Case Report - (2017) Volume 2, Issue 4
Peter Max Halschou-Jensen1*, Andreas Balslev-Clausen2 and Peter Søndergaard1
1Department of Orthopaedic Surgery, Herlev University Hospital, Denmark
2Department of Orthopaedic Surgery, Hvidovre University Hospital, Denmark
Received date: July 11, 2017; Accepted date: August 16, 2017; Published date: August 18, 2017
Citation: Halschou-Jensen PM, Balslev-Clausen A, Søndergaard P (2017) Traumatic Hip Dislocation after Fall during Sledging. Trauma Acute Care Vol.2:52. doi: 10.21767/2476-2105.100052
Copyright: © 2017 Halschou-Jensen PM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Traumatic hip dislocation is uncommon in children. Yet, it represents an orthopaedic emergency, because delayed treatment can lead to avascular necrosis of the femoral head. In this case a four- year-old boy and an eight-year-old girl were treated in an emergency department less than two weeks apart. They both received a posterior hip dislocation after accident during sledging. Their hips were reduced within 6 h in the operating theatre, and the patients were discharged few days later. At the follow-up after six and 12 weeks both patients were doing well, and X-rays were normal.
Keywords
Traumatic hip dislocation; Orthopaedic emergency
Background
Traumatic hip dislocation is uncommon in children [1-4]. In children under the age of 14 years the incidence is 0.8 per million per year [3]. In Denmark there is about 900,000 children from 0-14 years [5], giving 0.7 traumatic hip dislocations each year.
The most common complications are avascular necrosis of the femoral head (6%), re-dislocation (6%) and coxa magna (10%) [1-4].
The overall treatment is quick reduction in general anaesthesia.
Case Report
Within a 2 week period a 4 year old boy and an 8 year old girl showed up in the emergency department with pain in the left hip after fall during sledging.
In both cases x-ray of the left hip showed a posterior dislocation (Figure 1), and the treatment was closed reduction of the hip in general anaesthesia.
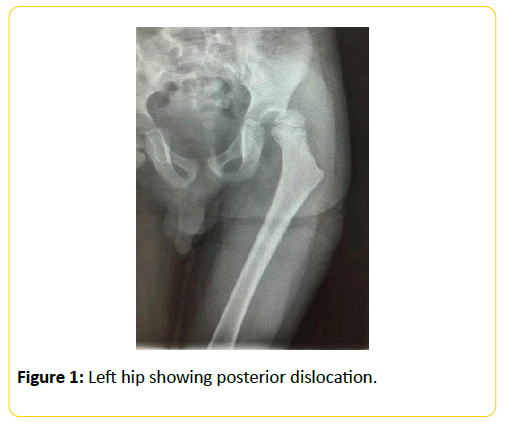
Figure 1: Left hip showing posterior dislocation.
The day after they did a CT scan that showed no sign of intra-articular damage. Both patients were discharged few days later in general god condition.
In both cases there were no predisposing factors, the hips were reduced within 6 h after the injury and the aftercare dictated 6 weeks without weight bearing to protect the cartilage. No cast were prescribed.
The 6 and 12 weeks follow up showed normal x-ray and patients without any symptoms.
Discussion
Traumatic hip dislocation in children is uncommon, and the existing literature is primarily case reports. Therefore, the updated recommendations regarding treatment and follow up, is based on low evidence literature. Do to the fact that it is a rare condition, makes is very difficult to do randomised controlled trials, and the recommendation must be based on expert opinions and case reports.
The anatomy of younger children causes traumatic hip dislocations to occur due to low energy trauma as the acetabulum and surrounding tissue is less rigid, and posterior dislocation is most frequent (96%) [1-4]. There are rarely associated injuries and rarely seen hip dysplasia or connective tissue disease in the described cases, but this may be considered a predisposing factor [1].
In the younger group, the incidence is almost the same among boys and girls, while in the elder children the incidence is highest among boys [1-3].
During the clinical examination, the child typically stays with the affected leg shortened, adducted, flexed and inwardly rotated in the hip (Figure 2). The diagnosis is made on an anterior/posterior (AP) X-ray of the pelvis, and if possible a lateral view. CT and MR scan are not indicated in the primary investigation. The treatment is pain relief and rapid reduction of the hip in general anaesthesia.
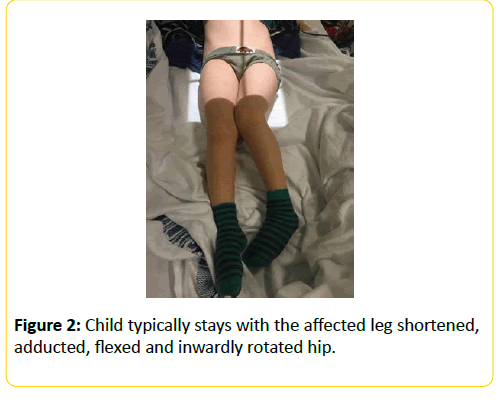
Figure 2: Child typically stays with the affected leg shortened, adducted, flexed and inwardly rotated hip.
Traumatic hip dislocation in children is an orthopaedic emergency condition and the hip should be reduced as soon as possible to minimize the risk of complications, and several studies describe a 6 h limit [1-4]. Traumatic hip dislocations that are reduced later than 6 h post-trauma are described with up to 20-fold increased risk of later avascular necrosis of the femoral head [1,3,4]. The literature does not describe any specific methods for reduction of the hip, but recommends the same methods as in adults. Most often it will be possible with the patient in the supine position, while applying longitudinal distraction of the femur with the hip slightly inwardly rotated and in 90° flexion.
In larger children there is a risk of epiphysiolysis of the femoral head, and reduction should be done with caution.
If it is not possible after three attempts to reduce the hip with a closed procedure, open reduction should be performed. The surgical approach must be in the same direction as the dislocation, i.e., posterior approach in posterior dislocation and anterior approach in anterior dislocation [4].
After reduction the stability should be tested, and the reduction should be controlled with X-ray AP and Lateral, and additional Lauenstein projection to exclude epiphysiolysis of the femoral head.
If X-ray shows joint space asymmetry, it is recommended to do a CT or MRI scan to exclude interposition of structures such as labrum, capsule, or osteochondral fragments [1,3,4].
It is recommended that there is no weight bearing in the affected leg for 6 weeks to protect the cartilage, and in the event of instability apply a hip spica cast for 6 weeks.
Outpatient follow-up with X-ray of the hip is recommended after 6 and 12 weeks and clinical check after 52 weeks. Traumatic hip dislocation is a rare condition in children. Evidence is low, but by rapid diagnosis and reduction (<6 h) of the hip in general anaesthesia, the prognosis is good.
References
Traumatic hip dislocation; Orthopaedic emergency
Traumatic hip dislocation is uncommon in children [1-4]. In children under the age of 14 years the incidence is 0.8 per million per year [3]. In Denmark there is about 900,000 children from 0-14 years [5], giving 0.7 traumatic hip dislocations each year.
The most common complications are avascular necrosis of the femoral head (6%), re-dislocation (6%) and coxa magna (10%) [1-4].
The overall treatment is quick reduction in general anaesthesia.
Within a 2 week period a 4 year old boy and an 8 year old girl showed up in the emergency department with pain in the left hip after fall during sledging.
In both cases x-ray of the left hip showed a posterior dislocation (Figure 1), and the treatment was closed reduction of the hip in general anaesthesia.
The day after they did a CT scan that showed no sign of intra-articular damage. Both patients were discharged few days later in general god condition.
In both cases there were no predisposing factors, the hips were reduced within 6 h after the injury and the aftercare dictated 6 weeks without weight bearing to protect the cartilage. No cast were prescribed.
The 6 and 12 weeks follow up showed normal x-ray and patients without any symptoms.
Traumatic hip dislocation in children is uncommon, and the existing literature is primarily case reports. Therefore, the updated recommendations regarding treatment and follow up, is based on low evidence literature. Do to the fact that it is a rare condition, makes is very difficult to do randomised controlled trials, and the recommendation must be based on expert opinions and case reports.
The anatomy of younger children causes traumatic hip dislocations to occur due to low energy trauma as the acetabulum and surrounding tissue is less rigid, and posterior dislocation is most frequent (96%) [1-4]. There are rarely associated injuries and rarely seen hip dysplasia or connective tissue disease in the described cases, but this may be considered a predisposing factor [1].
In the younger group, the incidence is almost the same among boys and girls, while in the elder children the incidence is highest among boys [1-3].
During the clinical examination, the child typically stays with the affected leg shortened, adducted, flexed and inwardly rotated in the hip (Figure 2). The diagnosis is made on an anterior/posterior (AP) X-ray of the pelvis, and if possible a lateral view. CT and MR scan are not indicated in the primary investigation. The treatment is pain relief and rapid reduction of the hip in general anaesthesia.
Traumatic hip dislocation in children is an orthopaedic emergency condition and the hip should be reduced as soon as possible to minimize the risk of complications, and several studies describe a 6 h limit [1-4]. Traumatic hip dislocations that are reduced later than 6 h post-trauma are described with up to 20-fold increased risk of later avascular necrosis of the femoral head [1,3,4]. The literature does not describe any specific methods for reduction of the hip, but recommends the same methods as in adults. Most often it will be possible with the patient in the supine position, while applying longitudinal distraction of the femur with the hip slightly inwardly rotated and in 90° flexion.
In larger children there is a risk of epiphysiolysis of the femoral head, and reduction should be done with caution.
If it is not possible after three attempts to reduce the hip with a closed procedure, open reduction should be performed. The surgical approach must be in the same direction as the dislocation, i.e., posterior approach in posterior dislocation and anterior approach in anterior dislocation [4].
After reduction the stability should be tested, and the reduction should be controlled with X-ray AP and Lateral, and additional Lauenstein projection to exclude epiphysiolysis of the femoral head.
If X-ray shows joint space asymmetry, it is recommended to do a CT or MRI scan to exclude interposition of structures such as labrum, capsule, or osteochondral fragments [1,3,4].
It is recommended that there is no weight bearing in the affected leg for 6 weeks to protect the cartilage, and in the event of instability apply a hip spica cast for 6 weeks.
Outpatient follow-up with X-ray of the hip is recommended after 6 and 12 weeks and clinical check after 52 weeks. Traumatic hip dislocation is a rare condition in children. Evidence is low, but by rapid diagnosis and reduction (<6 h) of the hip in general anaesthesia, the prognosis is good.