Ferdinando D’Avenia1,2 and Richard Miron3*
1University Hospital of Parma, Parma, Italy
2Clinica Dentale D’Avenia, Private Practice, Parma, Italy
3Department of Periodontology, University of Bern, Bern, Switzerland
- *Corresponding Author:
- Richard Miron
Department of Periodontology, University of Bern, Bern, Switzerland
Tel: (954) 812-5061
E-mail: richard.miron@zmk.unibe.ch
Received date: July 09, 2018; Accepted date: July 30, 2018; Published date: August 06, 2018
Citation: D’Avenia F, Miron R. Vertical Bone Augmentation of the Posterior Mandible with Simultaneous Implant Placement Utilizing Atelo-
Collagen-Derived Bone Grafts and Membranes. Periodon Prosthodon. 2018, 4:3. doi: 10.21767/2471-3082.100045
Copyright: © 2018 D’Avenia F, et al. This is an open-access article distributed under the terms of the creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Keywords
Bone graft; Immediate implant dentistry; Atelo-collagen; Osteogenesis; Bone regeneration
Introduction
Vertical ridge augmentation is one of the most challenging
scenarios faced by a treating clinician [1-3]. Typically, a 2-stage
approach is planned whereby a 9-month healing period is
utilized for complete bone regeneration to take place,
especially in the vertical direction [3-5]. Only thereafter are
implants placed into regenerated bone and restored.
Several parameters are important to optimize bone
regeneration. First, space maintenance is critical since
compression towards bone is directly linked with bone
resorption via a reduced vascular supply [6-8]. For these
reasons and those presented later in this case report, titanium
meshes, or titanium-reinforced membranes have been utilized
as barriers in large bone augmentation procedures.
Much research has also focused on the choice of bone
grafting materials utilized to perform bone augmentation
procedures [9-11]. While each class of bone grafting materials
possess their regenerative advantages and disadvantages, the
use of autografts in combination with xenografts has been a
favoured choice by many clinicians. While the autografts are
known to induce optimal bone, regeneration owing to their
ability to contain living progenitor cells and release of
osteoinductive growth factors [12,13], they also turnover
rapidly which is why clinicians have often favoured their
combination with low substitution xenografts.
One of the limitations to xenografts is that the majority are
completed devoid of proteins and growth factors [14]. During
the sterilization process, typically xenografts undergo thermal
procedures that deproteinize the graft leaving only a
mineralized biomaterial. Despite this, xenografts have been
one of the most widely used bone grafting materials over the
past several decades [9,10,15].
Recently, the fabrication and processing of xenografts have
made major advancements whereby sterilization procedures have been optimized utilizing atelopeptidation and
lyophilization technologies that modify the immune-collagen
components of collagen from the bone grafting material to
non-immunogenic atelo-collagen [16,17]. Processing of
xenografts utilizing these technologies has been shown to
preserve the natural properties of collagen with an endproduct
containing roughly 30% remaining collagen type I
utilizing a natural and biocompatible approach. It is therefore
hypothesized that the regenerative potential of such grafts
further optimizes bone regeneration.
Parallel to recent advancements made in tissue engineering
of bone grafting materials, much advancement has also been
pioneered in three-dimensional digital implant dentistry
[18-21]. Today it is possible to plan surgeries completely
virtually with surgical guides being fabricated to place implants
precisely in their 3-dimensional space. Since dental implants
are known osteopromotive materials, they may also be utilized
as bone-promoting materials. This case reports highlights the
placement of dental implants using guided digital surgery with
simultaneous vertical bone augmentation of the mandibular
posterior ridge. While this treatment concept saves the patient
additional surgical time and morbidity by simultaneously
performing the bone grafting procedure and implant
placement simultaneously, we demonstrate how
advancements in biomaterials as well as digital planning have
optimized the clinician’s ability to successfully shorten surgical
treatment times for patients.
Case Report
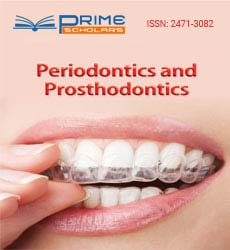
A 64-year-old female patient presents to the University
dental clinic in Parma, Italy with complaint of missing posterior
teeth. Cone-beam computed topography demonstrates severe
bone loss in both the horizontal and vertical directions in
regions 3.4-3.6 (Figure 1). The bridge placed in 3.3-X-X-X-3.7
was reported as currently failing and there was a large
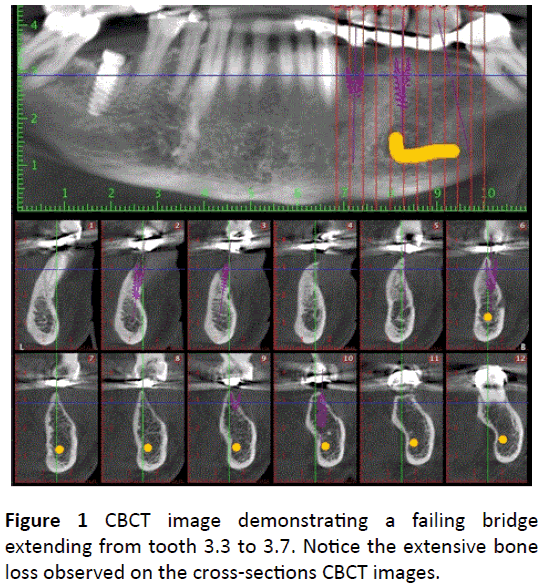
radicular cyst at site 3.4. Implants are therefore planned in
sites 3.4, 3.5 and 3.6 utilizing Romexis software (Planmeca, FI)
and, following, Nobel clinician (Nobel Biocare) software for the
surgical guide production (Figure 2). Notice the extent of
missing bone on the buccal surface of each of these implants
when digitally planned (Figure 2). Nevertheless, implant
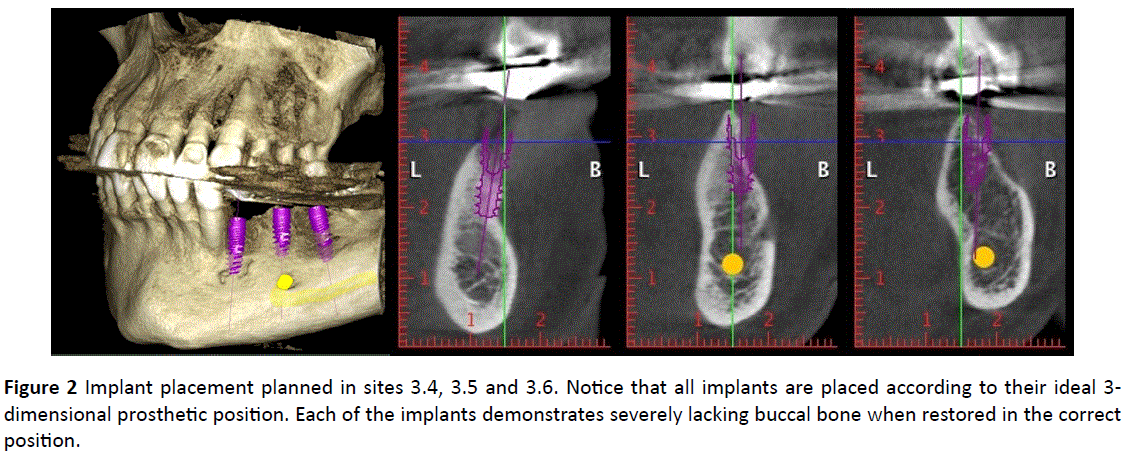
surgery is planned to utilize this correct prosthetically-driven
position. Figure 3 demonstrates a clinical photo of the intraoral
region 3.4-3.6. Notice the extent of bone loss observed
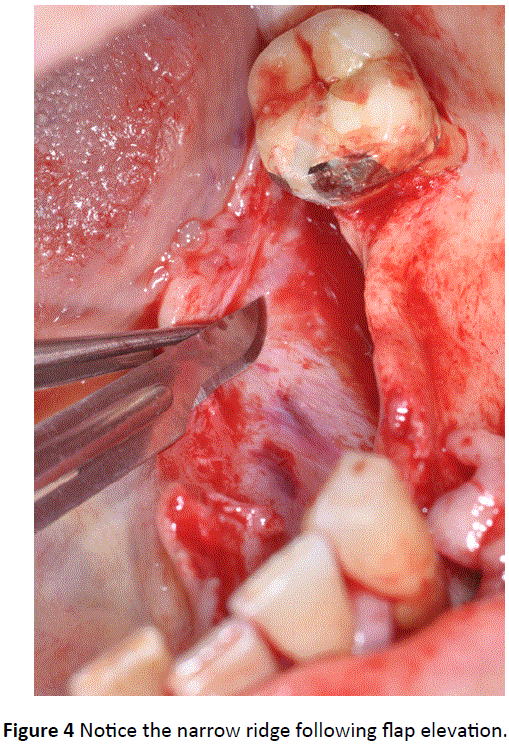
prior to flap elevation with a knife-edge ridge. Notice the bone loss occurring following flap elevation (Figure 4). Periosteal
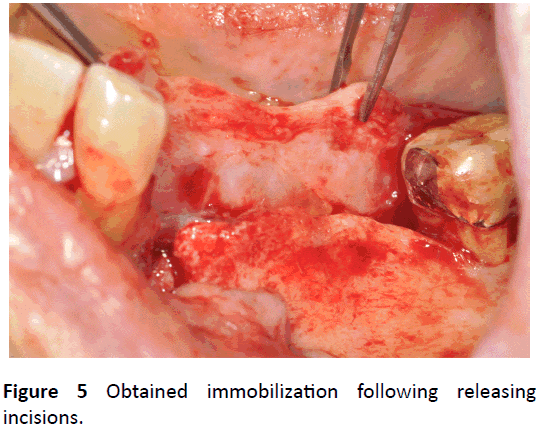
releasing incisions were performed to mobilize the flap (Figure
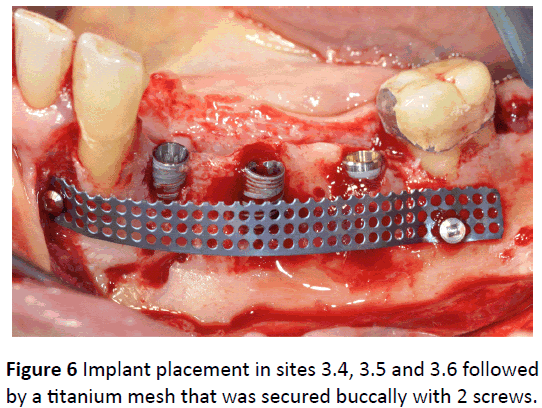
5). Three implants were placed (Nobel Active 3.5 × 13 mm -
Nobel Active 4.3 × 11.5 mm - Repalce CC 4.3 × 13 mm,
Nobelbiocare) in positions 3.4, 3.5 and 3.6 according to digital
planning. Notice that the implants were placed crestal to the
bone ridge owing to the planned vertical augmentation
procedure (Figure 6). A 0.2 mm thick titanium mesh band was
secured buccaly in order to create and support an adequate
regenerative space with minimal compression on the buccal
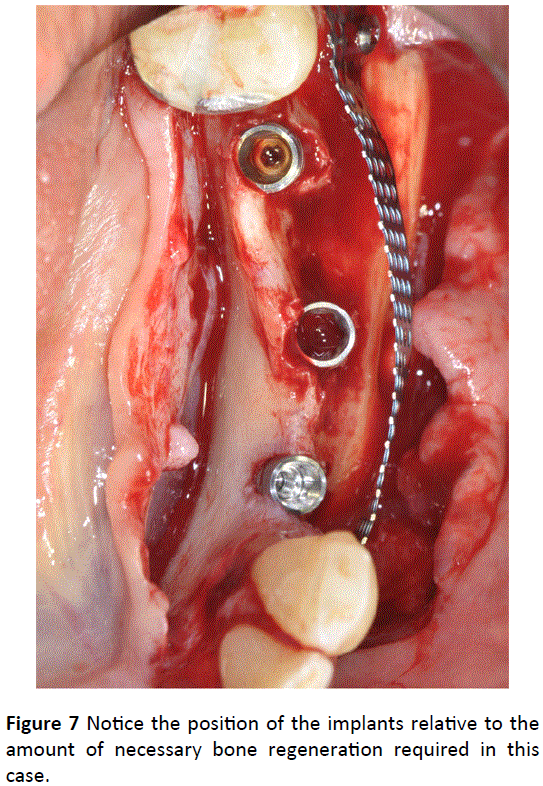
bone. Notice the extent of missing bone on the buccal surface
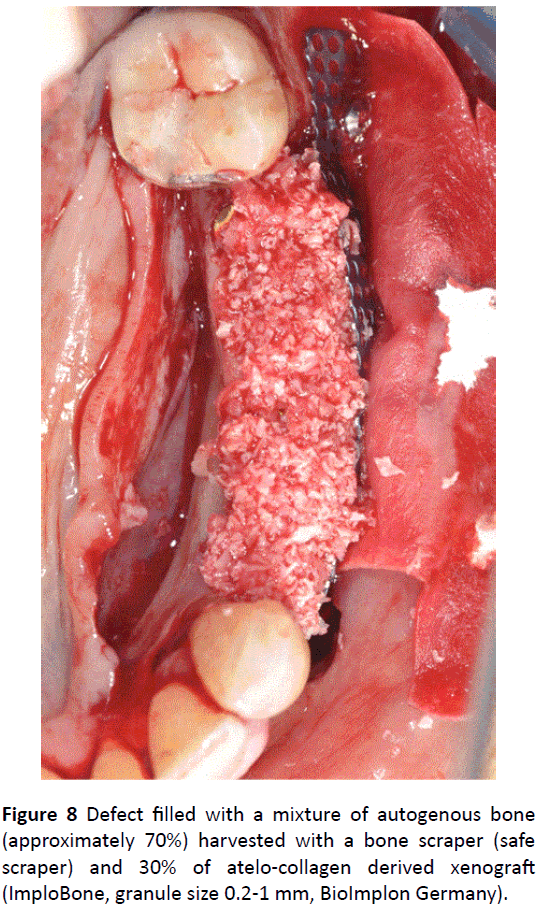
of the implants and interproximal (Figure 7). The defect was
then filled with a mixture of autogenous bone (approximately
70%) harvested with a bone scraper (safescraper) [22] from
the mandibular omo-lateral ramus and 30% of atelo-collagen
derived xenograft (ImploBone, granule size 0.5-1 mm,
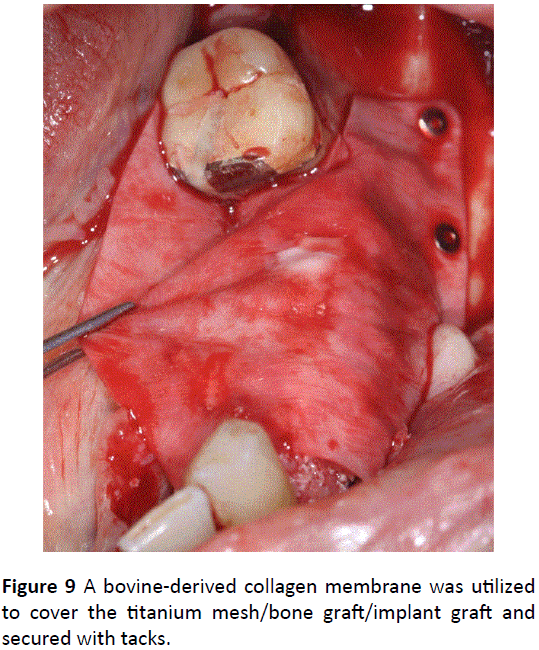
Bioimplon Germany) (Figure 8). A bovine type I collagen
membrane was then utilized to cover the entire defect and the
membrane was secured in place with tacks on the buccal side
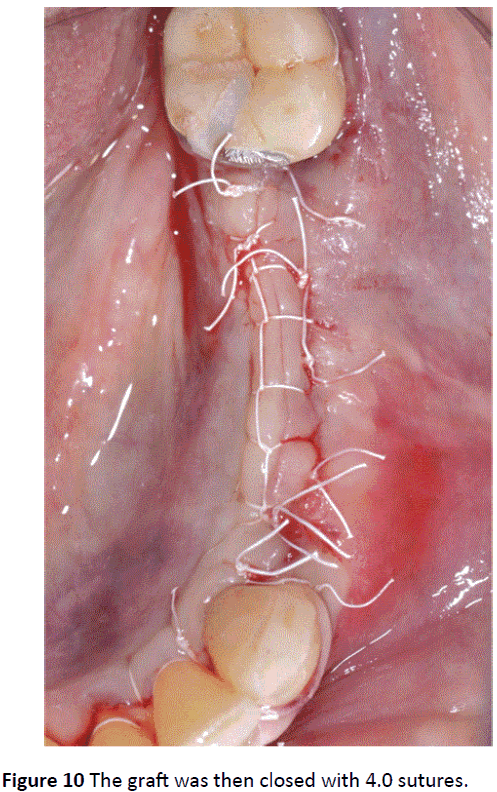
and sutured on the lingual side (Figure 9). The flap was then
double sutured closed with 4.0 sutures (Figure 10).
Figure 1: CBCT image demonstrating a failing bridge
extending from tooth 3.3 to 3.7. Notice the extensive bone
loss observed on the cross-sections CBCT images.
Figure 2: Implant placement planned in sites 3.4, 3.5 and 3.6. Notice that all implants are placed according to their ideal 3-
dimensional prosthetic position. Each of the implants demonstrates severely lacking buccal bone when restored in the correct
position.
Figure 3: Clinical image of the knife-edge ridge observed
between sites 3.4 and 3.6. An extensive bone augmentation
procedure is planned in both the horizontal and vertical
direction.
Figure 4: Notice the narrow ridge following flap elevation.
Figure 5: Obtained immobilization following releasing
incisions.
Figure 6: Implant placement in sites 3.4, 3.5 and 3.6 followed
by a titanium mesh that was secured buccally with 2 screws.
Figure 7: Notice the position of the implants relative to the
amount of necessary bone regeneration required in this
case.
Figure 8: Defect filled with a mixture of autogenous bone
(approximately 70%) harvested with a bone scraper (safe
scraper) and 30% of atelo-collagen derived xenograft
(ImploBone, granule size 0.2-1 mm, BioImplon Germany).
Figure 9: A bovine-derived collagen membrane was utilized
to cover the titanium mesh/bone graft/implant graft and
secured with tacks.
Figure 10: The graft was then closed with 4.0 sutures.
After 7 months of healing, CBCT demonstrated adequate
bone formation in both the vertical and horizontal directions
(Figure 11). A partial thickness flap was then raised, the Ti
mesh was removed and the implants were uncovered (Figure
12). Notice the amount of buccal bone that was formed after 7
months (Figure 13). A collagen matrix graft (Mucograft,
Geistlich, Switzerland) was then utilized on the buccal surface
to improve soft tissue thickness and healing abutments were
then placed (Figure 14). After 15 days, sutures were removed,
an impression was taken and a provisional restoration with
loading was placed (Figure 15). Notice the excellent bone
levels around the implants, viewed by X-ray (Figure 16). Five
months later, notice the excellent soft tissue healing (Figure
17). A final restoration was then screwed in place (Figures 18). Figure 19 demonstrates an X-ray taken 15 months post-op with
excellent maintenance and bone levels around the implants.
Figure 11: CBCT of the regenerated area after 7 months of
healing. Notice the bone formation occuring especially on
the buccal surface of all implants.
Figure 12: Partial thickness flap reveals excellent new bone
formation above and around all implants.
Figure 13: Notice the bone formation occurring; especially
on the buccal surface.
Figure 14: Mucograft utilized to improve soft tissue thickness
around the implant.
Figure 15: Fifteen days post mucograft placement, notice the
soft tissue healing. A provisional restoration with load was
then applied.
Figure 16: Notice the bone levels around the implants 7
months post initial surgery.
Figure 17: Notice the soft tissue contouring 8 months postgrafting.
Figure 18: Final zirconia restoration.
Figure 19: Final X-ray 15 months post-surgery. Notice the
maintenance of excellent bone levels utilizing this treatment
modality.
Discussion
The present case report demonstrated the successful use of
combining a large bone augmentation procedure of a severely
resorbed posterior mandible with simultaneous implant
placement. Though initially the implant was placed in
inadequate bone, the grafting procedure utilizing a
combination of autogenous bone and xenograft mixture was
able to successfully regenerate this large bone defect. It was
recently demonstrated that the xenograft’s incorporation of
atelo-collagen offers numerous advantages when compared to
xenografts devoid of collagen which include better adsorption
of growth factors, as well as improved cellular attachment,
proliferation and osteoblast differentiation [17].
In terms of their biomaterial characteristics, this relatively
novel processing technique does not use heat (thermal)
processing which has been linked with both destroying the
remaining protein content from the bone graft as well as
negatively impacts the natural crystalline micro-structure of
hydroxyapatite. These advanced sterilization procedures for
xenografts has been shown to preserve lyophilized collagen
with lower humidity which favours the hydrophilicity of the
bone matrix. In total, these xenografts contain roughly 2%
moisture, 65-75% hydroxyapatite, 25-35% atelo-collagen
content and up to 0.1% non-collagenous proteins [17].
Therefore, these combined advantages when compared to
deproteinized xenografts favours their ability to further
stimulate new bone formation, especially when utilized in
combination with autografts – known to secrete a wide array
of growth factors and cytokines [12,13].
Typically, regeneration of severely atrophic posterior
mandibles is performed using a 2-stage approach [3-5]. This is
owing to the difficulty in regenerating large bone defects in
the posterior mandible, especially in the vertical direction. In
the present study, the implants were utilized as a sort of tenting screw with the authors knowingly aware that bone can
be formed directly in opposition to the implant surface (owing
to the favourable osteoconductive features of a roughened
titanium surface [23,24]). In the present technique, the
implants were first place in the correct 3-dimensional position,
and thereafter this bone grafting complex was utilized in
combination with the implants and titanium mesh to optimize
space maintenance. After only a 7-month healing period, both
implant osseointegration and adequate bone regeneration
were achieved in a single surgery. This favoured much shorter
treatment protocols with the patient not requiring a second
surgery to place implants since they were performed
simultaneously.
Many new concepts were highlighted in this case report.
First, the atelo-collagen bone grafting material promoted
adequate bone regeneration in combination with an autograft
likely owing to the better immune response to natural atelocollagen.
Furthermore, it was found that simultaneous implant
placement was hypothesized to further speed graft
consolidation by providing 1) space maintenance, 2) less
overall defect bone volume requiring regeneration, and 3) a
titanium surface that favours osteoconduction. Future longterm
documented cases are nevertheless required to further
validate this concept.
Conclusion
This case report describes a surgical concept/technique
where concurrent guided bone regeneration and implant
placement was performed simultaneously. Key features to the
successful outcomes were the use of 3-dimensional implant
planning/placement, as well as the use of a titanium mesh to
prevent tension/compression on the regenerating bone. Lastly,
novel xenograft biomaterials that incorporate atelo-collagen
within the graft complex were shown to favourably promote
bone regeneration, likely owing to their superior
biocompatibility. Future comparative and large human studies
are necessary to further validate this proposed treatment
modality and validate this treatment concept.
References
- Roccuzzo M, Savoini M, Dalmasso P, Ramieri G (2017) Long-term outcomes of implants placed after vertical alveolar ridge augmentation in partially edentulous patients: a 10-year prospective clinical study. Clin oral implan res 28:1204-1210.
- Chavda S and Levin L (2018) Human Studies of Vertical and Horizontal Alveolar Ridge Augmentation Comparing Different Types of Bone Graft Materials: A Systematic Review. J Oral Implantol 44:74-84.
- Misch C (2017) Vertical Alveolar Ridge Augmentation in Implant Dentistry: A Surgical Manual.
- Urban IA, Lozada JL, Jovanovic SA, Nagursky H, Nagy K (2014) Vertical ridge augmentation with titanium-reinforced, dense-PTFE membranes and a combination of particulated autogenous bone and anorganic bovine bone-derived mineral: a prospective case series in 19 patients. Int J Oral Maxillofac Implan 29.
- Lozada JL, Urban I, Kan JY (2016) Decision Making in Bone Augmentation to Optimize Dental Implant Therapy. Evidence-based Implant Treatment Planning and Clinical Protocols:46.
- Mammoto T, Jiang A, Jiang E, Mammoto A (2013) Platelet rich plasma extract promotes angiogenesis through the angiopoietin1-Tie2 pathway. Microvas Res 89:15-24.
- Rakhmatia YD, Ayukawa Y, Furuhashi A and Koyano K (2013) Current barrier membranes: titanium mesh and other membranes for guided bone regeneration in dental applications. J Prosthodon Res 57:3-14.
- Watzinger F, Luksch J, Millesi W, Schopper C, Neugebauer J et al. (2000) Guided bone regeneration with titanium membranes: a clinical study. Br J Oral Maxillofac Surg 38:312-315.
- Buser D, Chappuis V, Kuchler U, Bornstein MM, Wittneben JG, et al. (2013) Long-term stability of early implant placement with contour augmentation. J Den Res 92:176s-82s.
- Jensen SS, Aaboe M, Janner SF, Saulacic N, Bornstein MM, et al. (2015) Influence of particle size of deproteinized bovine bone mineral on new bone formation and implant stability after simultaneous sinus floor elevation: a histomorphometric study in minipigs. Clinical implant dentistry and related research 17:274-85.
- Miron RJ, Zhang YF (2012) Osteoinduction: a review of old concepts with new standards. J Den Res 91:736-44.
- Miron RJ, Gruber R, Hedbom E, Saulacic N, Zhang Y, et al. (2013) Impact of bone harvesting techniques on cell viability and the release of growth factors of autografts. Clin Implant Dent Res 15:481-9.
- Miron RJ, Hedbom E, Saulacic N, Zhang Y, Sculean A, et al. (2011) Osteogenic potential of autogenous bone grafts harvested with four different surgical techniques. Journal of dental research 90:1428-33.
- Miron RJ, Zhang Q, Sculean A, Buser D, Pippenger BE, et al. (2016) Osteoinductive potential of 4 commonly employed bone grafts. Clin Oral Invest.
- Jensen SS, Bosshardt DD, Gruber R, Buser D (2014) Long-term stability of contour augmentation in the esthetic zone: histologic and histomorphometric evaluation of 12 human biopsies 14 to 80 months after augmentation. J Periodontol 85:1549-56.
- El Raouf MA, Fujioka-Kobayashi M, AbdEl-Aal ABM, Zhang Y, Miron RJ (2017) Novel Bioabsorbable Bovine Derived Atelo-Collagen Type I Membrane: Characterization into Host Tissues. Periodon Prosthodon 3.
- Fujioka-Kobayashi M, Schaller B, Saulacic N, Zhang Y, Miron RJ (2017) Growth factor delivery of BMP9 using a novel natural bovine bone graft with integrated atelo-collagen type I: Biosynthesis, characterization, and cell behavior. J Biomed Mat Res Part A 105:408-418.
- Patel N (2010) Integrating three-dimensional digital technologies for comprehensive implant dentistry. J Am Dent Assoc 141:20S-24S.
- Stapleton BM, Lin W-S, Ntounis A, Harris BT and Morton D (2014) Application of digital diagnostic impression, virtual planning, and computer-guided implant surgery for a CAD/CAM-fabricated, implant-supported fixed dental prosthesis: a clinical report. J Pros Dent 112:402-408.
- Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, et al. (2009) Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implant 24:92-109.
- Katsoulis J, Pazera P, Stern R (2009) Prosthetically driven, computer-guided implant planning for the edentulous maxilla: a model study. Clin Implant Dent Res 11:238-245.
- Zaffe D, D'avenia F (2007) A novel bone scraper for intraoral harvesting: a device for filling small bone defects. Clin Oral Implant Res 18:525-533.
- Martin J, Schwartz Z, Hummert T, Schraub D, Simpson J, et al. (1995) Effect of titanium surface roughness on proliferation, differentiation, and protein synthesis of human osteoblast‐like cells (MG63). J Biomed Mat Res Part A 29:389-401.
- Miron RJ, Oates CJ, Molenberg A, Dard M, Hamilton DW (2010) The effect of enamel matrix proteins on the spreading, proliferation and differentiation of osteoblasts cultured on titanium surfaces. Biomaterials 31:449-460.