- (2011) Volume 12, Issue 4
Neila Fathallah1, Michele Zamy2, Raoudha Slim1, Olivier Fain3, Houssem Hmouda4, Kamel Bouraoui1, Chaker Ben Salem1, Michel Biour2
1Department of Clinical Pharmacology, Faculty of Medicine of Sousse. Sousse, Tunisia.
2Pharmacovigilance Centre, Saint-Antoine Hospital. Paris, France.
3Department of Internal Medicine, Jean Verdier Hospital. Bondy, France.
4Intensive Medical Care, Sahloul University Hospital. Sousse, Tunisia
Received April 18th, 2011 - Accepted May 9th, 2011
Context We report a case of massive poisoning with meprobamate leading to acute pancreatitis. Case report A 43-year-old patient with a history of schizophrenia and multiple suicide attempts was admitted to the intensive care unit for severe poisoning with meprobamate (voluntary ingestion of 60 g). On admission, the patient was deeply comatose with low blood pressure and hypothermia. Laboratory analysis revealed leukocytosis and high lipase and amylase serum levels. There was no eosinophilia. Abdominal computed tomography showed pancreatitis grade A. The patient was intubated and ventilated, and intravenous dopamine was infused. The patient regained consciousness and was extubated five days later. Improvement in pancreatic tests was noted several days later. The outcome was favorable. Discussion According to the Naranjo probability scale, meprobamate-induced acute pancreatitis was probable. Acute pancreatitis in meprobamate poisoning is exceptional. The pathogenesis of pancreatitis-induced meprobamate poisoning may be explained by two mechanisms: stimulation of pancreatic secretion secondary to cholinergic activation and pancreatic ductal hypertension. Conclusions The signs of severe meprobamate toxicity are numerous including cardiovascular and central nervous symptoms. Acute pancreatitis should also be added as a possible manifestation of meprobamate poisoning.
Meprobamate, poisoning, pancreatitis
Meprobamate, a carbamate with a barbiturate-like mode of action, has sedative and hypnotic properties. Its adverse drug reactions are rare including drowsiness, confusion, ataxia, amnesia and dependence. However, clinicians have usually been faced with the problem of accidental or voluntary meprobamate poisoning leading to complications that are often serious and sometimes fatal. The most common complications are central nervous system depression and cardiovascular toxicity leading to severe hemodynamic failure and even circulatory collapse [1].
We herein report a case of massive poisoning with meprobamate including disturbances of vital functions and acute pancreatitis.
A 43-year-old woman with a 25-year history of schizophrenia and multiple suicide attempts, treated for the previous 3 years for breast cancer with chemotherapy, radiotherapy and mastectomy, was admitted to the intensive care unit for severe poisoning with meprobamate.
The patient had ingested 60 g of meprobamate (150 tablets) in a suicide attempt on the evening prior to admission. She was found by her mother in a stupourous state. She was immediately transferred to the emergency department.
On admission, the patient was unconscious. The initial evaluation of vital signs revealed the following: blood pressure of 80/40 mmHg, regular pulse rate of 40 min-1, irregular respiratory rate and temperature of 35.6°C. The remainder of the physical examination was unremarkable. No alcohol ingestion, illicit drugs or trauma were present.
On admission, laboratory analysis revealed leukocytosis (white blood cell count was 17.1 x109/L; reference range: 4-10 x109/L); there were no eosinophilia, serum amylase level at 685 IU/L (reference range: 0-100 IU/L) and lipase level at 3,400 IU/L (reference range: 0-160 IU/L). Liver tests revealed alanine aminotransferase (ALT) at 65 IU/L (reference range: 0-40 IU/L), aspartate amino-transferase (AST) at 87 IU/L (reference range: 0-35 IU/L), alkaline phosphatase at 115 IU/L (reference range: 80-250 IU/L), gamma-glutamyl transferase at 32 IU/L (reference range: 5-28 IU/L) and total bilirubin at 17 μmol/L (reference range: 0-17 μmol/L).
Serum calcium and magnesium, glycemia, triglyceridemia, serum lactic dehydrogenase and creatine kinase were normal. Renal function tests were also normal. No toxicological blood screening was done. Abdominal computed tomography showed pancreatic edema without evidence of gallstones. The common bile duct and the liver were normal. A diagnosis of acute pancreatitis grade A was made.
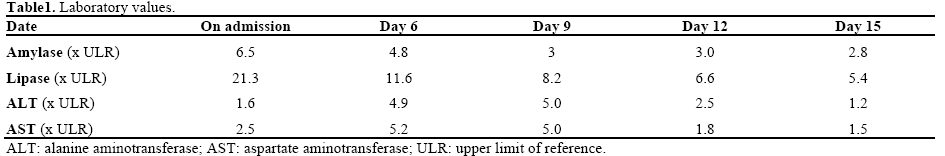
Respiratory and circulatory depression required intubation and mechanical ventilation of the patient. She received a 10-minute intravenous infusion of catecholamine at rates of 5 μg/min/kg BW. The patient was administered “nothing by mouth”, and continuous intravenous serum glucose (5% dextrose solution) infusion was started. The situation improved rapidly and her blood pressure was 110/80 mmHg. Five days later, the patient regained consciousness; she was extubated and was transferred to the psychiatric department. Control of laboratory tests 15 days after admission showed a decrease in serum amylase to 284 IU/L and serum lipase to 871 IU/L (Table 1). Her white blood cell count was 11.2 x109/L. Physical examination was unremarkable: blood pressure of 130/80 mmHg, pulse rate of 85 min-1 and respiratory rate of 20 min-1. Neurological examination revealed an extrapyramidal syndrome; reflexes were present and symmetrical. The patient was discharged a few days later without meprobamate.
Meprobamate is used as anti-anxiolytic and anticonvulsant agent. Meprobamate poisoning remains frequent. Thirty-three years ago, Allen et al. reported that meprobamate was implicated in 7% of admissions due to psychotropic drug over-dosage between 1962 and 1975 in the United States of America [2]. In a recent retrospective review between June 1997 and October 2003, 2.2% of all admissions to the intensive care unit were patients requiring respiratory assistance because of deliberate meprobamate poisoning [3]. Morbidity and mortality are proportional to the duration and severity of the drug-induced coma. Meprobamate overdose is potentially fatal and may occasionally give rise to serious complications. Meprobamate is the main active metabolite of carisoprodol, a centrally active muscle relaxant analgesic. However, the signs of carisoprodol intoxication do not resemble those caused by its metabolite, meprobamate. Meprobamate produces its effects through the GABAergic neurotransmitter system and has a barbiturate-like mode of action at the GABAA receptors. So, meprobamate poisoning includes central nervous system depressing symptoms [4]. It is highly associated with coma, weakness, clonus and hyperactive reflex, tachycardia, hypotension and respiratory depression. In meprobamate poisoning, hypotension consists especially of peripheral arterial vasodilatation and hypovolemia. Although the underlying mechanisms of hypotension are poorly understood, it is thought that meprobamate may depress ventricular contractility being responsible for such hemodynamic failure [3].
Acute pancreatitis in meprobamate poisoning is exceptional [5]. In our patient, the diagnosis was based on laboratory tests and imaging features. There are various possible mechanisms for meprobamate-induced pancreatitis. The consequences of meprobamate poisoning, such as hypothermia and hypovolemia, are predisposing factors to acute pancreatitis. Prolonged hypothermia induces circulatory stasis in some organs, including the pancreas, leading to thrombosis and infarction. Hypovolemia, because of an increased viscosity of pancreatic fluid leading to proenzyme release, predisposes to acute pancreatitis, and may also aggravate a preexistent necrosis [6]. Other possible mechanisms of meprobamate poisoning-induced pancreatitis may also be explained by the stimulation of pancreatic secretion secondary to cholinergic activation and pancreatic ductal hypertension secondary to the increased viscosity of the pancreatic fluid, leading to peripheral duct rupture and proenzyme release [7]. According to the Naranjo probability scale, meprobamate-induced acute pancreatitis was probable in our case [8].
The modalities of treatment for meprobamate poisoning are numerous. They are based on supportive therapies. Drug elimination by emptying the gastrointestinal tract, followed by the administration of activated charcoal, is standard intervention [9]. In some cases, removing the meprobamate from the circulation may require forced diuresis, peritoneal dialysis and even hemodialysis. Mechanical ventilation may be necessary in some cases. Fluid resuscitation and the use of vasoactive agents may be required to treat hypovolemia and hypotension. Hemoperfusion may be useful when usual supportive therapies are not successful or if there are complications [1].
Since its introduction, clinicians have been faced with problems linked to acute poisoning by meprobamate. The symptoms of severe meprobamate toxicity are numerous, including cardiovascular and central nervous manifestations. Acute pancreatitis should also be added as a possible manifestation of meprobamate poisoning.
The authors have no potential conflict of interest