Research Article - (2025) Volume 11, Issue 1
Quality Improvement Project on Surgical Site Infections in Resource Limited Setup, Tibebe Ghion Specialized Hospital Department of Surgery, Bahir Dar, Ethiopia
Eyuel Behailu1*,
Abera Biadgo2,
Abebe Assaye1,
Teketay Siraj3 and
Daniel Atinaf3
1Department of General Surgeon, BahirDar University, Bahir Dar, Ethiopia
2Department of Public Health, Ethiopia’s Institute for Healthcare Improvement, IHI, Ethiopia
3Department of Nurse, BahirDar University, Bahir Dar, Ethiopia
*Correspondence:
Eyuel Behailu, Department of General Surgeon, BahirDar University, Bahir Dar,
Ethiopia,
Email:
Received: 11-Mar-2024, Manuscript No. IPJPIC-24-19165 ;
Editor assigned: 13-Mar-2024, Pre QC No. IPJPIC-24-19165 (PQ);
Reviewed: 27-Mar-2024, QC No. IPJPIC-24-19165 ;
Revised: 24-Mar-2025, Manuscript No. IPJPIC-24-19165 (R);
Published:
31-Mar-2025, DOI: 10.36648/2572-0376.10.1.37
Abstract
Background: Tibebe Ghion specialized hospital is one of the teaching hospitals found in Amhara regional state capital, BahirDar, North West Ethiopia started functioning since October 2018 G.C. It gives full range of clinical service of specialty and sub specialty cares. It has 10 OR tables, 126 and above outpatient rooms, 459 inpatient beds, with 2 dedicated intensive care units. SSI threatens the lives of millions of patients each year and also contributes to the spread of antibiotic resistance. Surgical site infections are commonest nosocomial infections and responsible for considerable morbidity and mortality as well as increased hospitalizations and treatment cost related to surgical operations. The aim of this QI project is to decrease the rate of SSIs.
Methods: Facility level QI project underwent using ‘model for improvement method’ aiming to decrease the rate of SSIs. Baseline data’s collected, fish bone analysis used for identification of the root causes and checklists are prepared and registered as clinical bundle indicators using Microsoft Excel. Interpretations are made through run charts, association of the outcome with the change ideas are assessed using scatter plot.
Result: Rate of SSIs was 25% at the beginning, which has shown a significant decrement to 10% by the end of the study period (August 2021 G.C). This was achieved by setting change ideas, running it through PDSA cycles (4 cycles). Initially, it was 40% and it became 80% by the end of the study.
Conclusion: This study demonstrated effective ways of decreasing SSIs by a comprehensive well designed QI project.
Keywords
QI project; Surgical Site Infections (SSI); Antibiotic resistance; Patient safety
Introduction
Bain metastases are a significant reason for mortality in bosom cancer [1]. The cerebrum is the primary site of metastasis from bosom disease in 12% of patients. Metastatic bosom malignant growth (BC) is, after cellular breakdown in the lungs, the second most normal disease related with cerebrum metastases. As malignant growth research leap forwards significantly further developed endurance of patients with cutting edge stage BC somewhat recently, the frequency of BMs is expanding accordingly [2]. It has been recommended that cerebrum metastases from bosom disease (BMBC) happen all the more habitually among more youthful ladies, those with bigger cancers or higher atomic grade, in certain subtypes like estrogen-receptor (trama center)-negative and HER2 overexpressing cancers, and those with nodal metastases [3].
Surgical Site Infections (SSI) is infections that occur at or near surgical incision within 30 days of operation or after 1 year if implant is placed [1,2]. It is the 3rd commonly reported nosocomial infection accounting for 10 to 40% of all nosocomial infections [3,4]. In low and middle-income countries, 11% of patients who undergo surgery are infected in the process [5]. In Africa, surgical site infections were the leading infections in hospitals (pooled cumulative incidence of 5.6 per 100 surgical procedures), strikingly higher than proportions recorded in developed countries [6]. Another study done in Africa indicated cumulative incidence of SSIs ranged from 2.5 to 30.9% [7]. SSI is the most costly HAI type with an estimated annual cost of $3.3 billion, and extends hospital length of stay by 9.7 days, with cost of hospitalization increased by more than $20,000 per admission [8-10]. Although high incidence of SSI is suspected in Ethiopia, the magnitude of the problem is not known; however, the overall SSI rate was reported to be 21% in general surgical wards of teaching hospitals [11].
Despite improvements in operating room practices, instrument sterilization methods, better surgical technique and the best efforts of infection prevention strategies, surgical site infections remain a major cause of hospital-acquired infections and rates are increasing globally even in hospitals with most modern facilities and standard protocols of preoperative preparation and antibiotic prophylaxis.
In response to inconsistent compliance with infection prevention measures, the centers for Medicare and Medicaid services collaborated with the U.S. centers for disease control and prevention on the Surgical Infection Prevention (SIP) project, introduced in 2002. Quality improvement measures were developed to standardize processes to increase compliance. In 2006, the Surgical Care Improvement Project (SCIP) developed out of the SIP project and its process measures. These initiatives published in the specifications manual for national inpatient quality measures, outline process and outcome measures [12]. This continually evolving manual is intended to provide standard quality measures to unify documentation and track standards of care. These measures included the timeliness, selection, and duration of peri-operative antibiotics. The investigators found both clinically and statistically significant reductions in postoperative infection rates after implementation of these measures [13]. However there is no international evidencebased guidelines had previously been available before WHO launched its global guidelines on the prevention of surgical site infection on 3 November 2016; there are inconsistencies in the interpretation of evidence and recommendations in existing national guidelines. These new WHO guidelines are valid for any country and suitable to local adaptations, and take account of the strength of available scientific evidence, the cost and resource implications, and patient values and preferences. Therefore, situation based interventions and region context specific preventive strategies should be developed to reduce the prevalence of SSIs among postop patients.
From our baseline study the rate of SSI at Tibebe Ghion Comprehensive Specialized Hospital (TGCSH) was 25 % which is very high when we compare it to the global and national level over all rates; results in increased morbidity, mortality, costs and hospital stay. The surgical QI team at TGCSH aimed to reduce the rate of SSIs from 25% to 12%, by implementing scientific recommendations: Appropriate use of antibiotics (prophylactic IV antibiotics within 1 hour before surgical incision, discontinuation within 24 hrs. post-surgery), early removal of transurethral catheter, avoid shaving, pre-op/ intraop shower for colorectal surgical pts and leaving skin incision open after operating on contaminated or dirty wounds. By applying these change ideas we hopped to decrease the rate of SSIs in our hospital.
Materials and Methods
Data Collection
Checklists are prepared which includes data’s for process measures as well as outcome measures. At the beginning of the study we have selected gastrointestinal surgical unit for the testing of our change ideas and weekly we planned to take 5 patients randomly and register them on the checklist and we will follow each pts for a month using phone calls for the occurrence of SSIs. Testing of Change ideas were done at different stages of the study and multiple PDSA cycles were allowed to run and the results are documented, studied and interpreted based on run chart rules for signs of improvement.
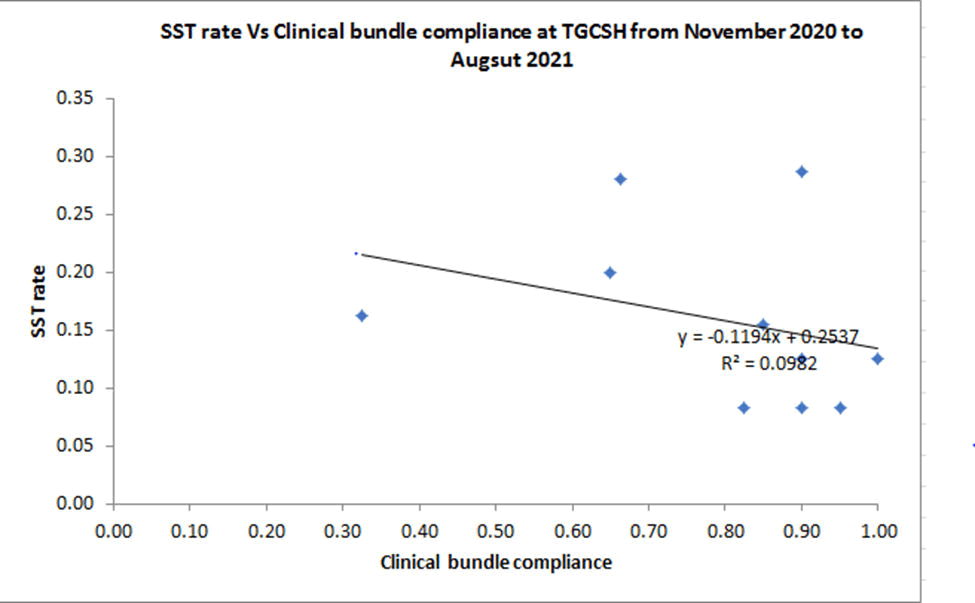
Data Analysis
We conducted scatter plot analysis for the effectiveness of the intervention. In the plot, we analyzed the effects of our clinical bundle indicators on the rate of SSIs and we have noticed an association though it’s a weak association.
Results
Quantitative results
Testing and run charts
Cycle I of the PDSA
Testing → testing has carried out in surgical ward mainly in GI and HPB ward since we wanted to start testing in small scale.
A 2 months study with active surveillance for the occurrence of SSIs is done primarily by phone calls.
Change ideas and activities carried out (using check lists)
- Antibiotics given within 1hr of surgical incision time.
- Prophylactic Antibiotics discontinued within 24 hrs.
- Catheter removal within 24-48hrs post op.
Data’s are collected weekly and patients are followed until the 30th post op day.
Process indicator and outcome indicators are set and we expected an initial increment from the base line rate of SSIs.
Process indicator: Adherence to the protocol/change ideas– mentioned above.
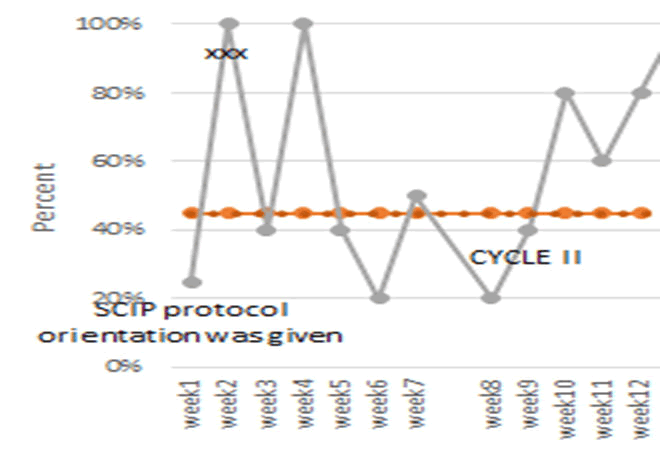
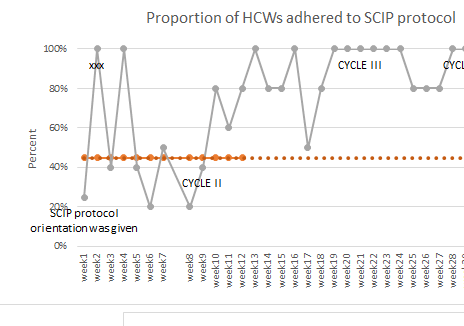
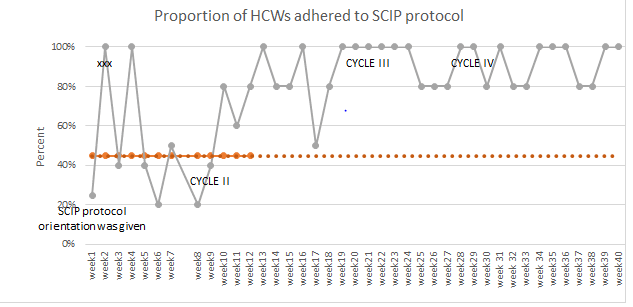
Run chart: On process indicator-40% achievement adherence to the activities (the SCIP process indicators) (Figure 1).
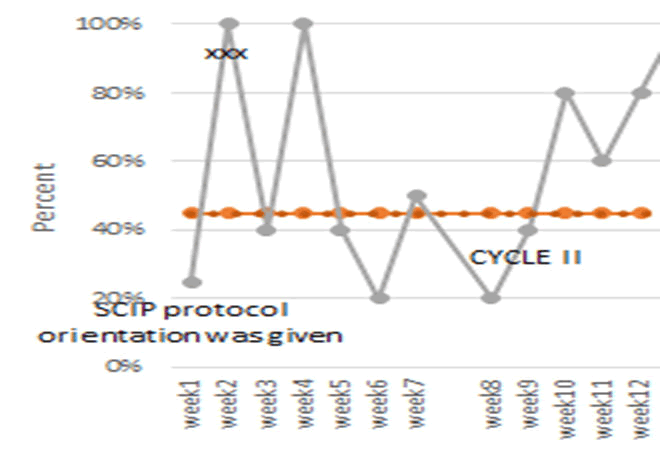
Figure 1: Proportion of HCWs adhered to SCIP protocol.
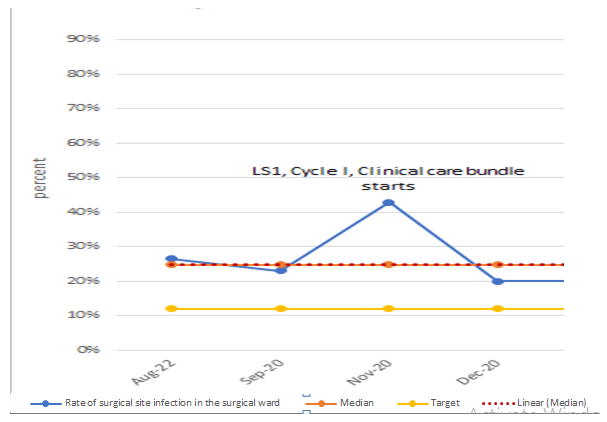
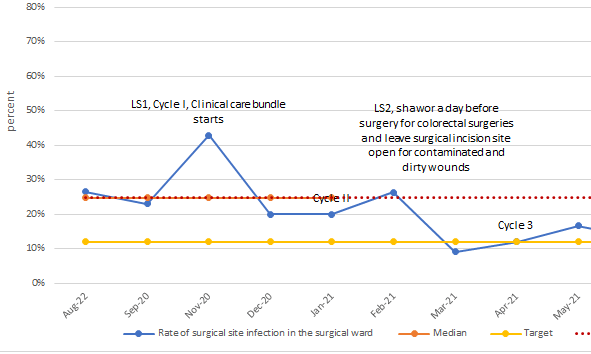
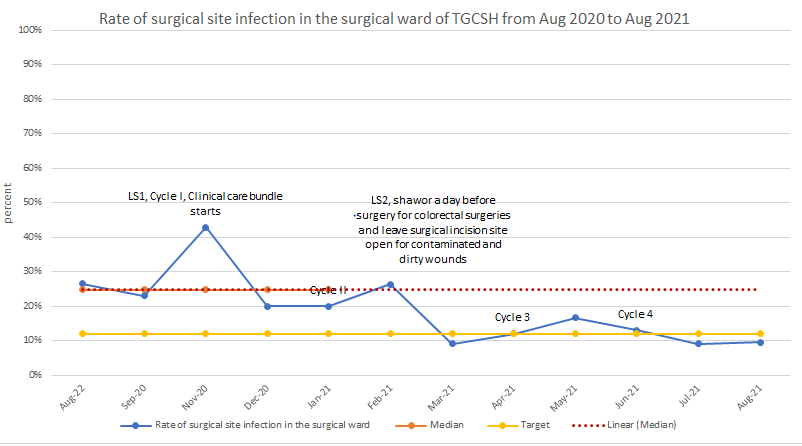
Outcome indicator-Rate of SSIs Has become 43% and 20% in Nov 2020 and Dec-2020 respectively (We predicted an initial increment due to an active detection) (Table 1 and Figure 2).
Run chart–on outcome indicator-Rate of SSIs.
| Note/Annotation |
LS1, Cycle I, Clinical C |
| Month |
Aug-22 |
Sep-20 |
Nov-20 |
Dec-20 |
| Number of inpatients with new surgical |
9 |
9 |
6 |
4 |
| Number of major surgeries |
34 |
39 |
14 |
20 |
| Rate of surgical site infection in the surgeries |
26% |
23% |
43% |
20% |
| Median |
25% |
25% |
25% |
25% |
| Target |
12% |
12% |
12% |
12% |
Table 1: Rate of Surgical site infections in surgical ward of TGCSH from Aug 2020 to Dec 2020.
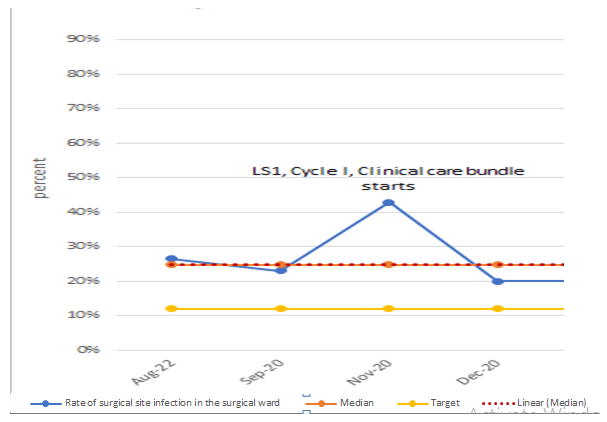
Figure 2: Rate of surgical site infections in surgical ward of TGCSH from Aug 2020 to Dec 2020.
Cycle II of the PDSA
The previous process measures/change ideas adapted, and addition of a new change idea “avoiding shaving of surgical site” was incorporated in our study.
General surgical cases are selected randomly from the surgical ward and the cycle has rolled for 3 months (Jan 2021 to Mar 2021).
A minimum of 5 patients (both emergency and elective) are selected randomly from the general surgical ward.
Training is given for surgeons, residents and ward nurses where we are going to introduce the change ideas.
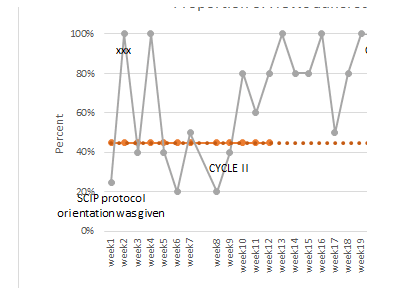
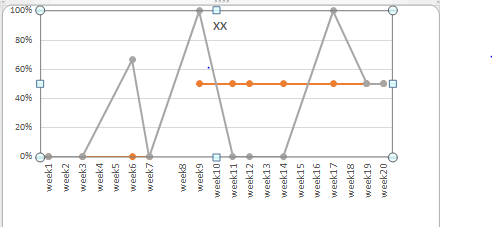
Process indicator and outcome indicators are set and we expected a decrement in the rate of SSIs with a target to reach 12% (Figure 3).
Process indicator-Adherence to SCIP protocol–adopted measurements with addition of one new measure (avoiding shaving of surgical site).
Run chart–on process indicator- significant improvement on health workers adherence to the change ideas (SCIP) were achieved.
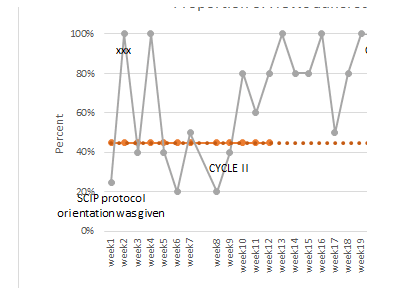
Figure 3: Adherence to the change ideas.
It shows there is a shift in process measures → sign of improvement.
Run chart on outcome indicator-Rate of SSIs (Table 2).
| Note/Annotation |
|
|
LS 1, Cycle I, Clinical C |
Cycle II |
|
LS2 |
| Month |
Aug-22 |
Sep-20 |
Nov-20 |
Dec-20 |
Jan-21 |
Feb-21 |
Mar-21 |
| Number of inpatients with new surgical |
9 |
9 |
6 |
4 |
4 |
5 |
2 |
| Number of major surgeries |
34 |
39 |
14 |
20 |
20 |
19 |
22 |
| Rate of surgical site infection in the surgeries |
26% |
23% |
43% |
20% |
20% |
26% |
9% |
| Median |
25% |
25% |
25% |
25% |
25% |
|
|
| Target |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
Table 2: Rate of surgical site infections in surgical ward of TGCSH from Jan 2021 to Mar 2021.
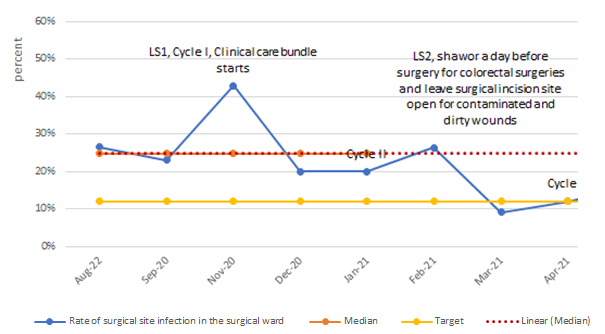
The rate was 20%, 26% and 9% on January, February and March 2021 respectively. The graph starts to show decrement in the rate of SSIs (Figure 4).
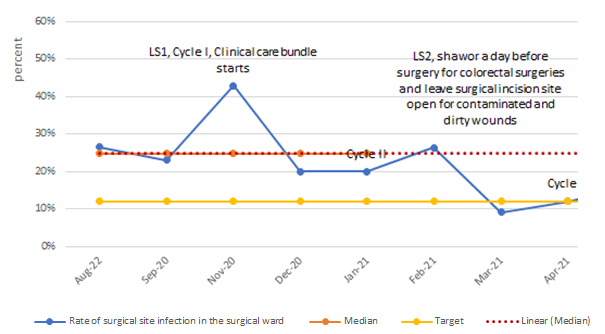
Figure 4: Rate of surgical site infections in surgical ward of TGCSH from Jan 2021 to Mar 2021.
Cycle III
The previous process measures/change ideas are adapted and addition of new change ideas as a new clinical bundle developed.
Pre-op shower or abdominal wash with soap for colorectal surgical pts before the surgical procedure.
New clinical bundles leaving skin open (incision site) in contaminated and dirty wounds, e.g. periappendical abscess.
Awareness creation regarding the additional intervention measures for the health care providers (communicated through the department telegram page and also verbally).
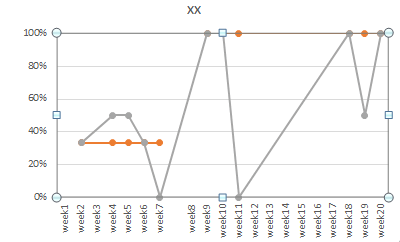
Each week general surgical cases are selected randomly from the same ward and the cycle has rolled for 2 months (Apr 2021 to May 2021) (Figure 5-7).
Process indicator-Adherence to SCIP protocol–adapted measurements with addition of two new measures.
Run chart–on process indicators the previous improvement noticed on the process measures are maintained.
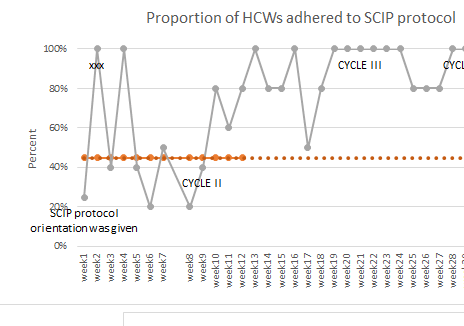
Figure 5: Adherence to the change ideas.
Figure 6: Run chart regarding adherence to Pre-op shower for colorectal surgeries
Figure 7: Run chart regarding adherence to leaving skin open for contaminated and dirty wounds
Outcome indicator
Run chart–on outcome indicator- Rate of SSIs (Table 3).
| Note/Annotation |
|
|
LS1, Cycle I, Clinical C |
Cycle II |
|
LS2 |
Cycle 3 |
|
| Month |
Aug-22 |
Sep-20 |
Nov-20 |
Dec-20 |
Jan-21 |
Feb-21 |
Mar-21 |
Apr-21 |
May-21 |
| Number of inpatients with new surgical |
9 |
9 |
6 |
4 |
4 |
5 |
2 |
3 |
4 |
| Number of major surgeries |
34 |
39 |
14 |
20 |
20 |
19 |
22 |
25 |
24 |
| Rate of surgical site infection in the surgeries |
26% |
23% |
43% |
20% |
20% |
26% |
9% |
12% |
17% |
| Median |
25% |
25% |
25% |
25% |
25% |
|
|
|
|
| Target |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
Table 3: Rate of surgical site infections in surgical ward of TGCSH from Apr 2021 to May 2021.
The rate has become 12% and 17% on April and May 2021 respectively. The decrement in the rate may be due to increased adherence and addition of important change ideas (Figure 8).
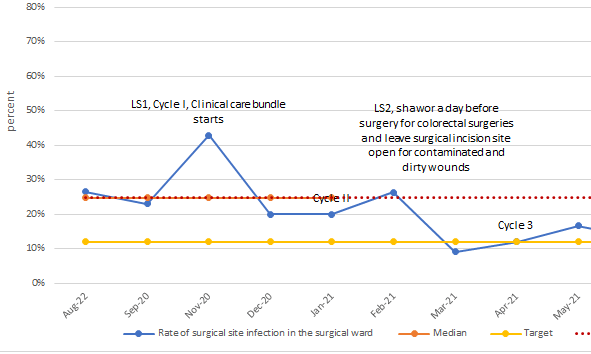
Figure 8: Rate of Surgical site infections in surgical ward of TGCSH from April 2021 to May 2021.
Cycle IV
All the previous 6 change ideas are adapted and carried out at cycle IV.
General surgical cases are randomly selected from a same ward and the cycle has rolled for 3 months (June 2021 to August 2021).
At least 5 patients (both emergency and elective) are selected randomly.
Process indicator and outcome indicators are set. And we expected a further decrement in the rate with a target to reach 12% (Figure 9).
Process indicator-Adherence to SCIP protocol.
Run chart-on process indicators (June 2021 to August 2021).
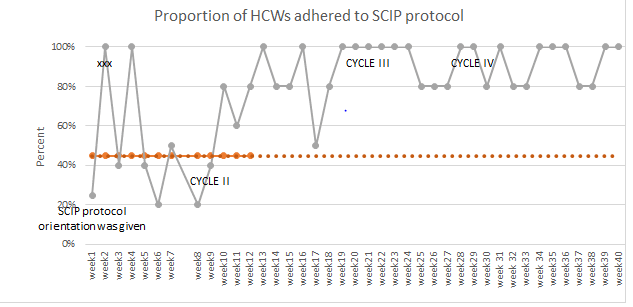
Figure 9: Adherence to the change ideas.
Process indicators–adherence to the new clinical bundles (Figures 10 and 11).
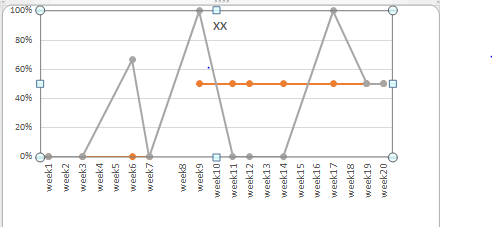
Figure 10: Run chart regarding adherence to Pre-op shower for colorectal surgeries.
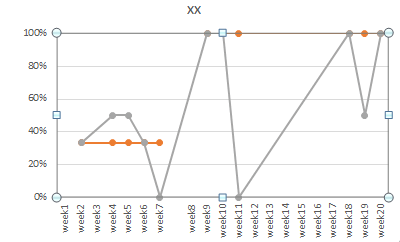
Figure 11: Run chart regarding adherence to leaving skin open for contaminated and dirty wounds.
Outcome indicator
Run chart–on outcome indicator-Rate of SSIs (Table 4).
| Note/Annotation |
|
|
LS1, Cycle |
Clinical C |
Cycle II |
|
LS2, shawo |
Cycle 3 |
|
Cycle 4 |
|
|
| Month |
Aug-22 |
Sep-20 |
Nov-20 |
Dec-20 |
Jan-21 |
Feb-21 |
Mar-21 |
Apr-21 |
May-21 |
Jun-21 |
Jul-21 |
Aug-21 |
| Number of inpatients with new surgical |
9 |
9 |
6 |
4 |
4 |
5 |
2 |
3 |
4 |
3 |
2 |
2 |
| Number of major surgeries |
34 |
39 |
14 |
20 |
20 |
19 |
22 |
25 |
24 |
23 |
22 |
21 |
| Rate of surgical site infection in the surgeries |
26% |
23% |
43% |
20% |
20% |
26% |
9% |
12% |
17% |
13% |
9% |
10% |
| Median |
25% |
25% |
25% |
25% |
25% |
|
|
|
|
|
|
|
| Target |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
12% |
|
Table 4: Rate of surgical site infections in surgical ward of TGCSH from June 2021 to August 2021.
The rate has become 13%, 9% and 10% on June, July and August 2021 respectively. The decrement in the rate may be due to increased adherence to the change ideas (Figure 12).
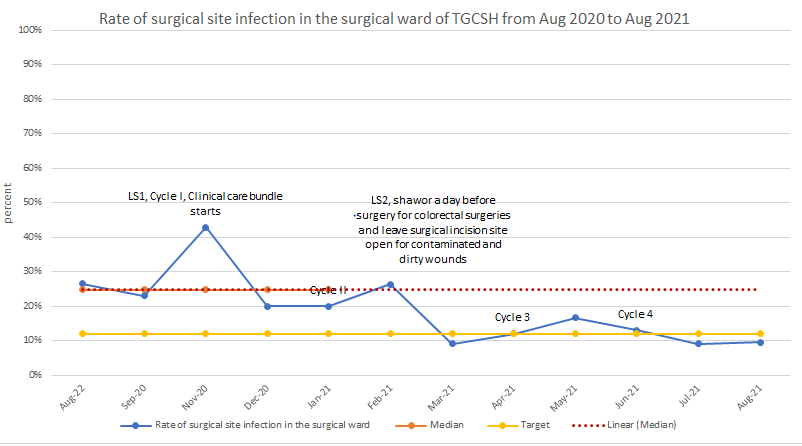
Figure 12: Rate of surgical site infections in surgical ward of TGCSH from June 2021 to August 2021.
This has shown a shift in the rate of SSIs → sign of improvement (Figure 13).
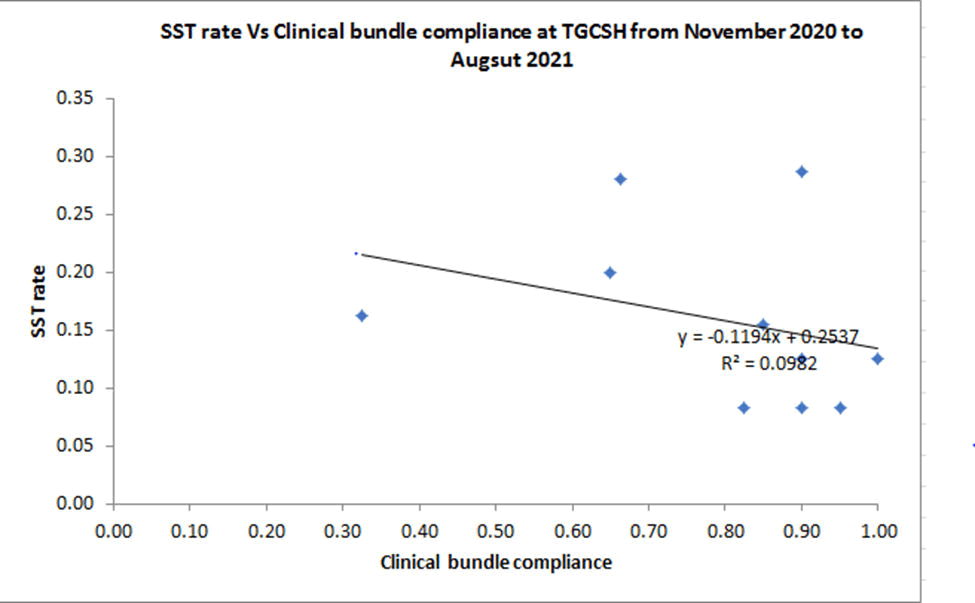
Figure 13: Scatter plot analysis- the r/n ship b/n the change ideas and the rate of SSIs.
It shows an association b/n the change ideas (1st clinical bundle) and the rate of SSIs though it’s a weaker association.
Discussion
We conducted our study at facility level for 12 months and noted a significant decrement in the rate of SSIs by the end of the project August 2021. Initially at the beginning of the study from October 2020 to December 2020, we have conducted our intervention (PDSA cycle I) in a selected set of patients and at specific ward (GI and HPB ward) where there is a few health care providers involved. After creating awareness verbally with the stake holders we went to implement the change ideas at that specific ward but due to the complexity of the procedure done at this wards, elderly pts with comorbidity, few number of pts operated per week, lengthy preoperative stay in the wards and poor adherence to the change ideas, we didn’t get a result as we want it to be, so we have learned from this and in cycle II we have changed the ward to general surgical ward specifically ward B, where the above challenges are minimal and in addition to that a formal 2 days training has given to health care providers working in that ward (nurses, surgical residents and senior surgeons working in the mentioned ward). From Jan 2021 to Mar 2021 a 3 month study was conducted with ‘adaption’ of the previous change ideas with addition of a new change idea; that is ‘avoid shaving at incission site’.
The adeherence to the change ideas shows a shift in the run chart graph which indicates a sign of improvement- proper implementation of change ideas. Also the rate of SSIs starts to show some decrement on the run chart graph but didn’t achieve its target. Then we continued our study with ‘adaption’ of the newly added change ideas and introduced a another change ideas at the commencement of new cycle that is PDSA Cycle III, these new change ideas showed high proportion (81.8 %) of SSIs is contributed by either colorectal surgeries or emergency surgeries with a class of wound as contaminated or dirty surgical wounds.
Adherence was high to the previous process measures but regarding the newly introduced change ideas like; pre-op shower and leaving skin wounds open for wound care in contaminated or dirty wounds were not as expected. Especially the challenge to implement pre-operative shower in our set up was due to dysfunctional bath rooms, so we started to do intraoperative abdominal bathing instead, for colorectal surgical pts. The rate of SSIs was continually decreasing and the run chart shows the line going down below the mean level. Then due to the fact that we have noticed a positive results from the previous process indicators we further conducted our study with ’adaption’ of the measures and a new PDSA cycle (Cycle IV) has allowed to run for subsequent months and the rate of SSIs has showed a significant decrement by the end of the study period-August 2021. A ‘Shift’ on the run chart graph has been noticed so; by definition this is a sign of improvement.
Conclusion
If there is a commitment and dedication to bring quality of care to our pts and also a culture of learning from the mistakes we make while performing the project, we can achieve what we wanted to see even in resource limited set ups . We have identified the true or the actual rate of surgical site infections in our set up for the first time. Our plan is to publish and also distribute our study findings nationally as well as to the international level by that we can assure a sustainable implementation of the findings.
Due to the lack of sufficient data points on the newer ‘clinical bundle change ideas’ we failed to do a scatter plot analysis regarding the association of this change ideas and the rate of SSIs. And also the limit of the generalizability of this study is, it was conducted in a small number of pts, at specific ward and only general surgical pts excluding pts like orthopedic, gynecologic or other sub specified surgical fields, but it has still be a significant entry point for large scale studies.
Recommendation
Continuous support for quality improvement projects by the governing body is needed.
Strict follow up of scientific recommendation and evidence based medicine are very crucial in decreasing SSIs.
To establish basic infrastructure works in the hospital that helps to improve quality of care to surgical pts- e.g. to establish bathrooms in the wards, well ventilated OR rooms, AC machines in the OR, Glucometer, thermometer, etc. to further decrease the rate of SSIs.
Creating awareness and proper trainings on scientifically recommended infection prevention strategies.
Acknowledgements
The authors would like to express due appreciation for BahirDar University Tibebe Ghion Comprehensive specialized Hospital for allowing us to access patients data. We are also grateful to IHI, Ethiopia for providing us different reference materials and continuous supervisions and support.
Funding
No specifically allocated fund for this project.
Availability of Data and Materials
The datasets during are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Consent for Publication
Not applicable.
References
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, et al. (1999) Guideline for prevention of surgical site infection, 1999. Am J Infect Control. 20(4):247-280.
[Google Scholar] [PubMed]
- Tietjen L, Bossemeyer D, McIntosh N (2003) Infection prevention: Guidelines for healthcare facilities with limited resources. Jhpiego Corporation.
- Singh R, Singla P, Chaudhary U (2014) Surgical site infections: Classification, risk factors, pathogenesis and preventive management. Int J Pharm Res Health Sci. 2(3):203-214.
- AlanR S, Kavitha C (2011) Antibiotic prophylaxis to prevent surgical site infection. Am Fam Physician. 83(5):585-590.
- World Health Organization (2016) Global guidelines for the prevention of surgical site infection: World Health Organization.
- Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, et al. (2011) Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. The Lancet. 377(9761):228-241.
[Crossref] [Google Scholar] [PubMed]
- Nejad SB, Allegranzi B, Syed SB, Ellis B, Pittet D. Health-care-associated infection in Africa: A systematic review. Bull World Health Organ. 89(10):757-765.
[Crossref] [Google Scholar] [PubMed]
- Ban KA, Minei JP, Laronga C, Harbrecht BG, Jensen EH, et al. (2017) American College of Surgeons and Surgical Infection Society: Surgical site infection guidelines, 2016 update. J Am Coll Surg. 224(1):59-74.
[Crossref] [Google Scholar] [PubMed]
- Awad SS (2021) Adherence to surgical care improvement project measures and post-operative surgical site infections. Surg Infect. 13(4):234-237.
[Crossref] [Google Scholar] [PubMed]
- Zimlichman E, Henderson D, Tamir O, Franz C, Song P, et al. (2013) Health care–associated infections: A meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 173(22):2039-2046.
[Crossref] [Google Scholar] [PubMed]
- Mulat Taye MT (2005) Wound infection in Tikur Anbessa Hospital, Surgical Department.
- Rosenberger LH, Politano AD, Sawyer RG (2011) The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect. 12(3):163-168.
[Crossref] [Google Scholar] [PubMed]
- Dellinger EP, Hausmann SM, Bratzler DW, Johnson RM, Daniel DM, et al. (2005) Hospitals collaborate to decrease surgical site infections. Am J Surg. 190(1):9-15.
[Crossref] [Google Scholar] [PubMed]
Citation: Behailu E, Biadgo A, Assaye A, Siraj T, Atinaf D (2025) Quality Improvement Project on Surgical Site Infections in Resource Limited Setup, Tibebe Ghion Specialized Hospital Department of Surgery, Bahir Dar, Ethiopia. J Prevent Infect Control. 11:37.
Copyright: © 2025 Behailu E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.