Research Article - (2015) Volume 1, Issue 1
Desalegn Asmare Eshetu1*, Solomon Meseret Woldeyohannes2, Melkam Alemayehu Kebede3, Gezahegn Nekatibeb Techane4, Kefyalew Dagne Gizachew5 ,Minale Tareke Tegegne6, Bereket Tsegaye Misganaw7
1Department of Psychiatry, DebreBerhan Referral Hospital, Debrebirhan, Ethiopia; desalegnasmare23@gmail.com
2Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
3Department of Psychiatry, Faculty of Medicine, Addis Ababa University, Addis Ababa, Ethiopia
4Department of Paediatrics and Child Health, DebreBerhan Referral Hospital, Debrebirhan, Ethiopia
5Department of Psychiatry, DebreBerhan Referral Hospital, Debrebirhan, Ethiopia
6Department of psychiatry, Bahir Dar University, Bahir Dar, Ethiopia
7Department of emergency medicine, DebreBerhan Referral Hospital, Debrebirhan, Ethiopia
Corresponding Author:
Desalegn Asmare Eshetu
Department of Psychiatry
DebreBerhan Referral Hospital, Debrebirhan, Ethiopia
Tel: 36 1 463 1111
E-mail: desalegnasmare23@gmail.com
Depression is one of the most common mental health disorders among people with HIV/AIDS. It causes more disability and greater decrements in health than most other chronic illnesses. Data was collected from April to May, 2013 after obtaining verbal consent from the respondents. Data entry was performed by using SPPSS version 20 and analysis was done using logistic regression and odd ratio. A total of 416 respondents were interviewed and of the 221(53.1%) were female, 385 (92.5%) were orthodox in religion, 184(44.2%) were married and 380(91.3%) were Amhara in ethnicity. 157(37.7%) were completed primary education and 106 (25.5%) were jobless. Monthly income of the respondents was between 401-700 birr for 108(26%). Among 416 participants 38.94% were depressed. Depression was associated with being Female(AOR=2.071(1.077,3.985),30-39years(A OR=2.761(1.165,6.540)), 449years(AOR=3.847(1.489,9.942), 60-69 years (AOR=19.645 (4.020, 95.991), income < 200birr’s (AOR=3.917(1.559, 9.845),201-400 birr’s (AOR=2.796(1.139, 6.865)), 401-700birr’s (AOR=2.590(1.058, 6.340), Stage III HIV/AIDS (AOR=2.317(1.108, 4.848)), Stage IV HIV/AIDS (AOR=8.769(1.928, 39.872), Hospitalized in the past one month was (AOR=15.262(1.463, 159.219) and felt stigmatized were (AOR=3.597(1.861, 6.954). This study summarizes that there is high prevalence of depression on people living with HIV/AIDS. Among them sex, age, low income, HIV/AIDS stages, hospitalized in the past one month, and perceived stigma were significantly associated. Screening programs should focus on being females, low incomes, HIV Stage III and IV, those hospitalized the last one month, and perceived stigma. We recommend health care providers to address depressive disorders for people with HIV/ AIDS comprehensively
Keywords
Depression; HIV/AIDS patients
Introduction
Study done in Brazil was the prevalence of depressive symptoms was 53.5% among the surveyed population, which supports the idea that depressive symptoms are more common among PLWHA, mainly if compared with the general population. It was observed that 57.7% of the study participants were with depressive symptoms and did not take any psychiatric medication and 100% did not undergo psychotherapy, which indicates under treatment (1). Study done in Delhi was the prevalence of depression in patients with HIV under ART was 58.75%. The prevalence of depression increased with the severity of symptoms. The unemployed, uneducated, unmarried, belonging to joint families, having no or low family income, migrants, having indifferent or poor relationship with spouse, poor social support and had visited commercial sex workers had a greater prevalence of depression. Moderate to severe depressive symptoms were reported by 17.3% of the HIV-infected patients with females reporting significantly higher levels of depressive symptoms than males. A principal components analysis identified three clusters of depressive symptoms: cognitive-affective, negative cognitions and somatic symptoms.
The HIV-infected patients were found to display mainly cognitiveaffective symptoms of depression. Another research shows that 42.4% had a depressive episode. Prevalence of MDE was significantly higher in HIV-affected than HIV-infected participants, Being female, receiving a government grant, urban residency and adult care-giving were significantly associated with any depressive episode. Participants with a depressive episode were 2–3 times more likely to report poor health perceptions. Studies done in Eastern Uganda were among 1017 HIV-infected participants assessed for depression, 47% (476/1017) reported depressive symptoms (CES-D ≥ 23). Adjusting for age, gender, education, and source of income, patients with CD4 counts <50 cells/μl were more likely to be depressed (odds ratio 2.34, 95% confidence interval, 1.39–3.93, P=0.001).
Another study showed that being in a current relationship was associated with lowered odds of depression (OR=0.43; CI=0.23−0.81). The factors strongly associated with increased odds of depression were a past history of illicit drug use (OR=2.98; CI=1.60−5.54) and a diagnosis of ‘stress’ by treating doctors (OR=5.65; CI=2.50−12.77). HIV-related medical variables such as immune function, use of antiretroviral medication and duration of HIV infection were not associated with depression.
In South Africa were One hundred forty-nine recently diagnosed HIV/AIDS patients. Three variables: gender (odd ratio [OR]=1.23; 95% confidence interval [CI] 1.56, 1.93), impact of negative life events (OR=1.13; CI, 1.03, 1.23), and disability (OR=1.51, CI, 1.28, 1.80) predicted current major depression. It is well known from non-HIV populations that female gender and increased negative life events predict depression. These data also emphasize the importance of these links in HIV. Institutional based crosssectional study done in Nigeria was the respondents, 39.91% were found to be depressed, with stage of the disease, inability to afford medication, unemployment, lack of social support, inability to tolerate HAART and other drugs in the management of HIV, and CD4 cell (Cluster of Differentiation 4 T-lymphocytes subgroup, the cells specifically targeted by HIV) count level found to be associated with depression (2-7).
Cross-sectional studies done Jamaica were Sixty-three patients participated in the study and 43% (n=36) of them were depressed. No significant differences in depression rates were found with respect to any of the sociodemographic or clinical factors explored (p>0.05)(9). Cross-sectional study showed that the prevalence of depression was 27.7%. The female gender (odds ratio [OR]=10.65; p=0.00586), a low CD4 count during the study (OR=1.005247; p=0.01539), and current smoking status (OR=12.89; p=0.01693) were independently associated with MD. Another study done in Cameroon was the prevalence of depressive symptoms was 63%.
Another study done in Uganda was Prevalence of major depressive disorder was 8.1%. Factors associated with major depressive disorder at univariate analysis only were female gender, family history of mental illness, negative coping style, alcohol dependency disorder, food insecurity and stress; not associated with MDD were social support, neurocognitive impairment, CD4 counts and BMI. Factors independently associated with MDD were psychosocial impairment, adverse life events, posttraumatic stress disorder, generalized anxiety disorder and lifetime attempted suicide. Cross-sectional studies done in south east Nigeria were the prevalence of depression and risk of suicide was 27.8% and 7.8% respectively for the HIV positive subjects, while it was 12.8% and 2.2% respectively for the HIV negative blood donors (controls). Studies done in Rwanda were patients attending at primary health care Centre in Kigali, with a prevalence of 41.7%. HIV related medical factors that were studied, being a female, having presented many HIV-related symptoms in the month prior to data collection, and having less than 250 CD4 counts were statistically associated with depression. On the other hand, having high social and family support was a protector factor to depression. Research done in Botswana was 1,268 participants surveyed, 25.3% of women and 31.4% of men had depression. Among women, lower education (adjusted odds ratio [AOR] 2.07, 95% confidence interval [1.30-3.32]), higher income (1.77 [1.09- 2.86]), and lack of control in sexual decision-making (2.35 [1.46- 3.81]) were positively associated with depression. Among men, being single (1.95 [1.02-3.74]), living in a rural area (1.63 [1.02- 2.65]), having frequent visits to a health provider (3.29 [1.88- 5.74]), anticipated HIV stigma (fearing discrimination if HIV status was revealed) (2.04 [1.27-3.29]), and intergenerational sex (2.28 [1.17-4.41]) were independently associated with depression(15). Cross-sectional studies done Tigris were Out of 269 total participants, 142(52%) were females, 213 (79.2%) were from urban area and 56(20.8) were from rural. One hundred nine (40%) of the study subjects' age range was 35-44 and 129 (48%) were married. Orthodox religion constituted 80% followed by Muslim (11.5%) and Catholic (0.4%). Sixty (22.3%) were unemployed and majority, 229(85.2%) had a minimum of primary education. Among 269 participants 43.9% were depressed. Depression was associated with urban dwellers, with lower socio-economic class, unemployed and government employees, with OR of 3.19(1.5, 6.65), 4.43(1.35, 14.58), 2.74(1.34, 5.57), and 3.56(1.73, 7.30) respectively (7-16).
Justification of the study
The World Health Organization report on HIV/AIDS and mental illness (WHO, 2008) has indicated that while low and middleincome countries carry more than 90% of the burden of HIV/AIDS, there is very little information about the interaction between HIV/AIDS and mental health in these countries.
The findings of this study would add to the limited body of knowledge about the prevalence rate of depression among HIV/ AIDS infected patients in Ethiopia. It will also serve as a clinical reference to HIV care providers who may use the findings to offer comprehensive care to their patients. Since little is known about the prevalence of depression and the factors associated with Depression in a population of PLWHA in Ethiopia, this study might serve as a foundation for future public health and Mental Health research in the area, thus deepening understanding of the issue. It is therefore anticipated that the findings of this study will contribute to the development of local knowledge about mental illness and HIV/AIDS and used to inform Mental Health education curricula for both community and mental Health should be incorporated. The findings of this study might also help in influencing the development of appropriate policies, plans and intervention programs for the management of psychiatric illnesses in HIV/AIDS care settings. This in turn, might improve the quality of life for HIV/AIDS patients who are also suffering from Depression.
Objective
General objective
To assess the prevalence of depression and associated factors among HIV/AIDS patients attending ART clinic in Debrebirhan Referral Hospital, North Showa, Amhara Region, Ethiopia.
Specific objectives
To determine the prevalence of depression among HIV/AIDS patients attending ART Clinic in Debrebirhan Referral Hospital, North Showa, Amhara Region, Ethiopia.
To identify associated factors of depression among HIV/AIDS patients attending ART Clinic in Debrebirhan Referral Hospital, North Showa, and Amhara Region, Ethiopia.
Methods
Study design
Institutional based cross-sectional study design was employed.
Study area
The study was conducted in Debrebirhan Referral Hospital, Debrebirhan town, North Showa Ethiopia from April to May, 2013. Debrebirhan Town is located in the North Shoa Zone of Amhara Regional State 695 km from Bahirdar and 130 km from the capital of Ethiopia, Addis Ababa. Administratively, Debrebirhan District has 9 urban kebeles (smallest administrative units). Based on the 2007 Census conducted by the Central Statistical Agency of Ethiopia (CSA), Debrebirhan Town has an estimated total population of 61,025. In the study area, there are one Referral Hospital, one private Hospital, three health centre and five private clinics and six private pharmacies. Debrebirhan referral hospital is the only Referral Hospital in North Showa and also serves for patients from parts of Oromo and Afar regions. It serves for more than two million people. Debrebirhan Referral Hospital provides care and treatment for around 2287 PLWHA who comes from different areas and from these 1467 was on HAART the end of February 2013 and the rest 820 were on Pre ART care. The hospital has separate clinic that provide care and treatment for HIV/AIDS patients with daily visits ranging from 40 to 60. The total average monthly visit is 1200-1600 patients.
Study period
The study was conducted from April to May, 2013.
Source Population
Source population was comprised of all HIV infected patients receiving treatment (both on ART and pre-ART) at ART clinic of Debrebirhan referral hospital.
Study Population
Study population is comprised of all HIV infected patients receiving treatment (both on ART and pre-ART) at ART clinic in Debrebirhan Referral Hospital.
Data collection instrument
A structured questionnaire was used to collect data on sociodemographic characteristics (age, sex, ethnicity, religion, education, occupation, and marital status). PHQ-9 (Patients Health Questioners 9) was used to measure the depression level of HIV/AIDS patient. The PHQ-9 has demonstrated acceptable reliability, validity, sensitivity, and specificity (PHQ-9 score has a sensitivity of 88% and a specificity of 88% for major depression). A questionnaire format was used to collect CD4count, stage of HIV, duration on HIV status to be now, drug regimen, substance use, perceived stigma and social support. The researcher was recruiting two Bachelor sciences of nurses to collect the data. They were oriented on how to fill the questionnaire, the ethical principles, confidentiality and data management prior to their involvement for data collection.
Data quality control issues
Data quality control issues were insured by conducting pre-test among 5% total samples obtained from patients attending at Debrebirhan Health Centre, one of the health centres located in the town which gives care and treatment for patients with HIV/ AIDS. Training was given to data collectors on the data collection tool and sampling techniques. Supervision was held regularly during data collection period. The collected data was checked on daily basis for completeness and Consistency. The questionnaire is translated to Amharic and back to English using backward forward translation method and feedback was obtained from two psychiatrist who have worked on depression most of their lives.
Data processing and analysis
The coded data was checked, cleaned by entering into Epi. Info version 7 and then exported into Statistical Package for the Social Sciences (SPSS window version 20) for analysis. Descriptive summary using frequencies, proportions, graphs and cross tabs was used to present results of the study. Bivariate analysis was done remove to determine each of these factors and how they are associated with the dependant variable. Only factors that have been found to be significantly associated with depression among HIV/AIDS during bivariate analysis were entered into the multivariate analysis. P value <0.05 was taken as statistically significant.
Ethical considerations
Ethical clearance was obtained from Ethical Review Boards of University of Gondar and Amanuel Mental Specialized Hospital. Moreover the researchers were striving to protect and respect the privacy, secrecy and wellbeing of patients. The data collected for the purpose of this study was not including identification to ensure secrecy of participants all of the collected data was used only for the purpose of this study. Verbal consent was obtained from participants and an outline of the purpose of the study explained with each client who agreed to participate voluntarily.
Results
Description of the general characteristics of the sample
Cross sectional study design was conducted at Debrebirhan Referral Hospital, Amhara Region, Ethiopia. The study determined the prevalence of depression and associated factors among 416 HIV/AIDS clients attending ART clinic at Debrebirhan Referral Hospital.
A total of 416 respondents were interviewed and 221(53.1%) were female. The mean age of the participants was 38 years and range from 21 to 69. Three hundred Eighty five (92.5%) were orthodox Christians, 184(44.2%) were married and 380(91.3%) were Amhara in ethnicity. 157(37.7%) were completed primary education and 106 (25.5%) were jobless. Monthly income of respondents involved in the study was between 401-700 birr for 108(26%) clients less than 200 birr for 105(25.2%) clients.
The minimum CD4 cell count of respondents (n=416) was 1 and the maximum CD4 cell counts was 4500 with a mean of 428.53, and a standard deviation (SD=397.36). More than three fourth of the respondents 317(76.2%) had CD4 counts greater than or equal to 250. more than half of the respondents 234(56.2%) were on ART. Only 126(30.3%) had perceived stigma. In this study substance use which is defined as use of any of the specified substance (tobacco, alcohol, chat, cannabis or cocaine) in the past three months was 18.3% (n=76) and majority of the participants 340(81.7%) were not substance users (Table 1).
| Variables | Category | Frequency | Percent (%) |
|---|---|---|---|
| Age category (in years) |
20-29 Year | 93 | 22.4 |
| 30-39 Year | 150 | 36.1 | |
| 40-49 Year | 113 | 27.2 | |
| 50-59 Year | 38 | 9.1 | |
| 60-69 Year | 22 | 5.3 | |
| Sex | Male | 195 | 46.9 |
| Female | 221 | 53.1 | |
| Ethnicity | Amhara | 380 | 91.3 |
| Oromo | 29 | 7 | |
| Tigris | 7 | 1.7 | |
| Marital status | Single | 94 | 22.6 |
| Married | 184 | 44.2 | |
| Divorced | 72 | 17.3 | |
| Widowed | 66 | 15.9 | |
| Religion | Orthodox | 385 | 92.5 |
| Muslim | 17 | 4.1 | |
| Protestant | 14 | 3.3 | |
| Education | Unable to write and read | 75 | 18 |
| Able to write and read | 47 | 11.3 | |
| Primary | 157 | 37.7 | |
| Secondary | 99 | 23.8 | |
| Tertiary | 38 | 9.1 | |
| Income | <200 Birr | 105 | 25.2 |
| 201-400 Birr | 103 | 24.8 | |
| 401-700 Birr | 108 | 26 | |
| >700 Birr | 100 | 24 | |
| Jobs | Employed | 310 | 74.5 |
| Unemployed | 106 | 25.5 | |
| CD4 count | < 250 | 99 | 23.8 |
| ≥250 | 317 | 76.2 | |
| HIV/AIDS stages | Stage I | 162 | 38.9 |
| Stage II | 93 | 22.4 | |
| Stage III | 140 | 33.7 | |
| Stage IV | 21 | 5.0 | |
| Started ART taking | Yes | 234 | 56.2 |
| No | 182 | 43.8 | |
| Hospitalized in the past one Month | No | 409 | 98.3 |
| Yes | 7 | 1.7 | |
| Felt stigmatized | No | 290 | 69.7 |
| Yes | 126 | 30.3 |
Table 1 Distribution sociodemographic variable among study paticipant, DBRH, North Showa, Amhara region, Ethiopia.
Prevalence of depression among HIV positive patients attending in debrebirhan referral hospital.
The prevalence of depression was assessed using PHQ-9. The scale constitutes a total score of 27. A score 0-4 was considered as no depression and the score ≥ 5 was considered as having depression. Based on the cut of point ≥ 5, the prevalence of depression was found to be 38.94%. Multiple logistic regressions were used to minimize the risk of confounder for factors like sociodemographic status, Substance use, and Perceived stigma. The association between these factors and depression were tested and from socio demographic characteristics, being female (AOR=2.071(1.077, 3.985) was associated with depression. Male to female ratio of depression was found to be 2.071:1 Age category between 30-39 years (AOR =2.761(1.165, 6.540)) was associated with depression, those with age category between 30-39years 2.761times more likely to develop depression than the age category between 20-29 years. Age between 40-49 years (AOR=3.847(1.489, 9.942)) was associated with depression, those with age between 40-49 years 3.847times more likely to develop depression than the age category between 20-29 years. Age between 60-69 years (AOR=19.645(4.020, 95.991)) was associated with depression, those with age between 60-69 years were 19.645times more likely to develop depression than the age category between 20-29 years. Income less than 200 birr (AOR=3.917(1.559, 9.845)) was associated with depression. Those with income less than 200birrs were 3.917 times more likely to develop depression than those with income greater than 700 birrs.Income between 201 to 400 birr (AOR=2.796(1.139, 6.865)) was associated with depression. Those with income between 201 to 400 birr were 2.796 times more likely to develop depression than those with income greater than 700 birrs. Income between 401 to 700 birr (AOR=2.590(1.058, 6.340)) was associated with depression. Those with income between 401 to 700 birr were 2.590 times more likely to suffer from depression than those with income greater than 700 birrs. HIV/AIDS Stage III (AOR=2.317(1.108, 4.848)) was associated with depression. Those patients with stage III HIV/AIDS were 2.317 times more likely to have depression than their referent group. Stage IV (AOR=8.769(1.928, 39.872)) was associated with depression. Those with Stage IV HIV/AIDS patients are 8.769 times more likely to develop depression than their referent group. Being hospitalized in the past one month was (AOR=15.262(1.463, 159.219)) associated with depression. Those hospitalized in the past one month was 15.262 times likely to develop depression than their referent group. Perceived stigmatized (AOR=3.597(1.861, 6.954)) was associated with depression. Clients with perceived stigmatized were 3.597times likely to develop depression than their referent group (Figures 1 and 2).
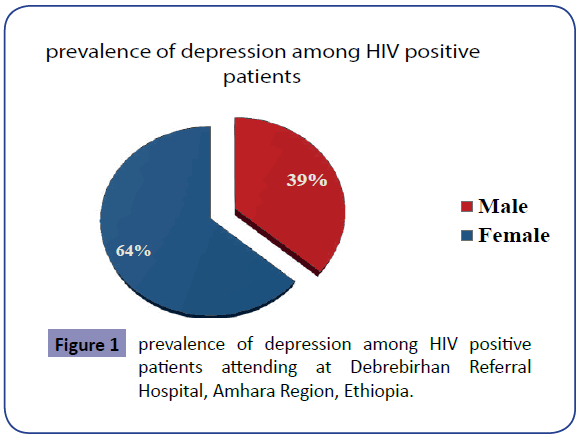
Figure 1: prevalence of depression among HIV positive patients attending at Debrebirhan Referral Hospital, Amhara Region, Ethiopia.
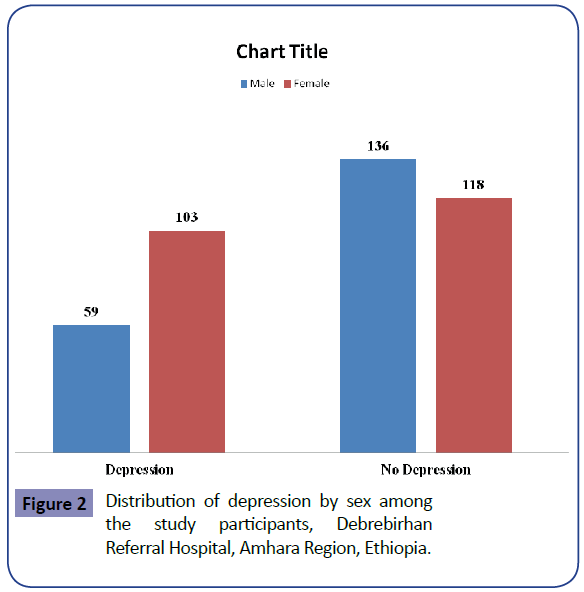
Figure 2: Distribution of depression by sex among the study participants, Debrebirhan Referral Hospital, Amhara Region, Ethiopia.
Discussion
In this study the prevalence of depression was found to be 38.94%. This cross-sectional study was also found significant associations between depression and being female, age category 30-39 years, 40-49 years. On the other hand, the number of HIV-related symptoms having Stage III and Stage IV disease were statistically associated with scoring positive to depression. Hospitalization in the past one month and felt stigmatized were statically associated with depression.
This study showed that there is high prevalence of depression among HIV/AIDS at Debrebirhan Referral Hospital when we compare the result with the general population. A cross-sectional study conducted by at three hospitals in Ethiopia on 269 HIV patients showed that prevalence of depression was 43.9% which was higher when we compare it with the finding in this research (16). The study done on prevalence depressions among HIV-infected patients attending a primary health care centre in Kigali found out that 41.7% of clients were depressed which is comparable with the finding of this research. Among them ninety six participants attending in this study (n=40) of them were depressed according to BDI (14). The result of our study is also higher than the study conducted in Uganda and south east Nigeria in which prevalence of depression was 8.1% and 27.8% respectively (12, 13). The possible reason for this difference might be due to the difference in instruments, study design and sample size. The prevalence rate of depression among HIV/ AIDS patient was 38.94% which is comparable to a study done at Aminu Kano Teaching Hospital, Nigeria in which the prevalence is reported to be 39.91%(8). The prevalence of depression in this study is lower than the study conducted in Brazil ,Delhi , Eastern Uganda and Jamaica in which the prevalence of depression were 53.5% ,58.75%, 47% and 43% respectively (1,2,5,9). Monthly income was significantly association with depression. This finding is consistent with study done at three hospitals in Ethiopia which found that income less than 200 birr’s associated with depression (15). Marital status, religion, educational status, employment status, started ART drug, most recent CD4 count (cells/μL) and social support were not significantly associated with MDD. Our findings are consistent with study done in semi-urban Entebbe district, Uganda (12). Stigma was significantly associated with depression in this research, which is consistent with research done in Botswana(15) (Table 2).
| Variable | category | Depression | p-value | AOR (95%CI) | |
|---|---|---|---|---|---|
| yes | NO | ||||
| Sex | male | 59 | 118 | - | R |
| female | 118 | 103 | 0.029 | 2.071(1.077, 3.985) | |
| Age group | 20-29 year | 26 | 67 | - | R |
| 30-39 year | 61 | 89 | 0.021 | 2.761(1.165, 6.540) | |
| 40-49 year | 47 | 66 | 0.005 | 3.847(1.489, 9.942) | |
| 50-59 year | 15 | 23 | 0.137 | 2.596(0.738, 9.128) | |
| 60-69 year | 13 | 9 | 0 | 19.645(4.020, 95.991) | |
| Income | <200 Birr | 50 | 55 | 0.004 | 3.917(1.559, 9.845) |
| 201-400 Birr | 42 | 61 | 0.025 | 2.796(1.139, 6.865) | |
| 401-700 Birr | 45 | 63 | 0.037 | 2.590(1.058, 6.340) | |
| >700 Birr | 25 | 75 | - | R | |
| HIV/AIDS stages | Stage I | 52 | 110 | - | R |
| Stage II | 33 | 60 | 0.339 | 1.461(0.671, 3.181) | |
| Stage III | 60 | 80 | 0.026 | 2.317(1.108, 4.848) | |
| Stage IV | 17 | 4 | 0.005 | 8.769(1.928, 39.872) | |
| Hospitalized in the past one Month | no | 156 | 253 | - | R |
| yes | 6 | 1 | 0.023 | 15.262(1.463, 159.219) | |
| Felt stigmatized | no | 100 | 190 | - | R |
| yes | 62 | 64 | 0 | 3.597(1.861, 6.954) | |
Table 2 Multivariate analysis of variables and depression symptoms among the study participant, DBRH, North Shoa, Amhara region, Ethiopia.
Conclusion
The aim of this study was to estimate the prevalence of depression and associated factors among people living With HIV/AIDS attending at Debrebirhan Referral from the findings of this study, it emerged that depression is high among people living with HIV/AIDS attending at Debrebirhan Referral For all the socio-demographic factors and HIV related medical factors that were studied, significant association was found between being female, age category 30-39,40-49 years old On the other hand, the number of HIV-related symptoms and having Stage III and Stage IV disease were statistically associated with scoring positive to depression. Hospitalization in the past one month and felt stigmatized were statically associated with depression.
Acknowledgments
We would like to acknowledge University of Gondar and Amanuel Mental Specialized Hospital for their financial support. We would also like to thank DebreBerhan Referral Hospital for support and cooperation during data collection.