Background: Paging-systems (PS) are important means of communication between providers. PS may provide only limited information, and quality of communication (QOC) may be suboptimal. To investigate QOC using PS at a general surgery residency program.
Methods: 7 surgical services pagers records were obtained from communication department over 24 hour in 2017. In addition to frequency, pages were evaluated for 5-quality metrics: paging party, callback number, urgency, reason for page, and patient identifiers. A survey was distributed to general surgery residents evaluating their perception of QOC.
Results: 126 pages were captured over 24 hours (61% am-shift, 39% pm-shift). Thirty-two% contained only a callback number, and 20% contained all 5-components. Fifty-one% were from patient wards, 28% consultants, and 21% peri-operative services. 97% did not include urgency, and 39% reason for page. Median components was 3, with consultants having an OR=6; [CI95%:1.9-18.2] (p<0.01) to page at least median number of components. There was no significant difference between am and pm-shifts. 48% felt that minimum components should be 5, none believed callback only is adequate or would relate to emergent/ urgent matters, only rarely/occasionally they did receive their set minimum or ≥ 3 required components, and despite returning callback number pages immediately, 21% would not wait>1 min on-hold. Majority agreed that callback only may lead to loss of time and felt that standardizing paging can improve communication.
Conclusion: The PS is still relevant in a hospital setting. Many pages could be improved to facilitate efficient communication to surgery residents. Residents feel strongly that there is room to improve QOC between providers. Despite relevance of PS, updating the system is necessary to improve inter-professional communication.
Keywords
Quality improvement; Communication; Residents; Pager
Introduction
During the early nineteen-thirties and forties, delivering messages to in-house physicians involved overhead paging by the operator. Physicians would return the call to the operator who would then transfer them to their paging party. Some practitioners carried a “beeper,” which notified the physician to call the operator by editing a beep. After the introduction of the pager in the 1950’s, hospitals praised the improved and swift communication between healthcare providers [1,2].
Several decades later, resident physicians still use the same technology to communicate with nurses, consultants and other ancillary services about patient care. Even the term “beeper” remains in use, analogous to the persistence of the term “dial a telephone” despite the lack of dials. However, communication technologies have evolved considerably outside of the hospital. Smartphones and apps such as Instagram, Twitter, FaceTime, and of course messaging allow an unprecedented ease in communication. Concerns over privacy and security currently limit the applicability of these modalities in medicine, but the technology is still familiar to all. We investigated the efficacy and quality of communication using the paging system in an academic general surgery residency.
Materials and Methods
Communication practices
At our institution, residents are provided with two-way pagers. Residents are typically paged using an online intranet webpage to produce alphanumeric messages. It is still possible to contact the hospital operator to page a resident, but they also rely on the communication webpage to alert the physician. Surgical services are assigned specific pager numbers allowing other healthcare providers to reach the resident physician directly. Records of these pages are stored by our communication department and are retrievable.
Each specialty surgical service team is assigned a pager number that is transferred to the junior resident when their shift begins. Despite having the option for 2-way pagers available, this function is almost never used at our facility. These pagers represent the main means of communication between surgical providing teams, and the surgical wards staff, consultants, and ancillary services such as laboratory.
Methods
After obtaining IRB exemption for our study, the records of seven specialty surgical services covered by our general surgery residents were obtained on a random 24 hour period during a weekday in the year 2017. These services included; emergency surgery, minimally invasive surgery, surgical oncology, pediatric surgery, vascular surgery, urology, and plastics and reconstructive surgery. Pager records were evaluated for time of page in addition to five components; paging party, urgency, patient identifiers, complaint or main reason for page, callback number and signature of the paging party (Table 1).
| S.no |
Element |
Definition |
| 1 |
Identity of Paging Party |
Individual/team sending page clearly mentioned |
| 2 |
Identity of Patient |
Name, location, team, or MRNŦ |
| 3 |
Urgency |
Non-urgent, urgent, emergent, or FYI/Action/Reply |
| 4 |
Main Complaint/Reason for Page |
Stating problem or request to be addressed |
| 5 |
Callback Number |
Number to be able to reach paging party |
Note: ŦMRN: Medical Record Number.
Table 1: Elements of a quality page.
A survey was distributed to residents in our surgical program to evaluate resident perception of communication using current paging system, urgency relayed in paged messages, annoyance that some pages may cause and their opinion regarding changing the current practice. A sample of the survey is attached as (Appendix 1).
Data from pager records and surveys was analyzed using the IBM SPSS® (NY, USA) for frequencies and distribution. Using Fisher’s Exact Test, we attempted to identify factors predicting a minimum of the median number of components or higher, including service, paging party and am versus pm-shift.
Results
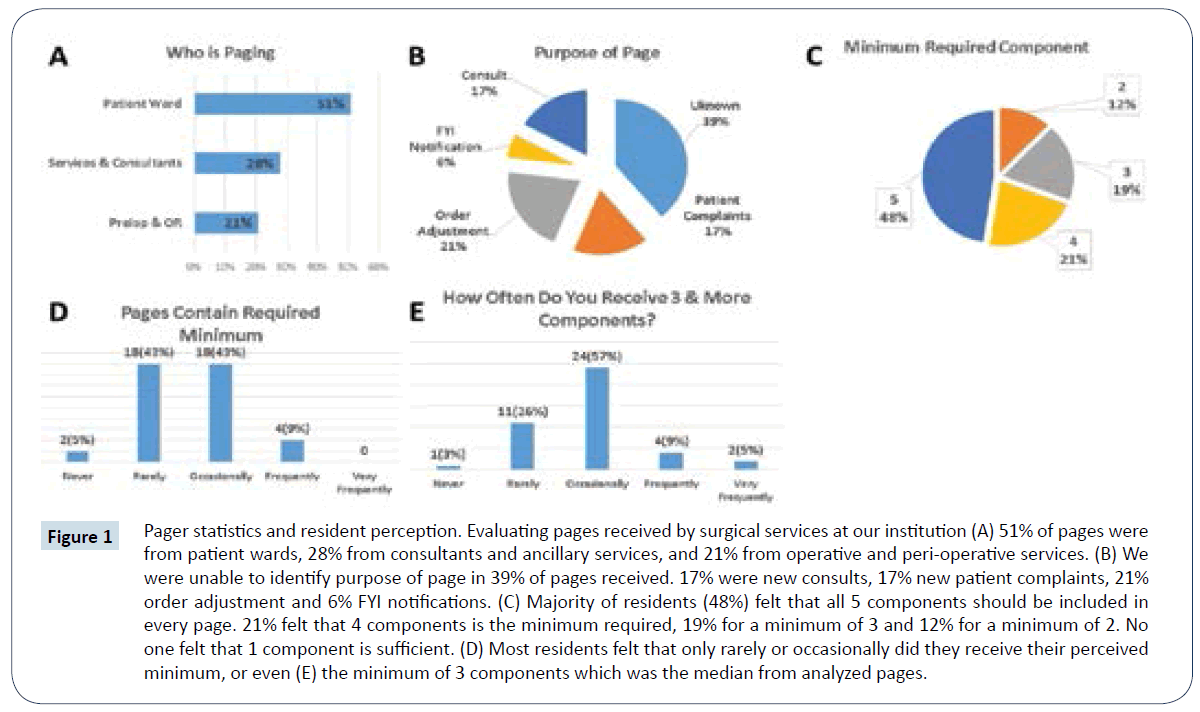
Records of 126 messages were obtained from our communication department from seven service pagers over a period of 24 hours. Of these pages 97% contained a call back number, 60% a patient identifier, 56% the complaint or reason for page, 52% the paging party and only 24% mentioned urgency. Per page, 32% contained only one of the five components, 9% two, 19% three, 20% four and 20% all five, with a mean and median of 3 components per page. The majority of pages (61%) were sent during the am shift with 51% sent by patient wards, 28% by consulting and ancillary services and 21% by the operative room and perioperative services (Figure 1A). The abundance of callback number only pages has also resulted in 39% of pages with no identifiable purpose as shown in (Figure 1B).
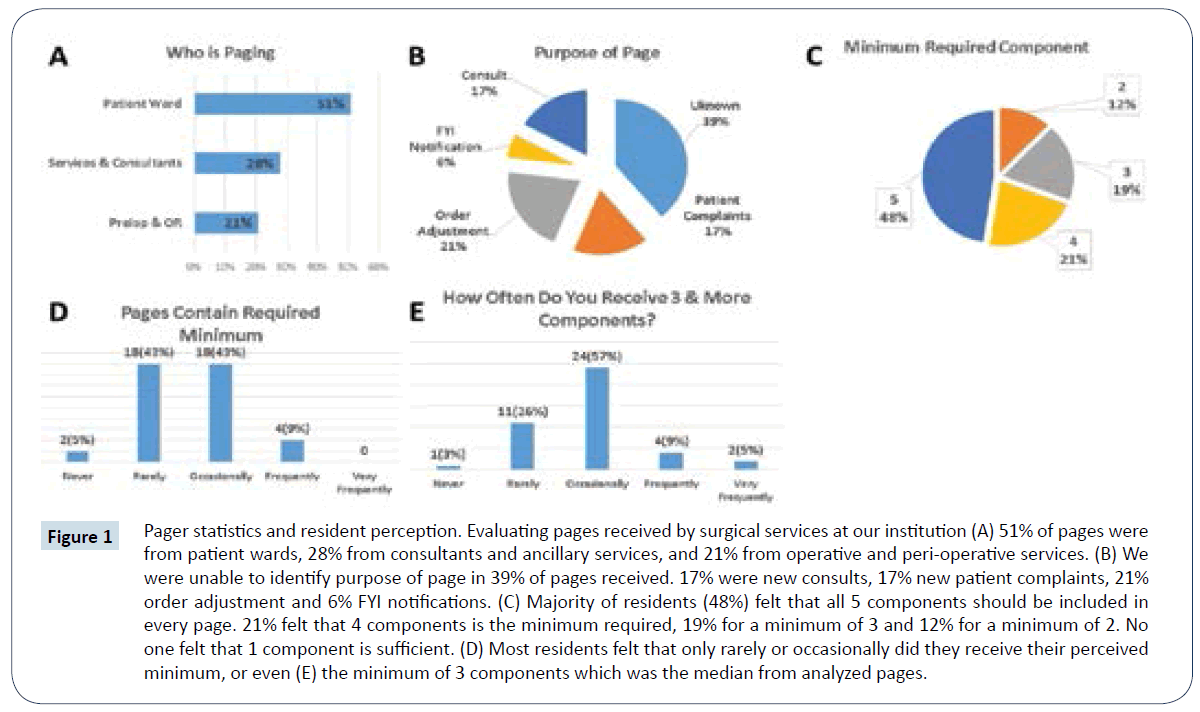
Figure 1: Pager statistics and resident perception. Evaluating pages received by surgical services at our institution (A) 51% of pages were from patient wards, 28% from consultants and ancillary services, and 21% from operative and peri-operative services. (B) We were unable to identify purpose of page in 39% of pages received. 17% were new consults, 17% new patient complaints, 21% order adjustment and 6% FYI notifications. (C) Majority of residents (48%) felt that all 5 components should be included in every page. 21% felt that 4 components is the minimum required, 19% for a minimum of 3 and 12% for a minimum of 2. No one felt that 1 component is sufficient. (D) Most residents felt that only rarely or occasionally did they receive their perceived minimum, or even (E) the minimum of 3 components which was the median from analyzed pages.
The Fischer’s Exact Test was used to evaluate which factors predicted higher likelihood of getting at least the median number of components in a single page. Surgical service and am versus pm shift did not significantly predict the event of such a page. However, when receiving a page from a consulting service versus ward services, there was a six time higher odds to get such a page (OR: 6 [CI 95%; (1.9-18.2) p-value<0.01).
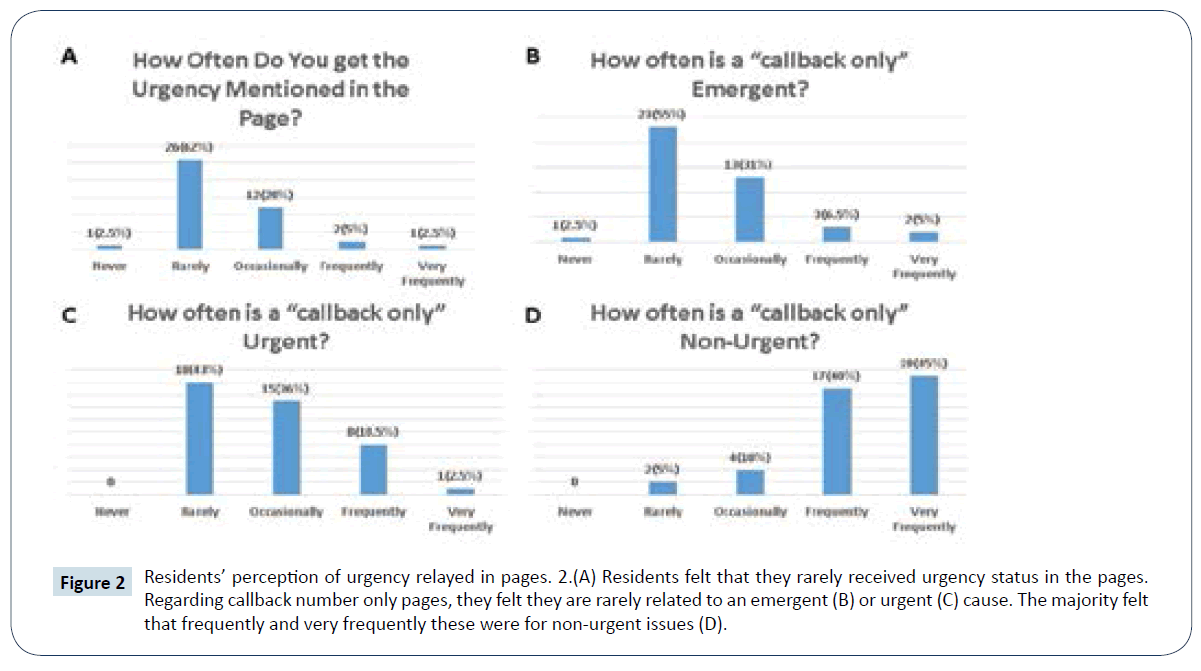
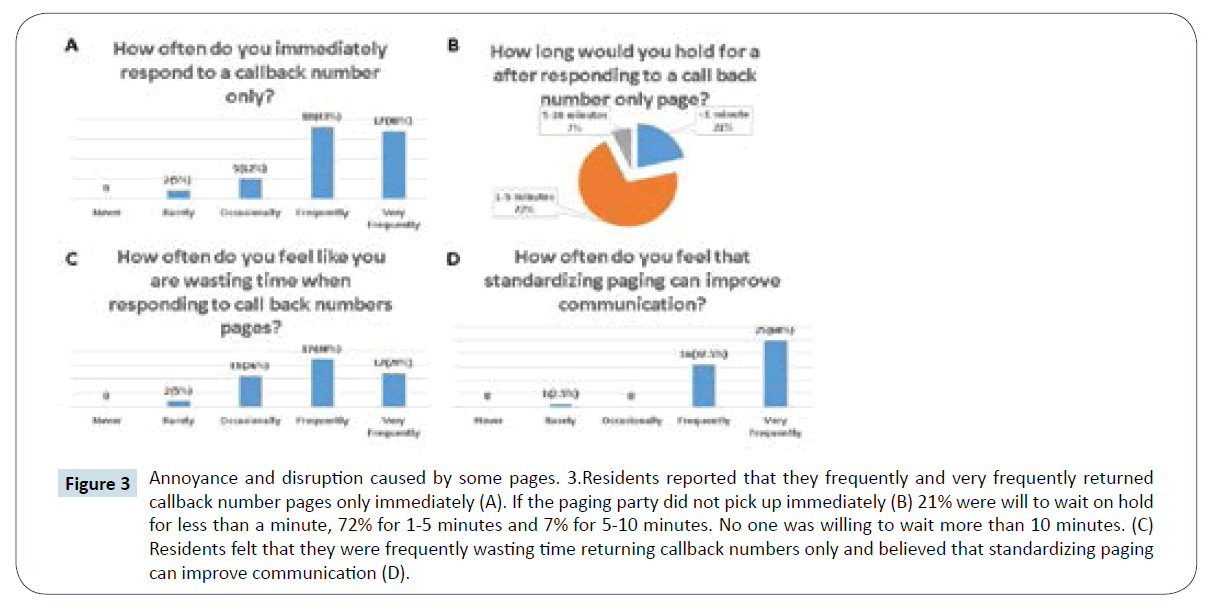
A survey was distributed to the residents in our general surgery program (Appendix 1). Forty-two residents completed and returned the survey (79%). The majority felt that the minimum required components should be five, and none felt that one component alone is enough (Figure 1C). The majority also felt that they rarely or occasionally received pages with their designate minimum (Figure 1D) as well as the minimum of three components (Figure 1E). They accurately predicted that they rarely received the urgency in the text pages (Figure 2A). Regarding the perceived urgency of a callback number only pages, the majority of residents agreed that it is rarely emergent (Figure 2B), rarely or occasionally urgent (Figure 2C) but frequently and very frequently non-urgent (Figure 2D). Despite majority of residents immediately returning the call for a number only page (Figure 3A), only 7% would stay on hold for five or more minutes if the paging party does not pick up (Figure 3B). This has led the majority to frequently and very frequently feel that they are wasting time returning such pages (Figure 3C). As such, residents unanimously felt that standardizing paging requirements would improve the quality of communication (Figure 3D). In addition, 74% felt strongly about changing the mechanism of paging to require a minimum component requirement. There were no differences among resident clinical years or gender.
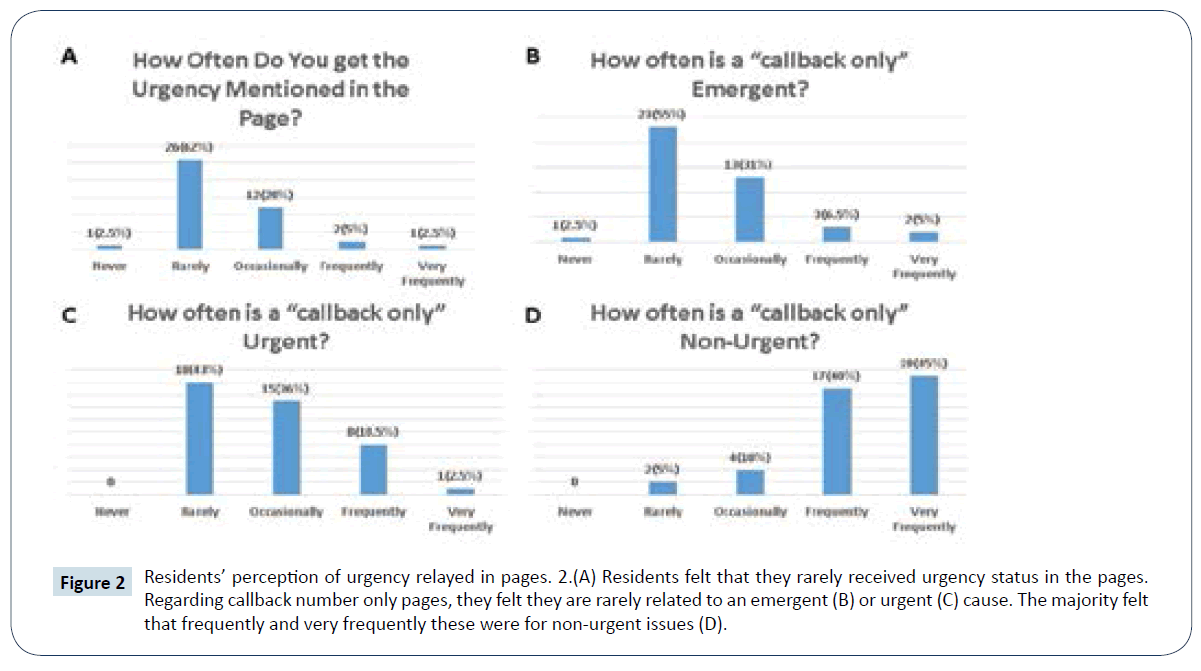
Figure 2: Residents’ perception of urgency relayed in pages. 2.(A) Residents felt that they rarely received urgency status in the pages. Regarding callback number only pages, they felt they are rarely related to an emergent (B) or urgent (C) cause. The majority felt that frequently and very frequently these were for non-urgent issues (D).
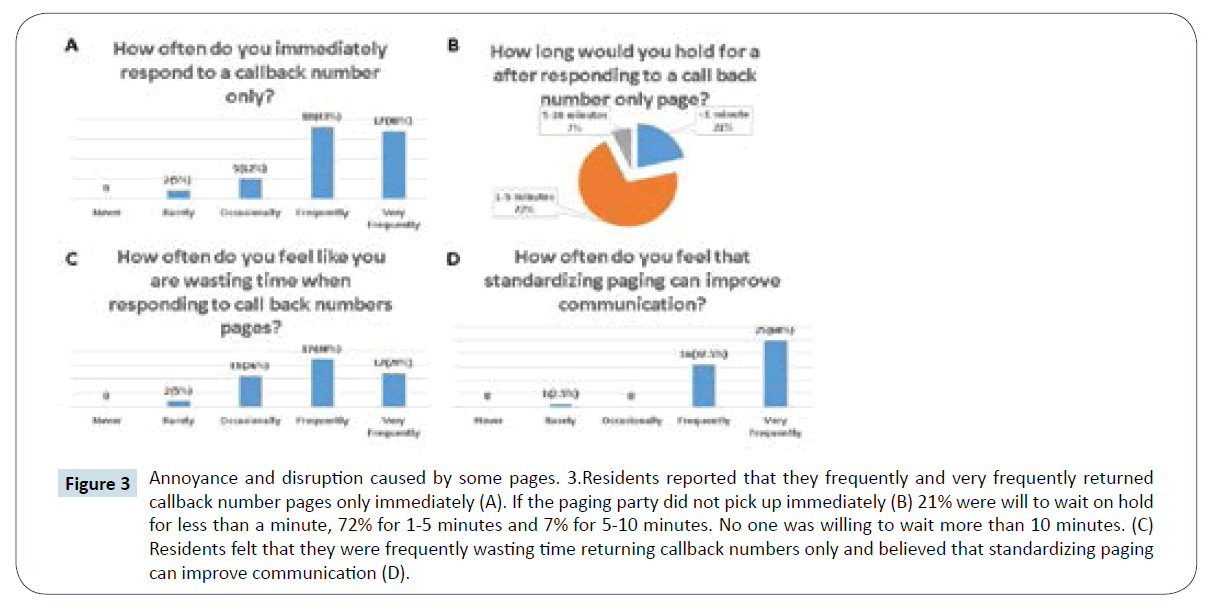
Figure 3: Annoyance and disruption caused by some pages. 3.Residents reported that they frequently and very frequently returned callback number pages only immediately (A). If the paging party did not pick up immediately (B) 21% were will to wait on hold for less than a minute, 72% for 1-5 minutes and 7% for 5-10 minutes. No one was willing to wait more than 10 minutes. (C) Residents felt that they were frequently wasting time returning callback numbers only and believed that standardizing paging can improve communication (D).
Discussion
In the late nineteen-thirties, Charles Neergaard, a radio engineer, was a patient in one of New York City’s hospitals [1]. He recalls the disruptive overhead pages for in-house physicians and thought that there must be a better way. He later went on to utilize his experience in radio-engineering to bring the pager into hospital systems. Hospitals embraced this technology, reporting less disruptive overhead pages, almost instantaneous return of pages and cleared switch boards for other phone calls [2-4].
Since then, the pagers have advanced to include new features including alphanumeric paging and 2-way messaging [4-6]. Some have reported improved communications between healthcare providers due to ability to send an alert as soon as possible. Others were skeptical, contending that paging callback numbers only would be a source of interruption to the normal work flow of both senders and recipients [5]. Driven by the prevalence of smartphones among healthcare providers, several centers have explored replacing the paging system with secure phone messaging and reported positive outcomes in ease of communication and response without interruption of workflow [7-11].
In our hospital, we have shown that the backbone of communication with residents remains the paging system. Within this framework, a substantial minority of pages include only a callback number. We identified five elements that would constitute an optimal alert, and these five elements were rarely all included in a message. In combination with the ease of communication outside of the hospital, a survey distributed to surgery residents showed a high degree of frustration and dissatisfaction with the current state of paging.
Based on our findings from pager logs and resident perception, we believe that standardizing alphanumeric paging to include the five identified components may improve both communication via the pager and resident workflow. This can be achieved by simply having required fields on the paging webpage prior to sending out a message. In addition, operators would require to fill these requirements prior to sending out pages and eliminating the option for callback number only.
Our study is subject to several limitations. The analysis was conducted at a single university-based academic medical center. The primary data was collected over a single twenty-four hour period, which may not be representative of the system as a whole. Our quality metrics were selected based on resident experience, but have not been validated as an objective measure of essential information. Last, our survey instrument is limited by recall bias and the inherent subjectivity of survey responses.
Quality of communication in healthcare is essential for providing proper and timely patient care, in addition to transfer of information. With the available technology in our time, we should thrive to optimize this service and eliminate any source of disruption to an already busy workflow. This may mean continued upgrading of the already existent pager system or introduction of a secure messaging application to the almost ubiquitous smartphones amongst providers.
Conclusion
More than half a century has passed since the introduction radio paging into healthcare. Hospitals, healthcare providers and communication technology have all evolved since then and so must the pager. Improving the quality of communication amongst healthcare providers and ancillary services is a must to be able to provide appropriate care and eliminate frustration in a busy work environment. With the technologies available to us nowadays, we must focus on improving the quality of communication in hospitals.
References
- Neergaard CF (1952) Radio paging goes into the doctor’s pocket. Mod Hosp 79: 122-126.
- Edwards V, Hatfield JN (1957) This Chicago hospital’s paging system does two jobs. Hospitals 31: 46-47.
- Tate KE, Gardner RM, Scherting K (1995) Nurses, pagers, and patient-specific criteria: three keys to improved critical value reporting. Proc Annu Symp Comput Appl Med Care: 164-168.
- Eisenstadt SA, Wagner MM, Hogan WR, Pankaskie MC, Tsui FC, et al. (1998) Mobile workers in healthcare and their information needs: are 2-way pagers the answer? Proc AMIA Symp 2: 135-139.
- Espino S, Cox D, Kaplan B (2011) Alphanumeric paging: A potential source of problems in patient care and communication. J Surg Educ 68: 447-451.
- Wu RC, Lo V, Morra D, Wong BM, Sargeant R, et al. (2013) The intended and unintended consequences of communication systems on general internal medicine inpatient care delivery: a prospective observational case study of five teaching hospitals. J Am Med Inform Assoc 20: 766-777.
- Joseph B, Pandit V, Khreiss M, Aziz H, Kulvatunyou N, et al. (2013) Improving communication in level 1 trauma centers: replacing pagers with smartphones. Telemed J E Health 19: 150-154.
- Przybylo JA, Wang A, Loftus P, Evans KH, Chu I, et al. (2014) Smarter hospital communication: Secure smartphone text messaging improves provider satisfaction and perception of efficacy, workflow. J Hosp Med 9: 573-578.
- Herrod PJJ, Barclay C, Blakey JD (2014) Can mobile technology improve response times of junior doctors to urgent out-of-hours calls? A prospective observational study. QJM 107: 271-276.
- Ferguson A, Aaronson B, Anuradhika A (2016) Inbox Messaging: an effective tool for minimizing non-urgent paging related interruptions in hospital medicine provider workflow. BMJ Qual Improv Rep 5: 1-5.
- Patel B, Johnston M, Cookson N, King D, Arora S, et al. (2016) Interprofessional communication of clinicians using a mobile phone app: a randomized crossover trial using simulated patients. J Med Internet Res 18: e79.