Among the patients whose masses were removed, seven patients (14. 0%) underwent laparoscopic surgery.
The widespread use of abdominal ultrasonography, CT, and MRI has resulted in an increased number of incidental findings of adrenal masses. The prevalence of adrenal incidentaloma, the term coined to describe such masses that are discovered coincidentally without clinical symptoms or suspicion, is approximately 4 percent [2]. As the frequency of adrenal mass detection has increased, the discovery of rare types of tumors such as cavernous hemangiomas, which had not typically been thought to arise from the adrenal gland, has also increased. A substantial number of cases of cavernous hemangioma from other organs such as the liver and skin have been reported, but there are only approximately 60 case reports of cavernous hemangioma from the adrenal gland. Because of the rarity of the tumor and the scarce clinical data on it, precise characteristics of the tumor remain obscure and there are currently no guidelines outlining the optimal diagnostic approach.
In an attempt to delineate the clinical characteristics of adrenal cavernous hemangioma, we conducted a review of the 52 published cases of the tumor. In our analysis, there were a number of notable features distinguishing adrenal cavernous hemangiomas from other types of tumors. First, the median age at diagnosis of adrenal cavernous hemangioma was 61. 8 years old, which is older than the peak age for pheochromocytoma and adrenocortical carcinoma, tumors that are usually identified during the fourth and fifth decades of life [3, 4]. Nonetheless, this does not mean that the onset of the disease is later than that of pheochromocytoma and adrenocortical carcinoma. It is possible that adrenal cavernous hemangiomas are simply detected at older ages because they usually do not manifest clinical symptoms until the size of the mass grows significantly. Second, the number of female patients was significantly higher than that of male patients. This tendency is similar to adrenocortical carcinoma, which also shows a female predominance. Pheochromocytoma, on the other hand, affects men and women equally. In the literature, it is reported that the female predominance is even greater for cavernous hemangioma of the liver (female to male ratio of up to 5 to 1) [5]. Female sex hormones have been suggested to explain the sexual predilection; however, debate remains because although a consistent association between the proliferation of cavernous hemangiomas and increased levels of estrogen has been observed, immunohistochemical staining has failed to show the presence of estrogen receptors in hepatic, orbital, or cerebral cavernous hemangiomas [6-8]. Further studies are required to explain the mechanism by which female sex hormones lead to the proliferation of cavernous hemangiomas. Third, approximately half of the patients reviewed showed no clinical symptoms, especially when the size of the tumor was small. Most were diagnosed clinically after reaching a size larger than 10 cm in diameter when they started to manifest mass effect. Only a limited number of cases reported endocrinologic disturbances. It is hypothesized that the hemangioma itself does not have endocrine activity but arteriovenous malformations within the lesions may lead to enhanced entry of endocrinologically-active metabolites into the bloodstream.
The appearance of the mass on imaging may be of particular interest to clinicians, because many adrenal cavernous hemangiomas are non-functional and do not show pathognomonic symptoms; thereby, the extent to which clinicians depend on imaging in order to establish the diagnosis is significant. More than half of the patients reviewed showed a heterogeneous internal structure of the mass with peripheral patchy enhancement or a centripetal pattern of enhancement when contrast was injected. They also showed focal or speckled calcifications either on X-ray or CT. It has been suggested that this pattern of calcification is secondary to multiple phleboliths that form within the dilated vascular spaces of the hemangioma [9]. The features of the mass on T1-weighted MRI were variable. A number of studies have proposed that adrenal cavernous hemangiomas tend to appear hypointense on T1-weighted MRI [10, 11]; however, in our review, the clinical evidence to support such a claim seemed lacking. The majority of the masses were hyperintense on T2-weighted MRI. It is suspected that the hyperintensity of the mass on T2- weighted MRI is due to the vast amount of blood contained inside. Nevertheless, many of these characteristics of adrenal cavernous hemangiomas overlap with the imaging phenotypes of other common diseases of the adrenal gland and therefore do not seem to provide definite evidence for differential diagnosis.
The optimal treatment guidelines for adrenal cavernous hemangioma have not been established; however, when the size of the tumor is small and there are no endocrinologic abnormalities, routine follow-up with endocrinologic evaluation and image studies may be considered. On the contrary, surgical excision seems to be a reasonable strategy for a large adrenal cavernous hemangioma since a significant number of patients appear to develop local complaints due to mass effect. While laparoscopic adrenalectomy has become the procedure of choice for excision of other adrenal masses, only seven cases (14. 0%) of adrenal cavernous hemangiomas in our review were managed with laparoscopic surgery. The largest tumor removed by laparoscopic surgery was 12 cm in diameter, and the surgeons who performed the surgical procedure reported that a large adrenal cavernous hemangioma should not be considered a contraindication for laparoscopic surgery [12]. We agree that a laparoscopic approach is a feasible and safe modality to remove adrenal cavernous hemangiomas because, unlike hepatic cavernous hemangiomas, cavernous hemangiomas from the adrenal gland tend to form a rigid fibrotic capsule, hence the risk of bleeding due to surgical manipulation is relatively low.
The present case and our review illustrate that distinguishing adrenal cavernous hemangiomas from other common adrenal tumors may be challenging, but they should be included in the differential diagnosis for adrenal incidentaloma.
The authors did not report any potential conflicts of interest.