Sollaku S1, Frantellizzi V1,2*, Casciani E3, Gualdi G3, Liberatore M1, Monteleone F1 and De Vincentis G1
1Department of Radiological, Oncological and Anatomo-Pathological Sciences, University of Rome Sapienza, Rome, Italy
2PhD Programm: Angio-Cardio-Thoracic Pathophisiology and Imaging, Sapienza University of Rome, Rome, Italy
3Department of Emergency Medicine, Policlinico Umberto I, Sapienza University of Rome, Rome, Italy
Corresponding Author:
Dr Viviana Frantellizzi
Department of Radiological, Oncological and Anatomo-Pathological Sciences
University of Rome Sapienza,Rome, Italy
Tel: +39 06 49978590
Fax: +39 06 49978592
E-mail: viviana.frantellizzi@uniroma1.it
Received date: June 24, 2017; Accepted date: August 14, 2017; Published date: August 16, 2017
Citation: Sollaku S, Frantellizzi V, Casciani E, Gualdi G, Liberatore M, et al. The Rare Case of Positive FDG-Positron Emission Tomography for Giant Cavernous Hemangioma of the Liver. Br J Res 2017, 4(3):19. doi: 10.21767/2394-3718.100019
Copyright: © 2017 Sollaku S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
18F-FDG PET; Cavernous hemangioma; Large hemangioma; Hepatic hemangioma
Case
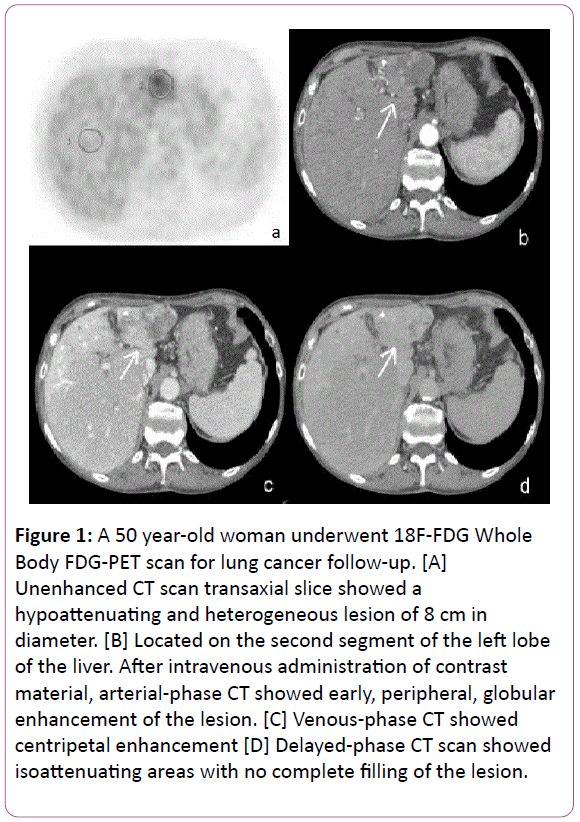
These findings suggested for a giant hemangioma, the most common benign liver tumor [1] (Figure 1). Large hemangiomas often present heterogeneous patterns and these heterogeneous appearances are shown because of intratumoral changes such as hemorrhage, thrombosis, extensive hyalinization, necrosis and fibrosis [2]. PET/CT is reported to be useful for the differentiation of benign from malignant liver lesions [3]. PET/CT scan demonstrated high FDG uptake compared to normal liver parenchyma. The lesion was also analyzed semi quantitatively using the SUV (Standardized uptake value) and L/B (Lesion to liver background) ratio. The maximum SUV for the lesion was 5.3 and L/B ratio was 2.3. This PET/CT scan was compared with previous PET/CT examination that showed high FDG uptake of the lesion as compared to the normal liver parenchyma. It is well known that benign liver lesions do not accumulate FDG more than normal liver background [4], considering a cut-off level to differentiate benign from malignant liver masses as 2 for the L/B ratio and 3.5 for the SUV of the lesion.
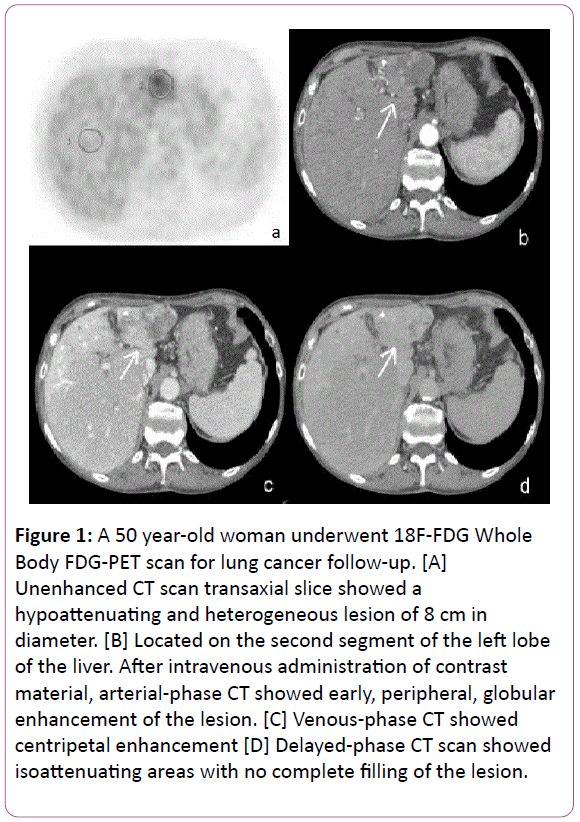
Figure 1: A 50 year-old woman underwent 18F-FDG Whole Body FDG-PET scan for lung cancer follow-up. [A] Unenhanced CT scan transaxial slice showed a hypoattenuating and heterogeneous lesion of 8 cm in diameter. [B] Located on the second segment of the left lobe of the liver. After intravenous administration of contrast material, arterial-phase CT showed early, peripheral, globular enhancement of the lesion. [C] Venous-phase CT showed centripetal enhancement [D] Delayed-phase CT scan showed isoattenuating areas with no complete filling of the lesion.
The lesion in our study showed typical hemangioma contrast enhancing during CT scan, like hepatic epithelioid hemangioendothelioma, a rare tumor of vascular origin [5,6]. Giant hemangioma which high SUV and high L/B ratio showed difficulties to differentiate it from other malignant lesions. FDG uptake can be explained by various hypotheses. Giant hemangioma can degenerate into a malignant tumor, the angiosarcoma. To our knowledge in the literature there is only one report of malignant transformation of hepatic hemangioma [7]. Another report described an angiosarcoma surrounding a cavernous hemangioma raising the hypothesis of malignant transformation of a hemangioma [8]. However the lesion of our case did not show changes in dimensions over time. One other hypothesis is that hemangiomas can have inflammatory features. This inflammatory process can explain glucose consumption thus high FDG uptake. The last hypothesis is connected with tissue metabolism. Benign tumors show normal to decreased metabolism. But these benign lesions can have hypermetabolic patterns showing increased FDG uptake. Hypervascularization and slowed down “wash-out” can lead to glucose accumulation. Necrotic areas within the lesion better support the last hypothesis.
References
- Sharma B, Martin A, Zerizer I (2013) Positron Emission Tomography-Computed Tomography in Liver imaging. Semin Ultrasound CT MR 34: 66-80.
- Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, et al. (2000) Imaging of atipical hemangiomas of the liver with pathologic correlation. RadioGraphics 20: 379-397.
- Delbeke D, Martin WH, Sandler MP, Chapman WC, Wright Jr KR, et al. (1998) Evaluation of benign vs malignant hepatic lesions with positron emission tomography. Arch Surg 133: 510-516.
- Shimada K, Nakamoto Y, Isoda H, Saito H, Arizono S, et al. (2010) FDG PET for giant cavernous hemangioma. Important clue to differentiate from a malignant vascular tumor in the liver. Clinical Nuclear Medicine 35: 924-926.
- Lyburn ID, Torreggiani WC, Harris AC, Zwirewich CV, Buckley AR, et al. (2003) Hepatic epithelioid hemangioendothelioma: Sonographic, CT, and MR Imaging appearances. AJR 180: 1359-1364.
- Miller WJ, Dodd GD III, Federle MP, Baron RL (1992) Epithelioid hemangioendothelioma of the liver: imaging findings with pathologic correlation. AJR 159: 53-57.
- Bertrand L, Puyeo J, Pages A, Ciurana AJ, Blanc F, et al. (1980) Hemangiosarcome du foie secondaire à une angiome caverneux calcifié: mort en coagulopathie de consommation. Ann Gastroenterol Hepatol 16: 19-27.
- Tohme C, Drouot E, Piard F, Bernard A, Brachet A, et al. (1991) Hémangiome caverneux du foie associé à un angiosarcome: transformation maligne? Gastroenterol Clin Biol 15: 83-86.