- (2015) Volume 16, Issue 3
Marvin Schober1, Ralf Jesenofsky2, Ralf Faissner2, Sebastian Krug1, Cornelius Weidenauer2, Wolfgang Hagmann3, Stephan L Haas4, Rainer L Heuchel5, Matthias J Löhr4,5
1Division of Gastroenterology, Endocrinology and Metabolism, University Hospital, Philipps- UniversitaetMarburg. Marburg, Germany.
2Department of Medicine II and Department of Gastroenterology, Hepatology and Infectious Diseases, University Medical Center Mannheim (UMM). Mannheim, Germany.
3German Cancer Research Center (DKFZ), Epigenomics and Cancer Risk Factors, Lung Cancer Genomics/Epigenomics. Heidelberg, Germany.
4Gastrocentrum, Karolinska University Hospital of Stockholm. Stockholm, Sweden. 5Department of Clinical Science, Intervention and Technology (CLINTEC), Karolinska Institutet. Stockholm, Sweden
Received November 4th, 2014 – Accepted March 25th, 2015
Context Pancreatic ductal adenocarcinoma is a dismal disease with one of the worst prognoses amongst solid tumors. Its ability to develop chemoresistance mechanisms towards cytotoxic drugs is the main cause of treatment failure. Objective Here, we have established a drugresistance model for pancreatic cancer in which Capan-1 pancreatic carcinoma cells (designated Capan-1 5-FU2000) acquired 5-fluorouracil (5-FU) resistance and were used as a paradigm to reveal alterations in intracellular signaling cascades that. Those alterations may contribute to the circumvention of apoptosis during the course of the disease, culminating in treatment failure. Methods We made use of 2-D-gelelectrophoresis, mass-spectrometry, sandwich-ELISA and western blotting to compare the proteomic expression patterns of respective mediators involved in pro- and antiapoptotic as well as inflammatory processes in both cell lines. An ATP-based chemosensitivity assay validated the chemoresistant phenotype of the Capan-1 5-FU2000 clones. Results We detected specific changes in our resistant cell clones in particular a decreased expression of S100A4. We also found a decreased basal phosphorylation of SAPK/JNK and P38. The expression of the pro-apoptotic mediators Bok and Bad was down- and up-regulated in these cells, respectively. In case of NfkB p65 and IkB-alpha treatment with 5-FU (2000 μg/mL for 96 h) markedly induced phosphorylation in native Capan-1 cells. In contrast in resistant clones it decreased phosphorylation of NfkB p65 and did not affect IkB-alpha phosphorylation. Basal phosphorylation of S6-ribosomalprotein was markedly increased in resistant clones, treatment with 5-FU decreased this phosphorylation, while in native Capan-1 cells it was vice versa. Conclusion Thus we can conclude that several pathways were found to be altered in chemoresistant Capan-1 5-FU2000 cells. Moreover that these alterations are most likely a consequence of the multistep adaption towards gradual cytotoxic exposure culminating in a chemoresistant phenotype. Interfering with these pathways may possibly reverse the phenotype and thus open up alternative treatment options.
Pancreatic Neoplasm
PDAC pancreatic ductal adenocarcinoma Capan-1 5-FU2000 cloned Capan-1 cells resistant to 5-FU concentrations of 2 μg/mL in culture medium TDC test drug concentration 2D-PAGE 2D-polyacrylamide-gel electrophoresis
Pancreatic ductal adenocarcinoma (PDAC) is a disease of the elderly, seen mainly in people older than 50 years of age [1]. In 2012, its incidence ranked 10th in the annual statistics of newly diagnosed carcinomas with 43,920 cases per annum. The median survival time of about 6 months and long-term survival of approximately 4% characterizes PDAC as a devastating disease even amongst malignant neoplasias [2, 3]. Thus the mortality rate for PDAC almost equals its incidence and it is currently the 4th leading cause of cancer deaths in the US [4]. Projections of cancerrelated death rates recently published by Rahib and colleagues even proclaim that pancreatic carcinoma will become the 2nd leading cancer killer by 2030 [5].
Several risk factors have been described for pancreatic cancer, including chronic pancreatitis, diabetes mellitus, smoking and germline mutations in genes such as BRCA2 [6]. A disease previously more common in men than in women, this trend has been changing in recent years, conceivably due to the rising number of women who smoke [7]. According to Raimondi, early diagnosis and increasing population longevity will lead to an increase in this lethal disease in the years to come [5, 8]. The clinical course of PDAC is predominantly that of a long asymptomatic progression leading to diagnosis, usually at an advanced stage of the cancer. With the neoplastic tumor mass most frequently localized in the pancreatic head (70% of tumors), followed by the body and then the tail, 80% of pancreatic cancer patients are already beyond curative therapy when diagnosed [1]. To date, surgery in the early stages of the disease is still the only chance of a cure. The aggressive and early metastatic behavior of PDAC make surgery a difficult choice, especially when one considers its retroperitoneal topography adjacent to major gastrointestinal vessels, making even curative resection the exception rather than the rule [3, 9]. Unfortunately, a curative, non-surgical option is still not in sight. Current chemotherapeutic regimes are restricted to neoadjuvant, adjuvant or palliative treatments, mostly using gemcitabine-based chemotherapy protocols. Recently, FOLFIRINOX (a combination therapy using oxaliplatin, 5-fluorouracil (5-FU), irinotecan and folinic acid) has shown significant survival benefits in patients with good performance status [10]. However, this palliative regimen is still being evaluated in ongoing clinical trials such as the CONKO-007 Study (EUDRACT Nr. 2009-014476- 21) amongst others [11-14]. Thus, it is still true to say that pyrimidine analogues such as gemcitabine or 5-FU, represent the backbone of pancreatic cancer treatment.
The chemotherapeutic restrictions based on PDAC's almost unique ability to acquire a variety of drug resistance mechanisms finally lead to the intensive research efforts of the past decades and the results have proven to be of importance in overcoming apoptosis induced by cytotoxics [15-23]. Recently, our group was able to contribute to that by demonstrating that membrane transporters are also of particular relevance in the chemoresistance of PDAC. Continuous treatment with 5-FU and/or gemcitabine induced the up-regulation of several multidrug resistance protein (MRP)-transporters, including MRP3, MRP4 and MRP5 in 5-FU-resistant Capan-1 cell clones (Capan-1 5-FU2000) when compared to the parent cell line [24]. MRP5, in particular, contributed to 5-FU resistance, as knock-down of MRP5 mRNA resulted in increased sensitivity towards 5-FU retreatment [24].
Nambaru and colleagues interestingly demonstrated similar results for MRP5 in Patu-02 cells [25] that, together with a study by our group in the same year [26], illustrated that altered transporter expression is important in overcoming the toxic effects of prolonged drug treatment.
To further elucidate the processes underlying adaptation towards pyrimidin alalogues - in particular 5-FU-, we now successfully established a model of chemoresistance using human pancreatic carcinoma cells - Capan-1. Thus, the establishment and characterization of, and alterations in, intracellular signal transduction in this unique 5-FU resistant cell line - designated Capan-1 5-FU2000 - offers supplementary insights and is the main focus of this report. To the best of our knowledge intracellular alterations in either pro- or anti-apoptotic pathways as well as inflammatory mediators in an acquired chemoresistance model of Capan-1 pancreatic carcinoma cells have not been reported so far.
The following results point out several proteins that showed differential regulation after adaptation towards 5-FU and thus might be relevant to tumor cell survival and might as well help to explain treatment failure in a clinical context
Tissue Culture
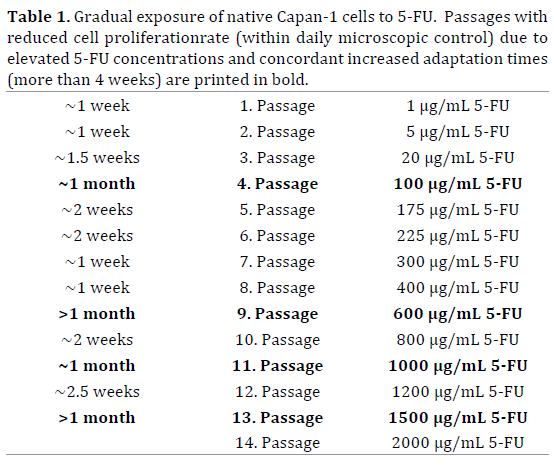
Native (parental) human pancreatic carcinoma cells (Capan-1), derived from a distant PDAC liver metastasis [27-29], were obtained from ATCC, Mannassas, VA (ATCC Number: HTB-79). The cells were adapted gradually to increasing doses of 5-FU (starting with 1 μg/mL 5-FU, added to the culture medium, and reaching 2 μg/mL within 8 months, after 14 passages) to establish acquired 5-FU-resistant Capan-1 clones (designated as Capan-1 5-FU2000).
ATP-Based Chemosensitivity Assay
The acquired resistance of the cloned Capan-1 cells was analyzed using an ATP-based assay as described previously [30-32]. Both the native Capan-1 and the cloned Capan-1 5-FU2000 cells were incubated in 96- well plates with 6 different concentrations of 5-FU for 5 to 7 days. The test drug concentration (TDC) of 5-FU was 22.5 μg/mL (172 μM = 100%) (Figure 1). All tests were performed as biological triplicates by CellTrend GmbH, Luckenwalde (Luckenwalde, Germany). Cytotoxicity was then calculated using the measured absorption rate (A) of the tested cell lines:
Cytotoxicity [%] = (1-[A treated–A blank]/[A neg–A blank]) x 100.
The inhibitory effects of 5-FU were expressed as the concentration that inhibits 50% and 90% of cell growth (IC50/IC90).
2D-Gel Electrophoresis
Two-dimensional polyacrylamide gel electrophoresis (2D-PAGE) was used to analyze differences in the proteomic expression patterns of native Capan-1 and Capan-1 5-FU2000 cells. Proteins were resolved by their specific isoelectric points in the first dimension, and in the second dimension by their specific molecular weight. Cells were lysed and a total of 50–75 μg of each lysate (concentration (c) = 1–2 μg protein/μL) was loaded on to linear immobilized pH gradient strips (IPG-Strip, Immobiline DryStrips pH 4–7; Amersham Biosciences, Buckinghamshire, UK). One dimensional (1D) separation was performed using the IPGphor system (Amersham Biosciences, Buckinghamshire, UK). Following 2nd dimension separation, spot detection was achieved with silver staining, or Coomassie Brilliant Blue G250 - if required for mass spectrometry. Each experiment was repeated 7 times. Subsequent spot analysis after staining (including densitometry) was performed using a GS-800 calibrated densitometer (Bio-Rad, München, Germany) and the results were analyzed using PDQuest 7.1 software (Bio-Rad, München, Germany) [33].
Quantitative Real-Time PCR (QRT-PCR)
Two-step QRT-PCR was used to quantify altered gene expression. Total RNA was isolated from cells, reversetranscribed and amplified in an Mx3000P cycler (Stratagene, Amsterdam, The Netherlands) using Absolute™ QPCR SYBR® Green Mix (Abgene, Epsom, UK). Relative quantification compared to the housekeeping gene, RPL13A, was performed using the “delta-delta-Ct” method with the following primers: S100α4, 5’-CTTGCACACGCTGTTGCTAT- 3’ and 5’-AACTTGCTCAGCATCAAGCA-3’ (467 bp fragment, bases 73–539) [34].
Western Blotting
The expression of specific proteins was analyzed using Western blotting. Equal amounts of native and 5-FU-resistant Capan-1 cell lysates were separated by SDS-PAGE, blotted onto polyvinylidene difluoride (PVDF) membranes and probed using specific primary antibodies and horseradish peroxidase (HRP)-conjugated secondary antibodies. Results were visualized using the chemiluminescence SuperSignal West Femto Chemiluminescent kit, Pierce (Pierce, Rockford, IL, USA, now part of ThermoFisher Scientific). Each test was performed as biological triplicates. Testing of the proapoptotic proteins, BOK and BAD, was performed according to the manufacturer’s instructions using the following kits: Phototope®-HRP Western Blot Detection System #7071 (Cell Signaling Technology Inc., Danvers, MA revised 04/15/08), and the Pro-Apoptosis Bcl-2 Family Antibody Sampler Kit #9942 (Cell Signaling Technology Inc., revised 01/11/07). Since these experiments were performed only once in each case, the results are only indicative.
Cells were lysed according to the manufacturer's protocol using cell lysis buffer® #980 (Cell Signaling Technology Inc., rev. 08/16/07).
Phosphosensitive semiquantitative analysis was performed for the following proteins: ribosomal protein S6 (rpS6), nuclear factor kappa B (NfkB), nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha (IkB alpha), p38 alpha and stress-activated protein kinase/c-Jun N-terminal kinase (SAPK/JNK) using the PathScan® Cell Growth Multi-Target Sandwich ELISA Kit #7239 (Cell Signaling Technology Inc., new 08/07), and the PathScan® Inflammation Multi-Target Sandwich ELISA Kit #7276, (Cell Signaling Technology Inc., new 10/07) according to the manufacturer's protocol.
Treatment groups are as follows:
• Parental Capan-1: no 5-FU;
• Resistant Capan-1 (abstention): withdrawal of 5-FU from the culture medium for 4 days;
• Parental Capan-1 (treatment): 2 μg/mL 5-FU for 4 days
• Resistant Capan-1 (abstention) + retreated: 5-FU withdrawal for 4 days followed by the addition of 2 μg/ mL 5-FU for a further 4 days.
The treatment duration was 4 days during which time the medium containing 5-FU was replenished every 48 hours.
The results are presented as the mean of 2 technical replicates.
To achieve 5-FU resistance, chemosensitive Capan-1 cells were incubated with increasing concentrations of 5-FU in the culture medium (Table 1). To confirm that the Capan-1 5-FU2000 cloned cell line was indeed resistant to 5-FU, an ATP-based chemosensitivity assay was performed by CellTrend GmbH, Luckenwalde (Luckenwalde, Germany). The resistant cell line demonstrated a 27-fold increase in tolerance towards 5-FU, when the inhibitory concentration (IC) 50 values were compared to the native Capan-1 control cells: 63.6 μg/mL 5-FU in Capan-1 5-FU2000 (concentration based on tested IC values) vs. 2.4 μg/mL in native Capan-1 cells (Figure 1). In this experiment, 2 μg/ mL 5-FU resulted in a growth inhibition in ~50% of native Capan-1 cells (IC50).
To detect intracellular changes in protein expression, a multivariate approach was undertaken: 2D-PAGE was performed followed by gel staining and characterization of a protein spot that was clearly differentially regulated between the native and resistant cell lines (Figure 2). The differentially regulated spot was characterized via mass spectrometry as S100α4, a calcium-binding protein. In addition, Western blotting was performed to validate the observed difference in the respective proteomic expression patterns. The results confirmed a marked decrease in the expression of S100α4 at the protein level in 5-FU resistant cells (Figure 3). In the current study, S100α4 expression in 5-FU-resistant Capan-1 cells was independent of 5-FU treatment as resistant cells showed a comparable downregulation of S100α4 after withdrawal of 5-FU from the culture medium.
Following ELISA assays, native cells and resistant Capan-1 cells revealed comparable basal levels of NfkB p65 and IkB-alpha phosphorylation. Treatment with 5-FU induced a marked increase in the phosphorylation of NfkB p65 and IkB-alpha in native Capan-1 cells; however, in resistant cells, 5-FU treatment decreased NfkB p65 phosphorylation, but had no effect on the phosphorylation of IkB-alpha (Figures 4 and 5).
The basal phosphorylation of ribosomal protein S6 was much higher in 5-FU-resistant clones than in the native cell line. Retreatment with 5-FU after 4 days of abstention interestingly resulted in decreased rpS6 phosphorylation in 5-FU-resistant cells, but had the opposite effect in native Capan-1 cells in case of treatment with 5-FU (2 μg/mL) (Figure 6).
ELISA testing for SAPK/JNK and P38 phosphorylation in 5-FU-resistant clones revealed a decrease in the basal phosphorylation levels of these proteins compared to the native cell line (Figures 7 and 8).
Supplementary western blotting experiments indicated differential expression of the pro-apoptotic mediators, BOK and BAD. Compared to the native cell line, BOK was down-regulated in 5-FU-resistant Capan-1 cells cultivated in medium with 2 μg/mL 5-FU. Withdrawal of 5-FU for 4 days increased BOK expression to levels comparable to native Capan-1 cells (Figure 9, upper panel). In contrast, BAD expression was up-regulated in 5-FU-resistant Capan-1 cells, independent of stimulation with 5-FU (Figure 9, middle panel). Actin was used as the loading control (Figure 9, lower panel).
Figure 9. Differentially regulated expression levels of BOK and BAD in (1) Capan-1 native cells: medium contained no 5-FU; (2) Capan-1 5-FU2000 cells (resistant), abstention: 5-FU withdrawn from medium; (3) Capan-1 5-FU2000 cells (resistant): medium contained regular 5-FU dose of 2 μg/mL. The blue square (see BOK line3 represents the densitometric area measured. Duration of treatment/incubation=22 hours.
Various cellular mechanisms have been characterized in recent decades. With respect to the model of acquired chemoresistance presented in the current study, we took a further step in elucidating intracellular differences in signal transduction pathways in Capan-1 cell lines adapted to drug-resistance. Differences in expression patterns of transporter proteins in these cells, in particular the multidrug resistance protein (MRP) family, have been described previously by our group with respect to known alterations in other tumor types displaying a resistance phenotype.
In the current study, we successfully established 5-FUresistant Capan-1 cell clones (Capan-1 5FU2000) following gradual exposure of chemosensitive cells to 5-FU during culture. We thereby demonstrate that acquired 5-FU resistance is associated with alterations in the proteomic expression pattern as well as the phosphorylation levels of some of the respective pro- and anti-apoptotic, and inflammatory regulator proteins.
First of all proving the acquired 5-FU resistance of our cell clones by comparing the IC 50 values of Capan-1 5FU2000 to the native cell line we observed a 27-fold increase in tolerance to 5-FU in the resistant cell line (Capan-1 5FU2000 = 63.6 μg/mL vs. 2.4 μg/mL in native Capan-1 cells. The concentration was based on the tested IC values - Figure 1). Comparative analysis of the parent and resistant cell lines clearly revealed a differential regulation of various pro- and anti-apoptotic mediators and of proteins known to be involved in cellular inflammation. We verified a decrease in expression of the calcium binding protein, S100α4, in resistant Capan-1 5FU2000 cell lines compared to the Capan-1 parent cells. S100α4 is thought to be involved in the regulation of chemoresistance and metastasis. Since previous reports have demonstrated that S100α4 knockdown sensitizes pancreatic carcinoma cells to gemcitabine treatment, S100α4 has been tested as an early diagnostic marker in various cancers, including the pancreas [35-38]. Furthermore, it is known that S100α4 is capable of suppressing BNIP3 promoter activity via the activation of NfkB, which is associated with chemoresistance in PDAC cell lines [37, 39]. The current results agreed with our previously published data, which demonstrated the down-regulation of S100α4 expression by 82%, and confirmed this down-regulation at the RNA level in 5-FU-resistant Capan-1 cells [34]. However, in contrast to the referred data of our group and the given data from other researchers, it remains contradictory if knockdown of S100α4 is associated with an increased sensitivity of pancreatic cancer cells towards cytotoxic treatment [34-40].
Our obtained data also conclusively reinforces the potential involvement of S100α4 in acquired chemoresistance as it illustrates a direct drug-related alteration in proteomic expression besides demonstrating the interdependence of redundantly regulated inflammatory signaling pathways, such as NfkB. The proteomic alteration fits quite well with a concordant decrease in S100α4 [34] since we observed a marked down-regulation of NfkB p65 and IkB-alpha phosphorylation in Capan-1 5FU2000 clones, according to the decrease in S100α4 levels in the resistant cell line. Those changes in signal transduction pathway responsiveness are obviously established during the adaptation of the cell line in response to a permanent 5-FU stimulus. In contrast, when native Capan-1 cells were treated with 5-FU (2 μg/ mL for 96 h; Figure 4) we observed a marked increase in NfkB phosphorylation levels. This effect might, therefore, be considered as an early cellular mechanism that has to be bypassed whilst establishing survival mechanisms in response to consequent cytotoxic stress.
With respect to our results regarding the expression of SAPK/JNK and P38 (Figures 7 and 8), their decrease in basal phosphorylation levels in case of Capan-1 5FU2000 cells also fits quite well with the rest of our data. Since phosphorylation represents a physiological cellular activation in context of cellular stress [41-44] in response to e.g. osmotic-, ultraviolet- or pro-inflammatory cytokine- mediated stress this might best be assumed as cellular habituation while permanent 5-FU exposure selects for adequate signal transduction response mechanisms [41- 49]. Thus their respective signaling pathways might necessarily be bypassed in the process of establishing an acquired 5-FU resistance to circumvent apoptosis.
We moreover found that the phosphorylation of ribosomal protein S6 (rpS6) showed a marked increase in resistant clones, but a decrease in response to treatment with 5-FU. Again this was in contrast to native Capan-1 cells where rpS6 phosphorylation was regulated with respect to the 5-FU treatment (Figure 6). Ribosomal protein S6 is thought to be important in the translation of mRNA into proteins needed for cell cycle progression as well as in the process of cellular translation itself [50, 51]. While rpS6 phosphorylation is known to be linked with increased intracellular translation frequencies, this result might be indicative of cytotoxic-induced elevated translation rates due to cellular stress [50]. Once more, the observed results are in line with elevated phosphorylation levels seen in Capan-1 5FU2000 clones, particularly since the measured basal expression levels of rpS6 were equal for native and resistant cells. One possible regulator responsible for this phenomenon might be m-TOR, a serine/threonine protein kinase known to be of relevance in tumor growth mostly via its role in PI3K/AKT signaling [52].
Using western blotting the expression patterns of the pro-apoptotic mediators, BOK and BAD, were down- and up-regulated respectively in 5-FU-resistant cell clones (Figure 9) [53-56]. In the case of BOK, it again seems reasonable that pro-apoptotic protein levels decrease as a consequence of cellular adaptation towards 5-FU exposure. Nevertheless, this was not the case for BAD. The observed increase in BAD protein levels might be best interpreted either as a loss-of-function in this signaling cascade, or it is possible that the observed increase in BAD protein is balanced by an undiscovered anti-apoptotic mediator [57]. However, it should be emphasized that the western blots presented in the current study are strictly indicative since the experiments were performed just once.
In summary, we successfully established 5FU-resistant Capan-1 cell clones adapted from a chemosensitive native Capan-1 cell line. Comaparing both cell lines we revealed a differential regulation of key mediators known to be relevant for inflammatory- as well as pro- and antiapoptotic cell signaling pathways when regarding their respective expression- and phosphorylation pattern.
The elegance of this model might be better assessed in the context of a recent publication by Jones and colleagues who presented a broad-spectrum genetic analysis of 24 pancreatic cancer samples. In their study, they discovered an average of 63 genetic alterations in every case of PDAC, which affected a core of 12 overlapping signaling pathways that were each genetically modified in 67%– 100% of the analyzed samples [58]. This result illustrated that a relatively large number of genetic alterations can affect a reasonably small number of core pathways. Those findings by Jones and colleagues call on targeted therapies that address nodal points or redundant regulators in cell signaling mechanisms rather than trying to target single mutated genes. Thus the next step in pancreatic cancer treatment becomes apparent and may allow us to kill two birds with one stone in helping to address the modern problem of cellular drug resistance. However, as we know from other types of cancer, and have seen in the current study, the processes underlying the hallmarks of cancer are mostly regulated by redundant pathways, thus the targeted treatment of only one cancer cell pathway may be insufficient as it will enable cancer cell survival following the activation of redundant alternative pathways culminating in drug resistance [59, 60].
In the current study, we successfully established 5-FUresistant Capan-1 cell clones (Capan-1 5FU2000) following gradual exposure of chemosensitive cells to 5-FU during culture. We thereby demonstrate that acquired 5-FU resistance is associated with alterations in the proteomic expression pattern as well as the phosphorylation levels of some of the respective pro- and anti-apoptotic, and inflammatory regulator proteins. Our model might therefore represent a paradigm to discover and identify starting points and potential targets for future therapies that aim at overcoming the difficulty of acquired chemoresistance.
This work was supported by a grant from the Ministry for Science, Research and the Arts (MWK), Stuttgart, Germany; by Dr. Hans & Lore Graf-Stiftung, Kaiserslautern, Germany, and by the National Swedish Science Foundation (VR K2008-55X-20655-01-3).
Marvin Schober: Literature research, manuscript writing; experiments
Ralf Jesenofsky, Ralf Faissner, Wolfgang Hagmann: supervision, manuscript writing
Sebastian Krug, Cornelius Weidenauer: manuscript review and writing
Rainer L Heuchel, Stephan L Haas: manuscript revision and writing
J Matthias Löhr: study design, idea, supervision, manuscript review and writing. All authors have read and approved the final version of the manuscript.
The authors had no conflicts of interest