- (2010) Volume 11, Issue 3
Zafer Teke1, Neslihan Inci Zengin2, Fuat Atalay1, Kerem Karaman1, Ali Eba Demirbag1, Meral Akdogan3
Departments of 1Gastroenterological Surgery, 2Pathology, and 3Gastroenterology, Turkey Yuksek Ihtisas Teaching and Research Hospital. Ankara, Turkey
Received: 14 February 2010 Accepted: 24 February 2010
Context Heterotopic pancreas is defined as the presence of pancreatic tissue, outside its usual location, which lacks anatomical and vascular continuity with the pancreas proper. Despite the development of modern diagnostic procedures, it is still difficult to differentiate heterotopic pancreas from benign or malignant tumors and other tumor-like lesions. Frozen examination of mucinous lesions arising from heterotopic pancreas may represent a diagnostic problem. A decision may be very difficult and it is sometimes impossible to decide on the basis of the frozen sections whether a lesion is benign or malignant. Case report We report a tumor-like lesion mimicking a mucinous (colloid) carcinoma arising in heterotopic pancreatic tissue in the prepyloric antrum of a 56-year-old woman which was found incidentally during an elective laparoscopic cholecystectomy for cholelithiasis. The tumor was treated by wedge resection and, in the frozen section examination, there were pancreatic ducts in the proper muscle layer, pancreatic acini with islets of Langerhans under the serosal surface and mucinous lakes close to the heterotopic pancreatic tissue and to a peripheral nerve. Conclusion The significance of this unusual lesion is its potential confusion with mucinous (colloid) carcinoma or other mucous tumors. Such confusion is more likely to occur if the tissue sample is selective or limited, and the presence of pancreatic tissue cannot be verified. Therefore, we believe that a choice of local excision, wedge resection or more extensive eradication be determined only after intraoperative, pathological confirmation of the complete and accurate diagnosis.
Carcinoma; Frozen Sections; Pancreas; Pyloric Antrum; Stomach
IPMN: intraductal papillary mucinous cystic neoplasm; PanIN: pancreatic intraepithelial neoplasia
Heterotopic (ectopic, aberrant) pancreas is defined as the presence of pancreatic tissue, outside its usual location, which lacks anatomical and vascular continuity with the pancreas proper. Heterotopic pancreas may be found incidentally in the stomach, duodenum, small intestine, Meckel’s diverticulum or biliary tract by upper endoscopy, upper gastrointestinal contrast radiography, laparotomy or autopsy. The frequency of ectopic pancreas has been estimated as 1 case per 500 explorations of the upper abdomen or 0.6- 13.7% of autopsies [1, 2]. Heterotopic pancreas is usually asymptomatic; however, it may manifest as a mass lesion with obstruction, ulceration or bleeding, or it may accompany pathological changes known to occur in the pancreas, such as acute pancreatitis [3, 4], epithelial cysts or cystic dystrophy [5], pancreatic pseudocyst [3], and exocrine [6, 7] or endocrine [8] neoplastic transformation. Despite the development of modern diagnostic procedures (endoscopic biopsy and endoscopic ultrasound), it is still difficult to differentiate heterotopic pancreas from benign or malignant tumors and other tumor-like lesions [9]. Unfortunately, an endoscopic biopsy of a submucosal tumor often samples only the overlying mucosa. To verify the diagnosis, it is often necessary to remove the entire lesion.
We herein report a case of a tumor-like lesion mimicking mucinous (colloid) carcinoma developed from heterotopic pancreas of the prepyloric antrum which was incidentally encountered during an elective laparoscopic cholecystectomy for cholelithiasis . This pathological entity must be evaluated cautiously by both the surgeon and the pathologist. This article describes how tumor-like lesions mimicking mucinous carcinoma in the heterotopic pancreas should be handled with a special reference to frozen section examination.
A 56-year-old woman was admitted to an outpatient surgical consultation complaining of intermittent abdominal pain in the upper right quadrant, often radiating to the back, and nausea and vomiting. She had first noted the pain 3 months previously. She stated that the pain occurred approximately every 3-4 weeks, and that each episode lasted several days at a time. The patient had undergone an appendectomy and simple ovarian cyst surgery in her past medical history. The family and social histories were non-contributory. She denied any symptoms of dysphagia, hematemesis, melena, anorexia, weight loss or change in her bowel habits. On admission, physical examination revealed upper right quadrant tenderness to palpation, but there was no guarding or rebound. Pertinent laboratory tests, including serum amylase and lipase, and serum tumor markers, such as CA 19-9 and carcinoembryonic antigen (CEA), were within the normal range. Transabdominal ultrasonographic examination showed the presence of multiple gallstones, the largest being 1 cm in diameter, in a gallbladder with thick walls. The liver was normal, and no prominent intrahepatic biliary dilatation was noted. Cholelithiasis with chronic cholecystitis was diagnosed. Upper gastrointestinal endoscopy revealed alkaline reflux gastritis and bulbitis. No mucosal or submucosal mass was identified during endoscopic examination. In order to prevent any additional episodes of biliary colic in this patient, the decision to perform an elective laparoscopic cholecystectomy was made. We began the operation with a standard four-port technique. The liver was normal at laparoscopic exploration of the abdomen, and the gallbladder was hydropic and thickwalled without pericholecystic adhesions. An incidental mass on the anterior side of the wall of the prepyloric antrum of the stomach was encountered in the course of performing the laparoscopic cholecystectomy without any other pathological findings (Figure 1). Due to the uncertainty of the nature of the lesion and our concern that it might be a malignant tumor, we decided to convert the laparoscopic procedure to an open laparotomy. An exploratory laparotomy confirmed a 2.5 cm lesion containing gelatinous mucinous material in the prepyloric antrum of the stomach with serosal thickening and a nodule. The tumor did not appear to infiltrate the surrounding structures. The lesion was excised locally, and the specimen was then sent for frozen section examination.
There were microcysts having dimensions of 0.05 to 0.1 cm in the proper muscle layer, pancreatic tissue under the serosal surface, and mucinous cystic areas side by side at the gross appearance of excised material (Figure 2a). The microscopic frozen section revealed pancreatic acini, ducts and islets of Langerhans localized in the wall of the prepyloric antrum. Glands and ducts were sprinkled in the submucosa, muscularis propria and subserosa (Figure 2b). Acini and islets were located at the subserosal site. The consultant pathologist thought it to be a benign lesion and, in particular, a heterotopic pancreas. The microscopic view of the serial frozen sections revealed mucinous lakes which contained some epithelial cells and dystrophic calcifications close to a peripheral nerve. There was no inflammation, overt ductal dysplasia or neoplasia. The pathologist phoned the operating room and explained to the operating surgeon that the lesion could be a mucinous tumor originating from the heterotopic pancreas. On the other hand, she hesitated to report the lesion as a benign or malignant tumor. However, she felt that the lesion could really be a mucinous (colloid) carcinoma because of an area of perineural invasion of mucinous material. The paucicellular mucin lakes included epithelial cells with some atypia (Figure 2cd). She told the surgeon that the histopathological decision had to be made after mounting in paraffin. There was no evidence of intraabdominal metastasis. The rest of the operation was uncomplicated. A primary gastric repair was carried out, and finally an open cholecystectomy was performed.
Figure 2: a. Low power view of the frozen section of a prepyloric antral lesion (H&E). HPm: heterotopic pancreatic tissue (mainly ductal) in muscularis propria; HPs: heterotopic pancreatic tissue (mainly acinar and rarely islands of Langerhans) at the serosal site; M: mucosa; ML: mucinous lake; MP: muscularis propria. b. Detail 1 in Figure 2a: pancreatic ducti in muscularis propria at frozen section (H&E). c. Detail 2 in Figure 2a: mucinous lakes which appear to be a perineural invasion of colloid carcinoma at frozen section (ML: mucinous lakes; n: nerve) (H&E). d. Atypical epithelial cells in mucinous material at frozen section (H&E). e. Mucinous lakes did not seem perineural as they did in the frozen section and they were paucicellular in the paraffin section (ML: mucinous lakes; n: nerve) (H&E). f. Mucinous lakes included few cohesive cell groups with suspicious atypia and mucinophages in paraffin section (H&E). g. Positive immunohistochemical reaction with pan-cytokeratin (anti-acidic cytokeratin (AE1) antibody and anti-basic cytokeratin (AE3) antibody) against the epithelial cell group (arrow) (diaminobenzidine chromogen). h. Positive immunohistochemical reaction with CD68 at macrophages (mucinophages) within the same area of Figure 2g.
Histopathological examination of the resected specimen from the stomach revealed a heterotopic pancreas composed of acini, ducts and islets of Langerhans (Heinrich type I) (Figure 2abc). But the mucinous lakes were at a distance from the peripheral nerve (Figure 2e) and showed fewer atypical epithelial cells with macrophages in the paraffin sections (Figure 2f). Actually, the immunohistochemical studies demonstrated that there were many more macrophages than epithelial cells within the mucin lakes (Figure 2gh). Acute or chronic inflammatory cells were not components of the lesion. There were no pancreatic intraepithelial neoplasia- (PanIN) or intraductal papillary mucinous neoplasia (IPMN)-like lesions in the rest of the heterotopic pancreatic tissue.
Pathological examination of the gallbladder showed an intact gallbladder measuring 7 cm in length. Multiple stones were identified and the gallbladder wall had a thickness up to 0.6 cm. Microscopically, it appeared to be chronic cholecystitis with xanthogranulomatous foci. The patient was discharged after an uneventful postoperative course and has undergone follow-up examinations for two years in our clinic.
We wrote this paper as a case report because of the relative rarity of mucinous lesions arising from heterotopic pancreas, and clearly express that we were not able to rule out the diagnosis of mucinous (colloid) carcinoma in the frozen sections of heterotopic pancreatic tissue, but were able to exclude it in the paraffin sections and with immunohistochemical studies. Due to the surgeon’s conservative approach, this situation concluded with only a local excision of the mucinous lesion, and it was possible to avoid a radical oncological surgery.
Frozen examination of mucinous lesions arising from heterotopic pancreas may represent a diagnostic problem. A decision may be very difficult and it is sometimes impossible to decide on the basis of the frozen sections whether the lesion is benign or malignant. Regarding mucinous lesions deriving from heterotopic pancreatic tissue, only one case which had been evaluated with frozen sections has ever been reported in the literature and this was by Nopajaroonsri [10]. In that case report, the author declared a false positive result at frozen section because there was an antral serosal nodule which revealed a pool of mucus containing epithelial clusters and chronic inflammatory cells with no verifiable pancreatic tissue at frozen section. Heterotopic pancreatic tissue was then identified in the mucosa and muscularis propria of the antrum with no evidence of mucinous carcinoma following a distal gastrectomy with omentectomy. Nopajaroonsri classified this lesion as a mucous extravasation nodule resulting from mucus retention in the heterotopic pancreas and expressed the significance of its potential confusion with mucinous carcinoma [10].
In our case, the pathologist saw the heterotopic pancreatic tissue even with the naked eye before the microscopic frozen section examination because of the full thickness wedge biopsy of the prepyloric antrum. The main problem appeared at the serial frozen sections when the pathologist was faced with paucicellular mucinous lakes contiguous to a peripheral nerve. There was no inflammation in the stroma. If it were in the pancreas proper, the lesion would be called “malignant” because mucin leakage into the stroma is an unexpected event in pancreatic tumors and mucin leakage is also more likely to produce an inflammatory reaction than that which occurs with the mucin of invasive colloid carcinoma [11]. Nopajaroonsri reported that mucus retention with the formation of mucous extravasation nodules is a unique and rare complication of heterotopic pancreas [10]. This lesion is characterized by extravasated mucus in a nodule of chronic inflammatory tissue with a few epithelial clusters. The mucous pools in mucinous carcinoma are usually large and infiltrative and show no significant inflammation or fibrosis. Although Nopajaroonsri reported that a mucous extravasation nodule in the heterotopic pancreas must be differentiated from mucinous carcinoma by size, circumscription and tissue reaction, such as fibrosis and inflammation [10], this did not hold true in our case. In our case, the mucinous lakes were not well-circumscribed, appeared to be infiltrating a peripheral nerve and had no significant inflammation or fibrosis. It is a well-known fact that epithelial cells in a mucinous carcinoma may look very innocent and sometimes cannot be found because of paucicellularity. Therefore, one cannot rule out the possibility of a mucinous carcinoma at frozen section examination using these criteria. Our patient’s good fortune was the surgeon’s conservative approach. The surgeon explored the abdomen and decided that there was no other primary tumor. This approach resulted in a wedge gastrectomy with a smaller resection margin, and omentectomy and regional lymphadenectomy were avoided. A second surgery could have been performed if it had proven to be a mucinous or colloid carcinoma.
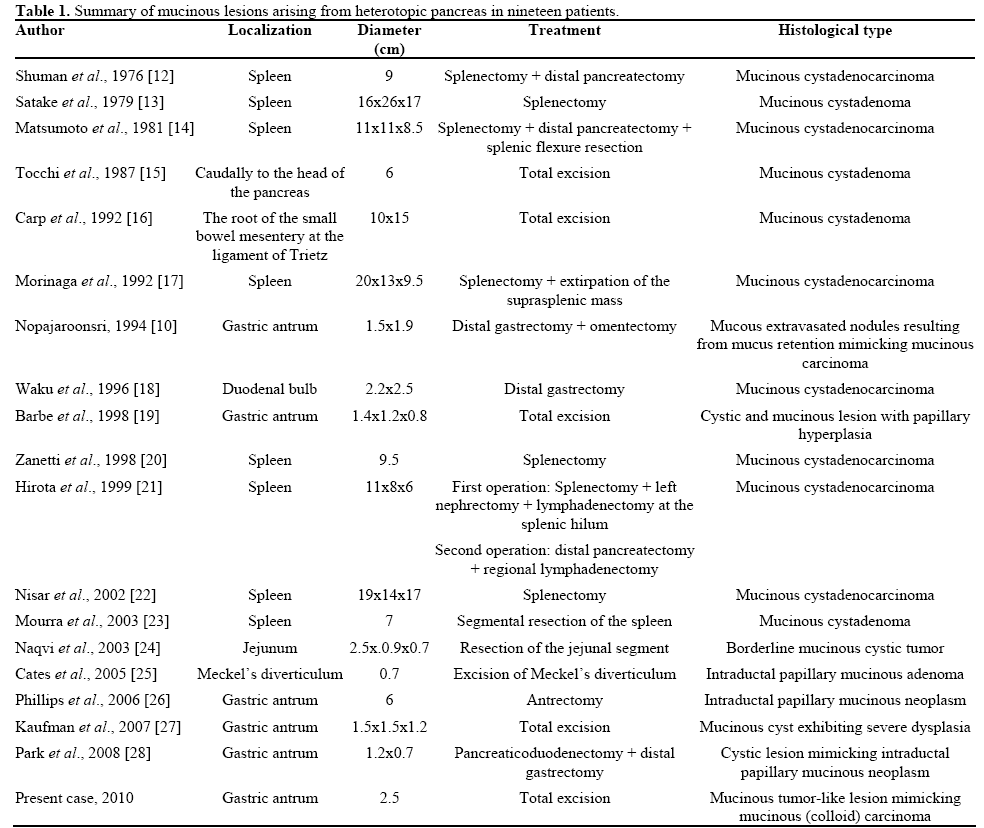
A review of the literature has identified eighteen cases of mucinous-type lesions arising in the heterotopic pancreas as shown in Table 1 [10, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28]. When we reviewed the literature, we found that there were no mucinous (colloid) carcinomas arising in heterotopic pancreas to be found anywhere. Another remarkable finding was the location of mucinous lesions. Only one mucinous cystadenocarcinoma was found in the duodenal bulb [18]. All the other mucinous cystadenocarcinomas arising in heterotopic pancreatic tissue were found in the spleen [12, 14, 17, 21, 22]. Therefore, if one sees mucinous pools or lakes close to heterotopic pancreatic tissue in the wall of a hollow viscus at frozen section examination and if there is no other primary tumor elsewhere in the abdomen, the probability of it being malignant is close to zero. If it turns out to be a mucinous/colloid carcinoma in the paraffin sections, it will be the first one ever reported. The main concern in our case was for the evaluation of the heterotopic pancreatic tissue in the serial frozen sections fearing that it could be a mucinous or other “surprising” lesion and/or tumor. In the literature regarding a carcinoma to be described as arising from heterotopic pancreatic tissue, three criteria have been proposed [29]: i) the tumor must be found within, or close to, the ectopic pancreatic tissue, ii) the nonneoplastic pancreatic tissue must comprise at least fully developed acini and duct structures, and iii) the transition between pancreatic structures and carcinoma must be observed (i.e., duct cell dysplasia and/or carcinoma in situ). In our case, the lesion was compatible with the first two criteria. However, the last criterion, which was not a finding in our case, is also not the case even in the pancreas proper. Tumors of the pancreas proper may not show the transition between the precursor lesions (such as PanINs and IPMNs). Such a situation is rather rare, and it may happen when the tumor is not extensively sampled during gross examination or the precursor lesions are overgrown by an invasive neoplasm. The overwhelming majority of colloid carcinomas in the pancreas and periampullary region arise from preexisting intraepithelial papillary tumor components, including IPMNs, namely, a colloid carcinoma of the pancreas and periampullary region virtually never exists without an associated low-grade papillary in situ component [30]. We estimated that a mucinous (colloid) carcinoma may be within the heterotopic pancreas, and could not be excluded just because those precursor lesions were not seen in frozen section examination.
There is some controversy regarding the pathomechanisms of development of invasive carcinomas derived from IPMNs and the differential diagnostics of mucous leakage and colloid carcinoma. Fukushima et al. described three mechanisms involved in the development of invasive carcinoma associated with IPMNs [31]: 1) penetration of the wall of the duct by neoplastic cells, 2) destruction of the wall of the duct by mucin collecting within the duct which results in increased intraductal pressure and the exiting of neoplastic cells beyond the duct, and 3) disordered polarization of cells leading to the formation of subepithelial mucin droplets which is the first step of muconodular infiltration. The last two mechanisms are typical of colloid carcinoma derived from IPMNs. Small subepithelial mucin droplets accompanying invasive or malignant non-invasive IPMNs, which may represent an early stage of colloid carcinoma development, have been described [31].
Recently, Nara et al. categorized invasive carcinomas derived from IPMNs into four patterns of invasion: infiltrative growth, mucous rupture, expansive growth and intra-abdominal rupture [32]. For the first two patterns of invasion, an additional subclass of “minimal invasion” was specified, based on a threshold of depth of invasion equal to 5 mm. This classification is somewhat complicated since colloid carcinoma may show all four patterns. A distinct category of “minimally invasive” IPMNs described as “mucous rupture” with scanty cancer cells floating in mucin lakes was added. For this type of “non-aggressive” colloid carcinoma, Nara et al. proposed a term of IPMN with “mucous rupture with cellular component”. On the other hand, they proposed a separate group of “aggressive” colloid carcinomas which are characterized by numerous cancer cells in mucin lakes, often accompanied by a tubular invasive component and, more frequently, infiltrating beyond the 5 mm threshold of “minimal invasion” [32].
The observations concerning the relative frequency of duct rupture and mucin leakage in IPMNs are discrepant; some researchers state that this phenomenon is common [33] and others report that it is rare [34]. It is localized only a short distance from the duct, does not usually contain epithelial cells within the mucin pools and is accompanied by an inflammatory reaction. In cases where the epithelium is present, it remains in continuum with carcinoma in situ and has the same cytological features [31, 34, 35, 36]. Acellular mucin pools with no malignant cells should not be considered a diagnostic feature of invasive IPMN [33, 36]. In some situations, the differentiation between large mucin pools and ectatic pancreatic ducts without lining cells may be very difficult [31, 33].
Recently, Stelow et al. identified 42 IPMN cases in their series, and 10 out of 30 IPMNs showed mucus extrusion, not diagnostic of malignancy [37]. They reported that most cases showed cystic pools of mucus in continuity with the intraepithelial lesions. Progressive flattening of the epithelium with a loss consistent with pressure atrophy was often seen, with the mucus penetrating into the adjacent parenchyma in a radiating pattern. Some sections showed isolated, circumscribed mucus pools devoid of epithelium. They suggested that both mucus rupture and duct expansion (‘‘expansive growth’’) associated with pancreatic IPMNs are akin to those features noted with appendiceal mucinous neoplasms and represent phenomena secondary to pressure and not related to the actual malignant characteristics of neoplastic cells.
Molavi and Argani clearly describe two criteria which are crucial for the differential diagnosis between colloid carcinoma and IPMN with duct/cyst rupture: 1) the diagnosis of colloid carcinoma should be based on the presence of clusters (‘balls’) of neoplastic cells located centrally within pools of mucin (in ruptured non-invasive IPMNs, only detached strips of epithelial cells are observed) and 2) mucin or neoplastic epithelium within perineural spaces, outside the pancreatic ductal system or the pancreas itself indicates colloid carcinoma [33].
In our case, the lesion was not compatible with these two criteria since there were no clusters of neoplastic cells located centrally within the mucin pools. Moreover, mucinous lakes were a distance from the peripheral nerve without any invasion into the perineural space and had fewer atypical epithelial cells with macrophages in the paraffin sections. There was no evidence of mucin or neoplastic epithelium invading the extra-heterotopic pancreatic tissue. In addition, immunohistochemical studies demonstrated that there were many more macrophages than epithelial cells within the mucin lakes. Therefore, we felt that this mucinous lesion was not a colloid carcinoma. Most cases of gastric heterotopic pancreas are usually not recognized clinically and their course is generally benign. If the tumor has been recognized preoperatively during endoscopy or endoscopic ultrasound, biopsy should be carried out to establish the diagnosis. If it is impossible to obtain histological confirmation of the nature of the lesion, it is not always necessary to operate. When the lesion is found incidentally during an abdominal operation, its removal is indicated in order to obtain histological confirmation of its character and to obviate the development of clinical manifestations or pathologic changes. Local excision is the most suitable surgical procedure; subtotal gastric resection is best reserved for patients in whom the true nature of the lesion cannot be established and malignancy is suspected.
Asymptomatic lesions of less than 2 cm can be followed without specific therapy [38]. The exception is in a patient with a lesion having a diameter of 2 to 3 cm or greater. If there is tumor having a diameter of 2 to 3 cm, this is smaller than the usual carcinomas for heterotopic pancreas with a gastric location. However, a clinical presentation consisting of epigastric pain, nausea, vomiting and weight loss, and an endoscopy showing an ulcerating or obstructing lesion are more compatible with malignancy. It appears prudent to treat all patients with lesions of 3 cm, even when they are asymptomatic. The occurrence of symptoms, most notably bleeding or obstruction, with lesions under 2 to 3 cm indicate a progression in the size of the lesion or ulceration, and perhaps malignancy. The recommended treatment for these lesions, depending on location, is usually excision by subtotal gastric resection. Local resection should be reserved for small lesions (2 cm or less in diameter) without gross evidence of malignancy [38].
In conclusion, although pancreatic heterotopia is rare, it should always be considered in the differential diagnosis of extramucosal gastric lesions. To the best of our knowledge, our case is the second mucinous tumor-like lesion reported which mimicked carcinoma in heterotopic pancreas of the gastric antrum. We believe that, when paucicellular mucinous lakes containing suspicious atypical floating epithelial cells are seen in the frozen section of such an incidental heterotopic pancreatic lesion smaller than 2.5 cm in diameter, the section must be interpreted cautiously in order to avoid diagnostic confusion and unnecessary radical procedures at the time of surgery. Thus, it is a formidable challenge for both the pathologist and the operating surgeon during intraoperative consultation.
Conflict of interest The authors have no potential conflict of interest