- (2009) Volume 10, Issue 2
Haxiaobieke Kasimu1, Talidao Jakai2, Chen Qilong1, Jiasharete Jielile1
1Department of General Surgery, One-Affiliated Hospital, Xinjiang Medical University. Urumqi, China
2Department of Surgery, Hospital of Habahe County. Xinjiang, China
Received April 22nd, 2008 - Accepted December 30th, 2008
Context An uncomplicated and easy-to-use method of pre-estimating the severity of gallstone pancreatitis shortly after admission was required in order to direct clinicians for monitoring and/or transferring to a specialized center. Objective To determine the role of brief assessment in pre-estimating the severity of gallstone pancreatitis at admission. Patients Fifty-eight patients with gallstone pancreatitis were consecutively followed regarding the course of complications. Main outcome variables Sensitivity analysis of the Biliary Ranson score (>3), the modified Imrie score (>3), the acute physiology and chronic health evaluation II (APACHE-II) score (>5), white blood cell count (>14.5 x103 /dL), blood urea nitrogen (>12 mg/dL), random blood sugar (>150 mg/dL), pulse rate (>100 beats/min) and combinations of the four brief assessments were compared using the z-test. Two-tailed P values less than 0.05 were considered statistically significant. Results Both the Biliary Ranson score >3 and the modified Imrie score >3 had a sensitivity of 96.4% and a specificity of 96.7%. Both the APACHE-II score >5 and random blood sugar >150 mg/dL had a sensitivity of 89.3% which is comparable to a Biliary Ranson score >3 and a modified Imrie score >3. Conclusion As compared to a Biliary Ranson score >3, a modified Imrie score >3 and an APACHE-II score >5, random blood sugar >150 mg/dL can be considered as an oversimplified and effective prognostic indicator at admission in patients with gallstone pancreatitis.
Blood Glucose; Gallstones; Pancreatitis, Acute Necrotizing; Prognosis
The incidence of acute pancreatitis has increased in recent years, and, for the most part, gallstones are responsible for the majority of attacks. Most patients with acute pancreatitis require only a short-term hospital stay and have limited morbidity. However, a few patients with acute pancreatitis will develop a more serious illness, with increased morbidity and mortality. The difficulty in pre-estimating the necessary course of the illness has been well described, and this unpredictability has resulted in the search for more objective methods of identifying the severity.
Numerous scoring systems namely: Ranson criteria [1], a modified Imrie score[2] and an acute physiology and chronic health evaluation II (APACHE-II) score [3] are the recently used prognostic indicators. But 48 h are required to finish the data collection for Imrie and Ranson criteria. The acute physiology and chronic health evaluation II scoring system is more complicated than either Ranson or Imrie, and it is therefore disadvantageous for routine use. There have been studies to find single-value foreseeable indicators in acute pancreatitis such as C-reactive protein, trypsinogen activation peptide, etc.. Much attention has been paid to predicting the severity and clinical course of this entity. The early recognition that a patient with pancreatitis may have gallstone acute pancreatitis is important because these patients may need more aggressive therapy and have more serious complications which require operative intervention than patients with other types of pancreatitis.
In their study, Meek et al. [4] also tried to set up a rapid evaluation for pre-estimating the severity of gallstone pancreatitis.
In this present study, we tried to formulate four brief admission assessments (white blood cell (WBC) count, blood urea nitrogen (BUN) level, pulse rate, and random blood sugar (RBS)) easily available at the time of admission in comparison to APACHE-II, modified Imrie3, or Biliary Ranson scores [5] in pre-estimating the severity of gallstone pancreatitis.
In this prospective study, all 58 consecutive patients admitted for gallstone pancreatitis in the Department of Surgery of the 1-Affiliated Hospital, Urumqi, China, between January 2005 and October 2007 were studied. The diagnosis and severity of acute gallstone pancreatitis was based on the Atlanta criteria. Pancreatitis with an etiology other than gallstones (e.g., alcoholic, idiopathic, drugs, etc.) were excluded from the study. Patients with a previous history of diabetes mellitus were also excluded.
In all cases, a detailed history was recorded. This was followed by detailed comprehensive physical and systemic examinations. Physiological factors and laboratory data were collected on admission and recorded daily.
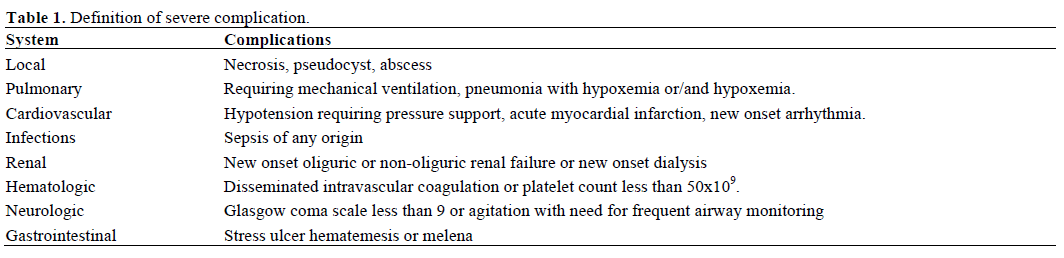
The patients who were enrolled in this study were managed according to recent clinical guidelines and were monitored daily for severe systemic and local complications. Patients developing any of the complications listed in Table 1 were regarded as patients with severe pancreatitis.
Four assessments were considered as prognostic indicators at admission, taking into account the following cut-off values [6]:
• random blood sugar (RBS) greater than 150 mg/dL;
• blood urea nitrogen (BUN) greater than 12 mg/dL;
• white blood cell count (WBC) greater than 14.5x103/dL;
• pulse rate greater than 100 beats/min.
Reference Standards
The APACHE-II [3], the modified Imrie [2], and the Biliary Ranson scores [5] were also calculated using the biochemical and physiological data.
The following cut-off values were taken into account in order to define the reference standards for the definition of severe acute pancreatitis [7]:
• APACHE-II greater than 5;
• modified Imrie greater than 3;
• Biliary Ransons greater than 3.
The sensitivity and specificity of each individual simplified criterion, as well as of combinations of simplified criteria, were calculated in comparison to the reference standards. The comparison of sensitivities among the different variables was carried out by applying the z-test. The comparison of the specificity was also carried out for variables with comparable sensitivity. The z-test compared any two proportions.
All the data were analyzed by SPSS version 11.0 software (SPSS, Inc., Chicago, IL, USA). P values less than 0.05 were considered statistically significant.
Patients were enrolled in the study after obtaining written informed consent, and the study was approved by the Ethical Committee of the Hospital. The study protocol conformed to the ethical guidelines of the "World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects" adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004.
Of a total of 58 patients, 31 (53.4%) were female and 27 (46.6%) were male. The average age of the patients was 48 (range: 24 to 76 years).
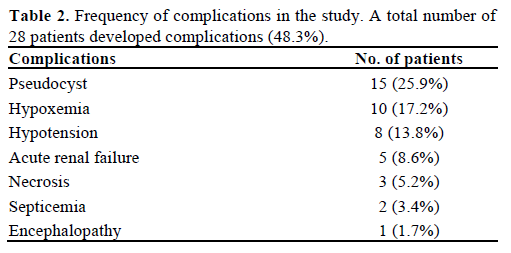
Twenty-eight patients (48.3%) developed complications (Table 2) and were considered to be cases of acute severe pancreatitis; the other 30 patients (51.7%) were considered to be cases of mild pancreatitis. Fourteen patients (24.1%) developed local complications only; of these, 13 patients developed only pseudocysts and one developed necrosis. There was no mortality in these patients. Systemic complications were present in 12 patients (20.7%). Hypoxemia was the most common complication and it was present in 10 cases (17.2%). The total number of mortalities in this study was five (8.6%) and all these patients had multiple organ system failure.
The sensitivities and specificities of the various factors we evaluated are shown in Table 3. Both a Biliary Ranson score greater than 3 and a modified Imrie score greater than 3 had a sensitivity of 96.4% (27/28 patients); each of them did not identify one patient who developed local complications only. Both had a specificity of 96.7% (29/30 patients) and erroneously pre-estimated only one patient as a case of severe attack. They were the most sensitive and specific indicators of severity in this study; an APACHE II score greater than 5 had a sensitivity of 89.3% (25/28) and a specificity of 86.7% (26/30).
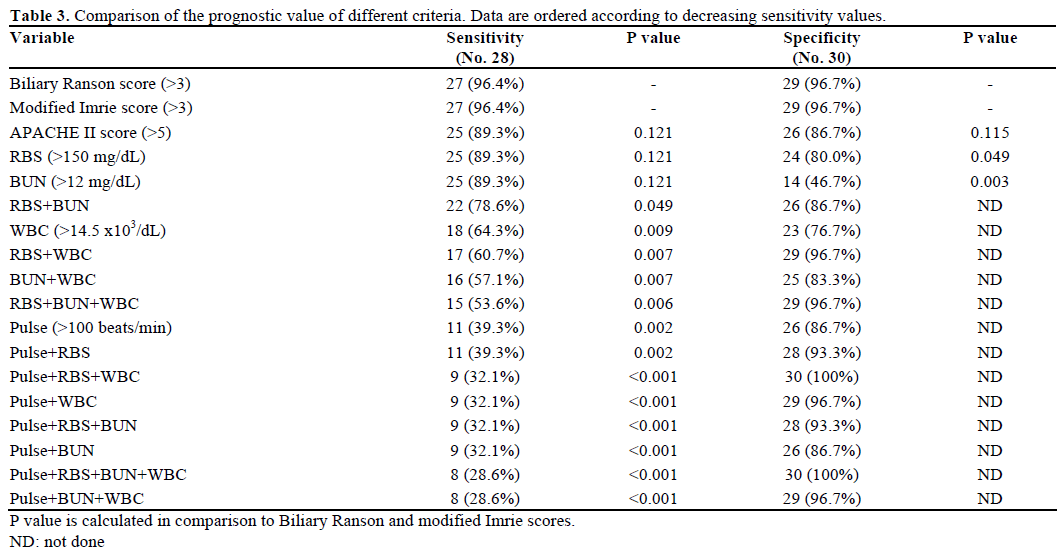
As far as the individual simplified criteria are concerned, the following data were obtained: an RBS level greater than 150 mg/dL correctly identified 25 patients with severe pancreatitis (a sensitivity of 89.3%) with a specificity of 80.0% (24/30); a BUN level greater than 12 mg/dL had a sensitivity of 89.3% (25/28) and a specificity of 46.7% (14/30) and it did not identify three severe pancreatitis patients all of whom developed local complications; a WBC count greater than 14.5 x103/dL had a sensitivity of 64.3% (18/28) and a specificity of 76.7% (23/30); a pulse rate greater than 100 beats/min had a sensitivity of 39.3% (11/28) and a specificity of 86.7% (26/30). The comparison of the prognostic values of all these factors is shown in Table 3.
In spite of the various experimental interventional studies on acute pancreatitis, a more accurate and a brief evaluation of the outcome of acute pancreatitis is still required for physicians.
A pre-estimate of the severity of acute pancreatitis is critical because those with severe disease could be selected for, and may benefit by, prompt intensive treatment. Those with mild disease could be spared from costly and invasive protocols [8] and should be differentiated from those patients who continued to be candidates for organ failure as the illness worsened 48 h after hospitalization, it was regarded as a clinical indicator as were other parameters such as clinical severity, obesity, an APACHE II score greater than 8 (24 h after hospitalization), C-reactive protein greater than 150 mg/L, and a Glasgow score greater than 3. Twenty-eight patients (48.3%) developed complications and were considered to be cases of acute severe pancreatitis; the other 30 patients (51.7%) were considered to be cases of mild pancreatitis [9]. The percentage of severe pancreatitis was higher than the average worldwide record [10]; a possible reason might be that those mild cases who suffered from alcoholic, idiopathic and drug pancreatitis were excluded.
Ranson et al. established 11 objective factors in order to identify severity in patients with acute pancreatitis [1]. Since 69% of these cases were related to alcohol, Ranson revised the criteria for patients with biliary pancreatitis [5]. Imrie modified Ranson’s prognostic scoring system and reduced the factors to nine [11]. Buter et al. modified the Imrie criteria by deleting the age factor [12]. Blamey et al. also modified the Imire criteria by including the age factor and deleting transaminase [2]. The acute physiology and chronic health evaluation II system of disease severity assessment was developed by Knaus et al. [3].
There were a number of disadvantages associated with these scoring systems. Taylor et al. [13] suggested that the number of patients with gallstone pancreatitis in the Ranson study of 1982 was inadequate (70% were again of alcoholic origin) to be used as an accurate prognostic scoring system and APACHE-II is disadvantageous in routine use by reason of its complexity. Harrison et al. [14] suggested that the initial clinical evaluation could not assess accurate severity and stage of disease after only 24 h of hospitalization in the majority of cases. Instead, further assessment within 48 h after hospitalization is indispensable because it improves the accuracy of determining severity of this disease, while most of parameters corresponding with gallstone pancreatitis might be consist with multiple evaluation systems such as Ranson and APACHE-II.
Some authors believe that multiple scoring systems have too many values to be memorized and need 48 h for evaluation; therefore they result in a severe loss of the most crucial investigative and interventional time; in addition, the fact that the parameters might be influenced by treatment during the 48 h should be taken into account [15].
Other authors have previously reported the value of a simplified prognostic assessment of acute pancreatitis. High plasma glucose is an indication (feedback) of the severity of damage to islet cells [16]. Mentula et al. [17] showed that acute pancreatitis was related to deficient beta-cell function and decreased glucose tolerance. These studies suggest that higher RBS levels may call attention to more severe damage to the pancreas and that RBS could be used as a prognostic indicator.
Gan and Romagnuolo [18] demonstrated that an admission urea level exceeding 8.6 mmol/L was related to a mortality rate of 49%. Some authors considered that an elevated urea level indicates hypoperfusion, which may bring about the development of pancreatic necrosis [19]. Another study showed that an elevated serum urea level could be a reflection of poor renal reserve, hypovolemia, or gastrointestinal bleeding making these patients more susceptible to complications [20].
In a study of Ueda et al. [21] the sensitivity and specificity of a combined serum glucose level greater than 11.0 mmol/L (200 mg/dL) and/or a BUN level greater than 7.4 mmol/L (20 mg/dL) were 75% and 80%, respectively and this combination was comparable to the Imrie scoring system. Company et al. [22] later reached their findings of the earlier study by using the same cut-off values of serum urea/plasma glucose criteria. Sensitivity was 79% and specificity was 67% which were comparable to the APACHE-II, Ranson, and Imrie scoring systems. These findings point out that higher serum glucose and blood urea levels correlate with the severity of pancreatic insult and that they might be used as prognostic indicators. Meek et al. [4] researched the prognostic value of simple admission criteria (WBC greater than 14.5 x 103/dL; BUN greater than 12 mg/dL; RBS greater than 150 mg/dL; pulse rate greater than 100 beats/min) and compared them with an APACHE-II score greater than 5, a Biliary Ranson score greater than 3, and a modified Imrie score greater than 3. They demonstrated that an admission value of RBS greater than 150 mg/dL had a sensitivity of 82% and a specificity of 85% in patients without diabetes, and it was the best single pre-estimator of severity. They also confirmed that it was less cumbersome than scoring systems and allowed immediate triage to the appropriate level of hospital care.
The establishment and conclusions of our study were based on the clinincal data of gallstone pancreatitis after exclusion of diabetes mellitus. In our study, both an RBS level greater than 150 mg/dL and a BUN level greater than 12 mg/dL had a sensitivity of 89% which was comparable to an APACHE-II score greater than 5, a Biliary Ranson score greater than 3 and a modified Imrie score greater than 3. BUN greater than 12 mg/dL had the disadvantage of a very low specificity (47%), being significantly lower than that of a RBS level greater than 150 mg/dL (80%), which led a large number of mild attacks to be graded as severe.
A level of RBS greater than 150 mg/dL at admission can be regarded as an indicator to the clinician of the high possibility of the patient of developing severe complications and requiring a more intensive monitoring. However, this does not indicate any change in the clinical guidelines for the initial management of acute pancreatitis. Repeated clinical detections and monitoring of baseline parameters in the initial 72 h should also be carried out because it enables the clinician to identify which patients will develop complications
This study confirmed the findings of Meek et al. [4] and we can conclude that an RBS level greater than 150 mg/dL can be used as a uncomplicated prognostic indicator as it is simple to use in both rural and urban settings, is readily available at admission and allows rapid evaluation of severity.
The authors have no potential conflicts of interest