Chiara Tosin1, Amabile Bonaldi2,Lea Dell’orletta2, Riccardo Sartori3 and Paolo Biban2
1 Department of Philosophy, Education and Psychology, Pediatric Department, University of Verona, Integrated University Hospital of Verona, Italy
2 Pediatric Department, Integrated University Hospital of Verona, Italy
3 Department of Philosophy, Education and Psychology, University of Verona, Italy
*Corresponding Author:
Chiara Tosin
Department of Philosophy, Education and Psychology, University of Verona, Pediatric Department, Integrated University Hospital of Verona, Italy.
Tel: +393922083292
E-mail: Chiara.tosin@aovr.veneto.it
Received Date: March 17, 2017; Accepted Date: March 20, 2017; Published Date: March 27, 2017
Citation: Tosin C, Bonaldi A, Dell’orletta L, et al. Zinc Oxide 30% and Tocopherol Compared to 10% Zinc Oxide Ointment in the Treatment of Infant’s Diaper Dermatitis: A Triple Blinded Controlled Randomized Trial. Clin Pediatr Dermatol. 2017, 3:1. DOI: 10.21767/2472-0143.100024
Keywords
Nursing; Dermatitis; Diaper; Napkins; Neonate; Infant; Zinc oxide; Tocopherol; Rush; Skin
Introduction
Background
Diaper rash or diaper dermatitis (DD) is the most common skin disorder that occurs during early childhood [1], reaching its peak at an age between 6 and 12 months and with a variable frequency between 25-65%. An American study carried out on 8.2 million patients, showed one in four chance of an infant being diagnosed with DD [2]. There is no specific definition of this dermatitis involving the perineal-gluteal region [3]. Typical symptoms are the abrasion erythematous lesion, able to cause pain because of the potential involvement of the affected nerve endings. The etiology is still not fully known, although it certainly appears to be multifactorial. In the factors involved in its pathogenesis, an important role is attributed to the prolonged contact with urine and feaces and the occlusive effect of the diaper, which induce maceration and irritation of the skin [4]. The skin plays a biological role as interface between the body and the external environment, and from a neonatal age stands as a barrier to chemical, physical, radiating, infectious and mechanical insults that come from outside [5]. Most of these infectious, chemical, or physical insults act by triggering an oxidative reaction provoking skin damage from the release of free radicals and the consequent erythema, edema, abnormal keratinization, and skin aging. In normal intact skin, the barrier function is composed of two structures: the first is the stratum corneum, the outermost layer of the epidermis which is fundamental in order to reach an adjustment of transcutaneous water loss (TEWL); the second is a hydro-lipid film that covers the skin by acting as a natural physiological emollient and maintaining a stable pH between 5 and 6.5.
The moist environment under the diaper makes the skin more susceptible to infection with microorganisms, which exacerbates the condition and may lead to mycosis [6]. In multiple clinical studies, mycosis has been isolated in up to 80% [6] of children with DD which can be present for even three or more days [7]. Once the stratum corneum has been damaged the skin is more vulnerable to secondary infections by bacteria and fungi. Ferrazzini [7] found that colonization with Candida albicans was significantly increased in children with symptomatic diaper rash. A wide variety of other infections has been reported but it appears that Candida is the most common opportunistic invader in diaper areas. To treat skin infections and mycosis, many topical drugs are used. Ward [2] studied medications to treat DD in the United States, they founded that Nystatin was the leading treatment agent prescribed (27%), followed by clotrimazole (16%), a combination product of nystatin and triamcinolone (16%), hydrocortisone (8%), and a combination product of clotrimazole and betamethasone dipropionate (6%) Ward [2]. Other authors, as [8], tested the efficacy of antifungal medications. They enrolled 201 patients in the study. 101 were treated with miconazole nitrate.
over the years, many treatments for diaper rash have been tested, with different results. Currently great importance is given to the type of used diapers and hygiene of the skin. It is suggested that the quality of the diapers and the frequent replacement of the diaper can decrease the occurrence of maceration and therefore, the incidence of diaper dermatitis (DD)i. In the mid-80s the Berg's study defined over hydration and the increased susceptibility to friction and contact with urine and feaces as some of the most responsible elements for the cascade of inflammatory events causing dermatitis. Usual therapeutic options consist of frequent diaper changes, regular cleansing of the skin and application of fluid absorbing ointments and pastes. Ointments, which may contain zinc oxide, are recommended as a base-line therapy [9]. Subsequent studies have demonstrated the effectiveness of using diapers with a continuous release of a combination of zinc oxide and petrolatum [10,11]. In the literature, the properties of tocopherol have been analyzed many times in the treatment of skin diseases in the newborn, and in the treatment of surgical wounds with pre and post-surgery administration either as regards the management of lesions or the maceration of the skin due to the rubbing on the surface of the diaper or to stagnation of material such as feaces and urine in the most prone area to the onset of dermatitis [12].
Aim of the Study and Research Hypothesis
The purpose of this triple blind randomized clinical trial was to test the effectiveness of a 30% zinc oxide-based product and tocopherol/Vitamin E acetate pure (Ingredients: Tocopheryl Acetate, Zinc Oxide, Cyclopentasiloxane, Hydrogenated Castor Oil, Ethylhexyl Palmitate, Dymethiconol) in comparison with the most widely used product for the treatment of diaper dermatitis, the 10% ointment zinc oxide [13].
The primary aim of the study was to evaluate the efficacy of 5 days of the experimental treatment by using the paste of Zinc Oxide 30% and tocopherol/Vitamin E acetate pure compared to the use of a 10% Zinc Oxide ointment in the treatment of diaper dermatitis affecting the newborn's skin and the premature infant with gestational age ≥ 34 weeks. The study secondary aim is to assess the proportion of cases with complete recovery on the 5th day of treatment. It was expected no difference in the efficacy of both the treatments in reducing the time of recovering from DD.
Methods
Design
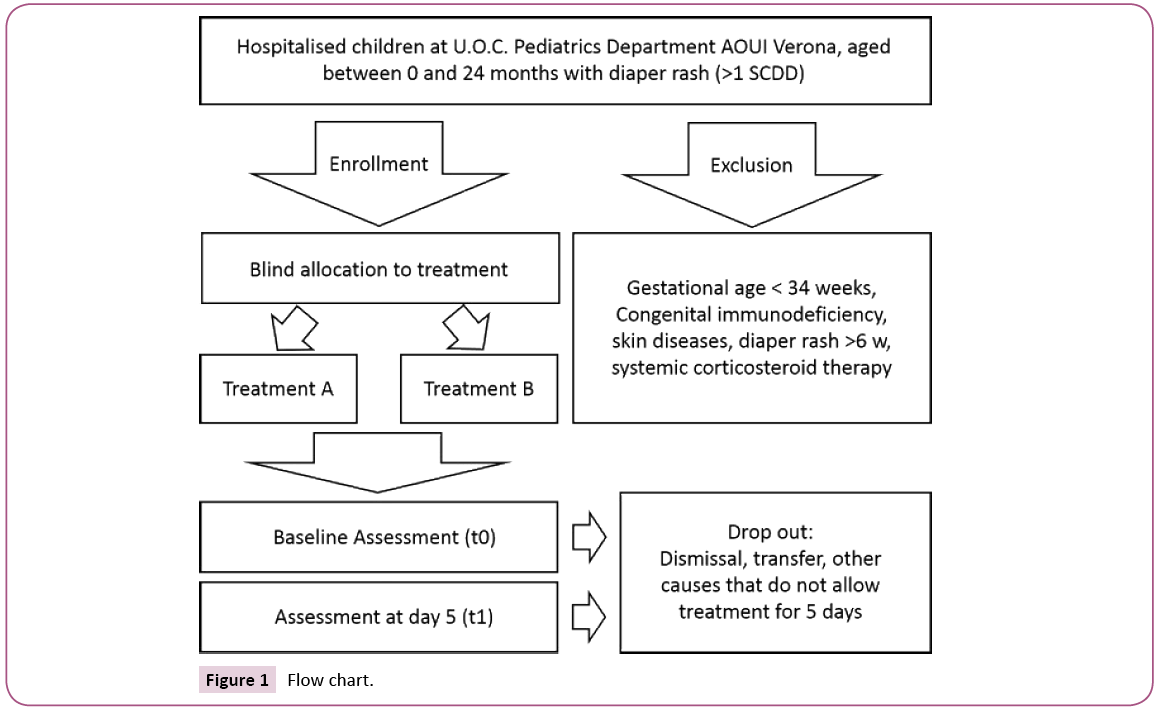
This was a triple-blind controlled trial (EudraCT, 2012-003567- 22), patients 0 to 24 months were randomized to receive Zinc Oxide 30% and tocopherol / Vitamin E acetate pure, Vea Zinc® or Zinc Oxide 10% ointment for 5 days. Eligible participants were all children aged 0–24 months admitted to the Pediatric department of Borgo Trento University Hospital in Verona, especially in the pediatric intensive care, pediatric ward and neonatal care, between March 2013 and August 2015. All infant with minimal severity diaper rash, score 1 according to the scale "Severity Classification of Diaper Dermatitis" (SCDD) [14] met the inclusion criteria. Patients were excluded if they suffered either from chronic DD persisting for longer than 6 weeks or from concomitant skin diseases (e.g. psoriasis, perianal streptococcal dermatitis, congenital warts, allergic contact dermatitis) which could have interfered with the assessment of DD. Preterm less than 34 weeks of gestational age, newborns with congenital immune deficiency, children with other concomitant skin diseases (psoriasis, epidermolysis bullosa, mycosis) and patients receiving systemic corticosteroids at enrolment were also excluded from the study. Patients dismissed or transferred before the 5th day after starting treatment with other UO were considered drop out.
At the recognition of diaper rash with a minimum severity score 1 according to the scale "Severity classification of diaper dermatitis" the consent to participation in the study was collected from parents of patients who met the inclusion criteria. Enrolled patients were then randomized to one of two treatments and became part of the study. The two groups of patients were administered respectively: pasta Oxide 30% Zinc and tocopherol/ Vitamin E acetate in a pure state in the experimental group and a 10% Zinc Oxide Ointment to the control group. Nurses were trained with specific courses both in the design of the study (design, objectives, methods, and evaluation) and on patient management mode. At each diaper change one of the two treatments were administered by the nurse who was in charge of the patient. The cleansing of the skin during the diaper change, was performed only with running water through spray (when possible) or otherwise using a soft, free of drugs material such as cotton soaked in warm water. The procedure was performed by dabbing the skin. When it was necessary to remove dry stool or meconium a small amount of Vaseline oil was added. The product was applied to clean and dry skin. The unit of measure used for administration of the treatment was the finger unit (the quantity of product corresponding to the phalanx of a finger is sufficient to treat a skin surface corresponding to the palm of the operator's hand).
To evaluate the efficacy of the experimental treatment we compared the SCDD score and its improvement from baseline in the two groups. Percentage of cases with complete healing (0 of the scale value) on the fifth day was calculated and compared between the two groups of treatment. Data collection. The sample size was calculated assuming a difference between the two treatment groups of 25% with a power of 80% and a significance of 5%, in less favorable assumptions that the percentage in the treatment group with only zinc oxide is equal to 50%. With these hypotheses, the number of patients to be recruited amounted to a total of 128 (64 cases per treatment group). A simple randomization in a 1:1 ratio to the two treatments was followed. Patients were randomized after enrolment in a chronological order through random assignment with a list created with the PASS11 software. The randomization list was kept in the biostatistics and AOUI Verona research support office archive. It contained the association between patient identification and treatment assigned. A password protected copy of that list was provided to the pharmacist of the company that ensured the preparation of the correct products. A "blinded" copy of the list was provided to the statistician who has processed the data associating the generic treatment ID (1 or 2). After verification of inclusion criteria, the nurse who was in charge of the patient was responsible for informing parents and obtain the consent to data processing. Subsequently picked up the progressively numbered envelope from the delivery authorized officer and associated the ID code of the envelope to the patient. None of the operators were aware of the assigned treatment. Only the numerical code randomly identified by the randomization list could determine in the process of elaboration of the data, what were the patients treated with either one or the other product. Envelopes with the treatment material were kept in a safe place and delivered by an authorized administrator. Once an envelope was selected and given to the patient, the nurse compiled and placed in the folder the forms (CRF and prepared the material needed for the treatment to the patient in his/her bed). The patients were assessed at enrolment and after 5 days of treatment. The two products were prepared in containers identical in shape, size and color. The preparation of the products was supervised by one of the company's pharmacists which ensured the correct preparation of the product. The products were in any way not identifiable without the randomization list. The treatments had the same color and compactness, and, despite one being a paste and the second being an unguent, these were characterized by an identical tactile consistency. The assignment took place in chronological order with respect to enrolment according to the scheme provided by the spreadsheet. The randomization list was kept on a password-protected spreadsheet. This list contained the patient's numeric identifier not attributable to the type of treatment given. The personal data (ID, birth date, age, date of acceptance, weight, diagnosis, department, administration of antibiotics, diet, bowel function) and data related to enrolment (dermatitis measurement on the scale of severity at enrolment and at time 0) were collected at the enrolment of the patient. Patients were assessed at baseline (time 0) and on the fifth day post-treatment (time 1) following the SCDD. Information was collected on pre-printed paper forms and then inserted in a specific electronic database. The percentage of patients estimated drop-out, based on the literature data, was around 30%.
Statistical analysis
Statistical analyses were performed by using SPSS 19. In order to compare population and treatment efficacy t-test and ANOVA were performed. A p<0.05 was considered statistically significant. Both targets were evaluated on the population "per protocol”: the population that did not meet the major protocol inclusion criteria such as the transfer and / or discharge before the 5th day of assessment was excluded. Only at the end of the statistical analyses, the statistician was made aware of the correspondence between the treatment number (1 or 2) and the type of treatment (zinc oxide associated or not to Tocopherol).
Results
All the patients were enrolled in the Pediatric department of Borgo Trento University Hospital in Verona. In the study period 180 patients were enrolled: 90 were assigned to the treatment group, 90 to the control group. 169 patients completed the study (n=85, n=84), 3 patients were discharged before the observation period, 5 patients withdrew due to willingness of physician, 1 patient died. In 2 cases the product was finished before the study ending) (Figure 1). Samples were considered comparable since there were no statistically significant differences for the variables: age, sex, disease, anthropometric measurements, diet, skin. At baseline the study population was almost evenly divided 85% (n=143) between slight rash and mild rash, and 15% (n=25) between moderately severe rash to severe rash, SCDD score at time 1 was similar in the two groups of treatment (p<0.05). No difference, with respect to demographic and clinical analyzed variables, was found between the SCDD score at time 0 and time 1 (p>0.05). Children with a neurological co-morbidity at admission had worst scores at time 1 respect to other co-morbidities. Although the SCDD score was clearly decreased in both groups by the end of trial F (3.139)=4.091, P< 0.01) (Table 1), there was not a statistically significant difference between groups as determined by ANOVA F (2.164)=0.151, p=0.860 (Table 2) There was not any adverse effect from either of the study products. 45% (n=75) of children experienced a complete heeling at time 2,91,7% (n=155) had an overall reduction of SDCC score and 14 patients (8.3%) had worse score at time 2 in all the comparison without any difference between the two groups of treatment. Respect to comorbidities, children with neurological impairment had the worst score at time 1 but the better improvement over time (p=0.01).
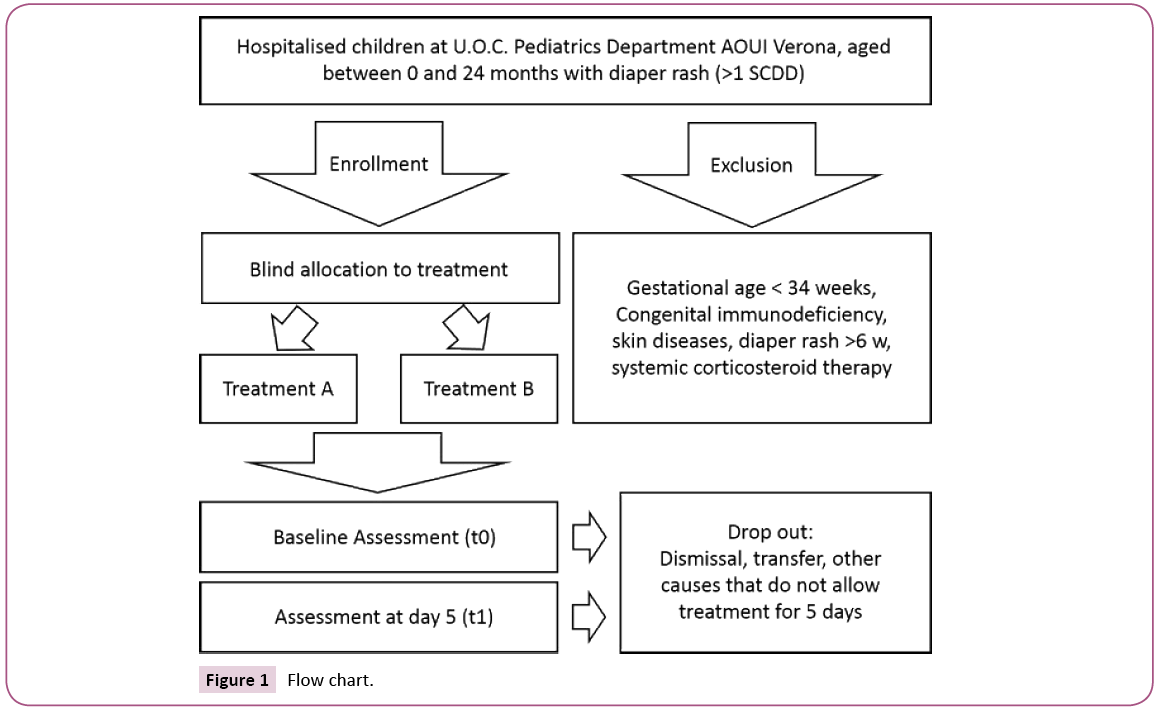
Figure 1: Flow chart.
| |
Sum of squares |
Df |
Mean square |
F |
Sig. |
| Between groups |
19.548 |
3 |
6.516 |
4.091 |
0.008 |
| Within groups |
221.389 |
139 |
1.593 |
| Total |
240.937 |
142 |
|
Table 1: ANOVA 1.
| |
Sum of squares |
Df |
Mean square |
F |
Sig. |
| Between groups |
0.536 |
2 |
0.268 |
0.151 |
0.86 |
| Within groups |
291.883 |
164 |
1.78 |
| Total |
292.419 |
166 |
|
Table 2: ANOVA 2.
Discussion
Diaper dermatitis, an acute inflammation of the skin in the diaper area, is the most common dermatologic disorder on infants [9]. DD makes the skin more susceptible to infection with microorganisms and may lead to mycosis [6]. Dixon et al. isolated C. Albicans from the skin of 41% of patients [15] the severity of diaper rash was founded significantly and positively associated with C. Albicans quantity [9]. Many products based on zinc oxide were studied for a safe and effective treatment for diaper dermatitis, the efficacy and safety of these products in DD were assessed on several times [13]. Not all patients respond equally to skin protective agents, and when DD is present for more than 72 hours’ colonization plays a more important role in the pathology [1,16]. According to literature [7,8] a department internal research confirmed 80% DD frequency on population. Nitzan and Cohen [17] said that there was a very little evidence demonstrating convincingly the efficacy of zinc as a first-line treatment for any dermatological condition, furthermore many authors highlighted the correlation of colonization and DD patients [10]. On this basis, further studies were carried out to evaluate the efficacy of different antifungals paste. In this randomized triple blinded controlled study, we compared two oxide based products commonly applied in DD: 30% zinc oxide in association with tocopherol ointment and 10% zinc oxide ointment. At the end of the trial 169 infants were enrolled, 45% of patients (n=75) showed a clinical complete heeling while 91,7% of patients (n=154) showed a total reduction of SDCC score. During the research period, there were not colonization onset without significant difference between groups about this. In conclusion, there was no difference in time of heeling or in colonization onset on the comparison of both the products.
Conclusion
Author’s first consideration is about the efficacy of trial medications. Both the ointments exerted a comparable beneficial effect in DD patients which might be attributable to the respective formulation. Despite the different composition both the products guaranteed effective action on dermatitis. Boiko [18] supposed a high correlation between DD management and the decreasing of SCDD score, his study however does not show any significant result regarding the efficacy of moistures. Other authors considered the importance of management on prevention and treatment of DD [19]. Consideration on the relevance of management procedures or medications composition can be made also on the basis of this study’s results. Another authors’ consideration is about the frequency of colonization. [20] define mycoses as the major complication in DD patients. Usually 5 days treated DD without reduction of SDCC is considered as mycoses [21]. During this study, no patient was diagnosed as colonized. Moreover, for all the period of the study, no one antifungal paste was bought by the department (verified with medication computerized system). Both the ointments seem to have an efficacy in reducing the onset of colonization. Not only are management procedures more important than the composition of zinc oxide products but also, they have a role on the colonization prevention. The results of this triple blinded randomized trial confirm the protocol evidence based development as necessary. In conclusion, management of napkin change timing (more frequent in high risk patients), method of cleaning (running water or cotton soaked in warm water to dab the skin without rubbing), method of applying product (to clean and dry skin) and quantity for administration (finger unit) have high impact on DD healing rates and on colonization onset rates. During all the period of the study, no one antifungal paste was bought by the department (verified with medication computerized system). The study was approved by the ethics committee of AOUI of Verona (CE 2247). All parents received oral and written adequate information on the study, and a special form for the expression of their informed consent has been given to them. The study was conducted according to the principles enunciated in the Declaration of Helsinki [22] and Good Clinical Practice [23]. There were no financial arrangements related to the design and conduct of the study. Insurance cover for subjects included in the study was that of AOUI of Verona.
Relevance to Clinical Practice
Diaper Dermatitis is actually the most common disease that occurs during the early childhood. At home parents use a lot of different paste to attend this disease and in the hospital, there are high levels of over colonization.
Different Oxide zinc pastes have similar results on Diaper Dermatitis, protocols and procedures in management of diaper dermatitis can have a relevant role on the heeling rates. Protocols and procedures in management of diaper dermatitis can have also a relevant role on the prevention of colonization.
The knowledge of medications efficacy can help in reduction of waste and costs, and can reduce the colonization onset.
Trial Registration
EudraCT Number: 2012-003567-22; Sponsor's Protocol Code Number: Zincox12; National Competent Authority: Italy - Italian Medicines Agency; Clinical Trial Type: EEA CTA.
References
- Atherton D (2016) Understanding irritant napkin dermatitis. International Journal of Dermatology 55: 7-9.
- Ward D, Fleisher A, Feldman S(2000) Characterization of diaper dermatitis in the united states. Arch Pediatr Adolesc Med154: 943-46.
- Davies M, Dore A, Perissinotto K(2005) Topical Vitamin A, or its derivatives, for treating and preventing napkin dermatitis in infants. Cochrane Database of Systematic Reviews, Volume 4.
- Boiko S(1999) Treatment of diaper dermatitis. Dermatol Clin17: 235-240.
- Bibi NY, Cohen A(2006) Zinc in skin pathology and care. J Dermatology treat 17:205-210.
- Eichenfield L, Bogen M(2007) Absorption and efficacy of miconazole nitrate 0,25% ointment in infants with diaper dermatitis. Journal of drugs in dematology.
- Bonifaz A(2013) The efficacy and safety of sertaconazole Cream (2%) in diaper dermatitis candidas. Mycopathologia175:249-254.
- Ferrazzini G., Kaiser R, Cheng SH (2003) Microbiological aspects of diaper dermatitis. 48:385-388.
- Concannon P, Gisoldi E, Philips S, Grossman R(2001) Diaper dermatitis: a therapeutic dilemma. Results of a double-blind placebo controlled trial of miconazole nitrate 0.25%. Pediatric Dermatolog 18:149-155.
- Atherton D (2004) A review of the pathophysiology, prevention and treatment of irritant diaper dermatitis.Curr Med Res Opin 20: 645-649.
- Hoeger P, Stark S, Jost G (2010) Efficacy and safety of two different antifungal pastes in infants with diaper dermatitis: a randomized, controlled study. JEADV24:1004-1008.
- Zampieri N(2010) A prospective study in children: Pre- and post- surgery use of vitamin E in surgical incisions. Journal of Plastic, Reconstructive and Aesthetic Surgery 63:1474-1478.
- Thiele J (2001) The antioxidant network of the stratum corneum. Curr Probl Dermatol29:42.
- Gelmetti C(2001) vitamina E topica in dermatologia pediatrica. In: Ursini F, Caputo R (eds.), Vitamina E in Dermatologia. Padova. University Publisher.
- AradA (1999) Efficacy of topical application of eosin compared with zinc oxide paste and corticosteroid cream for diaper dermatitis. Dermatology 199: 319-322.
- Berg R, Bukingham K, Stewart R (1986) Etiologic factors in diaper dermatitis: the role of urine.Pediatr Dermatol 3:102-106.
- Dixon P, Warin R, English M (1972) Alimentary Candida albicans and napkin rashes.Br J Dermatol86: 458-462.
- Hoeger P, Stark S,Jost G(2010) Efficacy and safety of two different antifungal pastes in infants with diaper dermatitis: a randomized, controlled study. Journal of the european academy of dermatology and venereology 24:1094-1098.
- JannigerC, Thomas I (1993) Diaper dermatitis: an approach to prevention employing effective diaper care. Cutis 52:153-155.
- Klunk C, Domingues E, Wiss K (2014) An update on diaper dermatitis. Clinics in dermatology32: 477-487.
- Leyden J, Kingman A(1978) The role of microorganism in diaper dermatitis. Arch Dermatol114: 56-59.
- Merril L (2015) Prevention, Treatment and parent education for diaper dermatitis. Nursing for women's health19: 324-337.
- Nachbar F, Korting H (1995) The role of vitamin E in normal and damaged skin. Journal of Molecular Medicine73:7-17.