Keywords
Obstetrics; History; Neuraxial anesthesia; Labor analgesia
Introduction
“Take a deep breath, hold, and push…”
This paints a picture of a woman just about ready to bring a new
life into the world. Yet such a wonderful childbirth experience can
bring one memories of pain, fear, and joy all packaged into one.
Childbirth is an experience that is both exciting and painful for
every woman. This is a review of the development of obstetric
anesthesia and puts in perspective the history of obstetric
anesthesia in both the western and eastern medicine, and how
each has contributed to the other.
Methods and Design
In western medicine, the introduction of modern anesthesia in
obstetrical practice has been credited to Sir James Y. Simpson
who used ether in childbirth on January 19th of 1847. A few more
attempts led him to chloroform which was found to be stronger
and better than ether [1]. By the turn of the 20th century, ether
and chloroform were ubiquitous in childbirth on both sides of the
Atlantic Ocean [2]. Despite this medical breakthrough, however,
the British criticized that ether and chloroform not only increased
the risk of hemorrhage and infection but had detrimental effects
on the newborn [3]. Some would argue that the pain of childbirth
was inseparable from the function of the uterus, and to suppress
that pain would inhibit labor [4]. Still, others would argue that to
relieve pain during childbirth was to counter the biblical teaching
that women would suffer in childbirth after Eve’s sin and that
anesthesia would open the door to unnecessary procedures
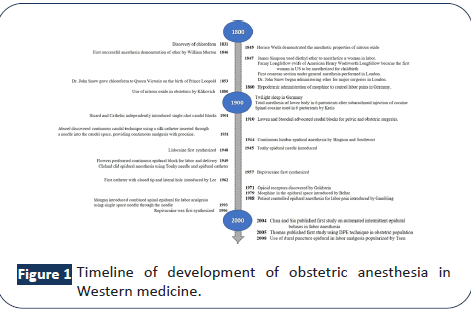
without the patient’s consent [4]. Figure 1 shows a timeline on
the development of obstetric anesthesia in the western part of the globe.
Figure 1: Timeline of development of obstetric anesthesia in
Western medicine.
Eastern medicine dates back to as early as the 3rd century BCE.
Countries like China, Japan, Philippines, and India have pain-
relieving drugs as evidenced by their extensive botanical resources
and writings dating back to the ancient times. However, despite
this wealth of knowledge, anesthesia has not flourished as much
to this day without western medicine influx to these countries.
Medicine in China is of great antiquity that relies in the dualistic
cosmic theory of yin and yang. Anesthesiology, however, was
brought to imperial China only when it opened its doors for trade
and evangelism. Dr. Rev. Peter Parker introduced ether anesthesia
into China a year after it had been publicly demonstrated in
Boston and then subsequently used chloroform anesthesia after
it was introduced by Simpson. After this momentous occasion,
medical education commenced in China with the establishment
of its first medical school. Pre-world war II anesthesiology in
China kept pace with its American and European counterparts.
Subsequent anesthetics introduced in the US were reviewed pharmacologically in China and the Chinese manufactured their
own anesthesia machine in the 1930s [5,6]. The nongovernmental
No Pain Labor and Delivery (NPLD) was launched in 2008 with
the goal of improving labor outcomes in China by increasing the
absolute labor epidural analgesia rate by 10% by establishing
10 training centers over a 10-year period. It also involves 24/7
obstetric anesthesia coverage in Chinese hospitals through
education and modeling multidisciplinary approaches [7].
Despite this undertaking, the rate of cesarean delivery in 2010
escalated to greater than 8.2 million deliveries annually, with
at least 12% were maternal request, mostly due to fear of
labor pains or analgesia failure [7]. In 2011, the Chinese Society
of Anesthesiology (CSA) established the obstetric anesthesia
committee, involving many experts to set up standards, guidelines
and consensus and designate training sites in mainland China [8].
In 1804, Dr. Hanaoka introduced anesthesia in early Japan 40
years before Morton’s use of ether anesthesia. He synthesized
the drug, Tsusensan, consisting of 6 medicinal herbs, with Datura
alba (Mandarage) as its main component. This Mandarage will
be known later to contain scopolamine. Labor analgesia was
attempted as early as in the Meiji period (1868-1912) with the
use of pantopon, an opioid with less respiratory depression
than morphine. Inhalational anesthesia using chloroform was
administered for cesraean delivery up to 1897 [9]. It was not
until postwar; however, that evolution of anesthesiology in Japan
progressed rapidly when doctors from the United States came to
Japan in 1950 to help reform Japanese medical science with the
subsequent establishment of the Japanese Society for Anesthesia
[9].
The richness of Indian culture combined with religion and
traditions have impacted their practice of medicine and healing
that led to the modern era. India boasts of significant contributions
to the development of anesthesia, dating from the pre-ether era
describing surgery using opium, wine, and Indian hemp in 500
BCE. The first administration of ether anesthesia in India was in
1847 in Calcutta, just five months after demonstration of ether
anesthesia in Boston. Chloroform was first administered in India
in 1848, barely 3 months after it was first used by Simpson [10].
Despite these advancements, culturally speaking, intense pains
are thought to be necessary to ensure a speedy delivery, thus
no remedies for reducing labor discomfort is given. Women are
considered shameless if they make noises audible to people
outside the room. The laboring woman’s silence is considered
very important in other parts of South Asia as well [11]. A crosssectional
study conducted in a tertiary care hospital in South
India in 2017 among 100 parturient showed that only 14% of
pregnant women were aware of labor analgesia. Majority of the
subjects would opt for a safe and effective labor pain relief but
its proportion has dropped to 55% when mentioned that costs
go up to 30% to 40% [12]. In other study involving 1000 full-term
pregnant women in rural India, only 33% had knowledge about
labor analgesia. When given full information about labor analgesia options, the main reason of refusal among 69% of these patients
dated back from childhood, when they were taught that they
have to undergo labor pains, and that it is mandatory to endure
the pain of childbirth. Socioeconomic status, lack of teaching, low level of practical exposure, and prevailing confusion/ignorance
about labor analgesia benefits as well as education status all
seem to be the biggest hurdles toward acceptance of pain relief
during childbirth [13].
During the precolonial period folklore medicine practices were
the cornerstone of medicine in the Philippines. Traditional ways
of healing include rituals and herbs with a Babaylan, a female
healing leader. From among the traditional healers came the hilot
which means “massager” or a “folk midwife” and the modern day
Traditional Birth Attendants (TBA) [14]. Despite having extensive
herbal medicines as documented in various writings by Spanish
friars, it was not until the beginning of the nineteenth century
which marked the end of the Galleon trade in 1820s and the
opening of the Suez Canal that has paved the way to western
medicine [15]. Towards the end of the 19th century, the American
colonization of the Philippines played an enormous role not only
in the country’s government but also in the healthcare system.
This includes restructuring hospitals to include a surgical ward
and operating rooms. The surgical department was started,
and American nurse anesthetists assisted by Filipino nurses
administered anesthesia [16]. It is not until Dr. Quintin Gomez,
who will later on be named the father of anesthesia in the
Philippines, had formal anesthesia residency training in Chicago
and came back to the Philippines to establish anesthesia training
for doctors. From then on, anesthesia as a separate specialty
blossomed.
In Philippine culture, labor analgesia is oftentimes pre-determined.
Physician practices are influenced by their knowledge of a
certain technique whether it is intravenous opioids or regional
anesthesia. Most of the time, Filipino parturients try to toughen
it out until later in the course, until pain is unbearable. Unique to
the obstetric practice in the Philippines is the use of episiotomy,
necessitating local anesthetic infiltration. When the decision for
a cesarean section has been reached due to fetal or maternal
distress, the anesthesiologist would be called immediately, and
spinal anesthesia is the method of choice. Some patients opt to
do the Lamaze method, a psycho-prophylactic method that is
based on increasing a mother’s confidence in childbirth through
classes teaching different ways to cope with pain using relaxation
and breathing techniques, movement and massage.
Opinions and practices definitely vary from one health care
worker to the next. Factors such as religion, economic status,
knowledge, fears, and previous experiences all play a role in the
patient’s and practitioner’s decision for labor analgesia. A study
of obstetricians in one of the largest tertiary hospitals in Manila,
Philippines has shown that in 2003, among deliveries in the
charity service, only 35% were given some form of analgesia. 86%
to 90% of parturients in the private hospitals, on the other hand,
has received some form of analgesia [17].
Labor analgesia in modern times has evolved. Neuraxial
analgesia has been, to date, the most effective method of pain
relief during childbirth in contemporary clinical practice [18].
However, neuraxial analgesia techniques are not limited to just
standard epidural and Continuous Spinal-Epidural (CSE) blocks.
While the debate has been ongoing as to which neuraxial technique is superior to the other, a novel approach called Dural
Puncture Epidural (DPE) has recently gained popularity after the
cornerstone study that compared standard epidural and CSE with
DPE for labor analgesia.
Introduced in 1996 by Suzuki and colleagues in patients
undergoing lower abdominal surgery, DPE involves identifying
the epidural space, creating a dural puncture using a spinal
needle, withdrawing the spinal needle and the epidural catheter
inserted. DPE provides rapid onset of sacral analgesia along
with bilateral caudal spread in the obstetric population [19]. The
mechanism is that the conduit created by the dural puncture
provides translocation of medications from the epidural space
to the subarachnoid space. This technique provides better
hemodynamic stability, improved epidural catheter function, and
lower incidence of asymmetric block with fewer maternal and
fetal side effects [19]. Table 1 shows a summary of the maternal
and fetal/neonatal effects.
| Maternal |
Fetal/Neonatal |
| less hypotension |
no fetal bradycardia |
| less pruritus |
median Apgar scores 8-9 |
| no post-dural puncture headache |
less frequent Apgar scores 7 at 1 min and 5 min |
| backache, neck ache, persistent postpartum paresthesia same incidence with epidural |
|
| rate of cesarean delivery same with epidural/CSE |
|
| less uterine hypertonus |
|
| less uterine tachysystole |
|
Table 1: Maternal and Fetal/Neonatal Effects of DPE.
Conclusion
It goes without saying that one’s own labor experience is truly
different from another. Over the years, obstetric analgesia and
anesthesia continues to evolve, and each woman is entitled
to her own experiences of labor. Most of all, analgesic and
anesthetic options will continue to be a woman’s decision,
coupled with accurate data and knowledge for pain relief that an
anesthesiologist will be able to offer.
Delivery of the infant into the arms of a conscious and pain-free
mother is one of the most exciting and rewarding moments in
medicine (Donald D. Moir).
References
- Heaton CE (1946) The history of anesthesia and analgesia in obstetrics. J Hist Med Allied Sci 1:567-572.
- Caton D (2004) Medical science and social values. Int J Obstet Anesth 13: 167-173.
- Edwards ML, Jackson AD, 2017. The historical development of obstetric anesthesia and its contributions to perinatology. Am J Perinatol 7: 211-216.
- Gibson ME (2017) An early history of anesthesia in labor. J Obstet Gynecol Neonatal Nurs 46: 619-627.
- Sim P, Du B, Bacon DR (2000) Pioneer Chinese anesthesiologists: American influences. J Am Soc Anesthesiol 93:256-264.
- EH H (1946) Peter Parker and the introduction of anesthesia into Chicago. J Hist Med Allied Sci 1:670-674.
- Hu LQ, Flood P, Li Y, Tao W, Zhao P, et al. (2016) No pain labor and delivery: A global health initiative's impact on clinical outcomes in China. Anesth Analg 122: 1931-1938.
- Hu L, Yao S (2017) The development of obstetric anesthesiology in mainland China. Transl Perioper & Pain Med 2: 23-28.
- Saito S, Kikuchi H, Matsuki A (2017) The history of Japanese anesthesiology. J Anesth Hist 3: 103-106.
- Divekar VM, Naik LD (2001) Evolution of anaesthesia in India. J Postgrad Med 47: 149.
- Jeffery R, Jeffery P (1993) Traditional birth attendants in rural north India. Knowledge, power, and practice: The anthropology of medicine and everyday life 7-31.
- Hussain SS, Maheswari P (2017) Barriers for labour analgesia in South India-knowledge and attitude of relevant stakeholders: A hospital-based cross-sectional study. Indian J Anaesth 61: 170-173.
- Shrivastava D, Chaudhary P (2015) Perception of painless labor in rural India. J South Asian Fed Obstet Gynaecol 7:130-133.
- Bantug JP (1953) A short history of medicine in the Philippines during the Spanish regime, 1565-1898. Philippine Medical-Pharmaceutical College.
- Joven AE (2012) Colonial adaptations in tropical Asia: Spanish medicine in the Philippines in the seventeenth and eighteenth centuries. Asian Cult Stud 38:171-186.
- Egay LM (2001) The development of modern anesthesiology in the Philippines. Philipp J Anesthesiol 13: 10.
- Toral JA, Alvarez ML, Marinas GD (2010) Factors affecting the choice for the use or non-use of analgesia and the choice of the method of analgesia during labor and delivery among obstetricians at a tertiary government institution. Philippine J Obstet Gynecol 34: 67-75.
- Chestnut DH, Wong CA, Tsen LC, Kee WDN, Beilin Y et al. (2014) Chestnut's obstetric anesthesia: Principles and practice e-book. Else Health Sci.
- Gunaydin B, Erel S (2019) How neuraxial labor analgesia differs by approach: Dural puncture epidural as a novel option. J Anesth 33: 125-130.