Keywords
Non-hemodialysis; P5 methodology; Clinical outcomes
Introduction
According to the Agency for Healthcare Research and Quality, it is
vital to use a systematic, structured approach in order to succeed
in improving patients’ experiences [1]. Systematic approaches to
improving care delivery guided by data are referred to as Quality
Improvement (QI) and are designed to bring about immediate
improvements in health delivery in particular settings [2].
There are a variety of methodologies used in Quality Improvement
(QI) initiatives, including The Institute for Healthcare Improvement
(IHI) Model for Improvement, Lean and Six Sigma [2-4]. Regardless
of the methodology used, QI models share common features
including emphasis on leadership to hold people accountable,
clear goals, use of measurement and analysis to identify issues
and guide decisions, emphasis on stakeholders as participants
and audiences for the improvement processes, use of structured,
iterative processes to implement improvement interventions,
monitoring and data collection, and transparent metrics. It is
critical to carefully choose strategies that have the best chance to
improve patient interactions [1].
Recognizing that the majority of hospitalized patients require
vascular access device placement to facilitate the delivery of
care, insertion of these devices are not without risk [5-7]. It is
crucial for institutions to understand their unique complication
rates and patterns of utilization for various devices. Furthermore,
it is essential to develop protocols, processes and practices
aimed at reducing complications such as Central Line-Associated
Bloodstream Infection (CLABSI) and thrombotic catheter
dysfunction.
CLABSI are responsible for approximately 30% of all Healthcare-
Associated Infection (HAI) related deaths [6]. CLABSI is a significant
cause of morbidity and mortality in hospitalized patients [5].
Primary infection risks are associated with indwelling devices
such as vascular access devices which increase the potential for
a CLABSI. Infection risk correlates with an increasing number of
device lumens [7]. Research demonstrates that the odds ratio
for CLABSI increases by 50% with the use of a triple lumen PICC
compared with a dual lumen [7].
Studies have shown that patients with sepsis often have central
line-related thrombosis based on the presence of microbial colonization on most vascular catheters within a fibrin sheath
[8]. Catheter occlusions resulting from thrombosis are common
in vascular access devices and require clearance with tissue
Plasminogen Activator (tPA) which is a costly intervention [9].
If tPA does not clear the occlusion, then replacement of the
catheter is required which exposes the patient to undue risk of
an insertion related bloodstream infection [5].
Considering the charge that improving the quality of care of
patients is a fundamental obligation of health care providers [10],
our institution, Sunrise Hospital and Medical Center, assembled a
multi-disciplinary team of stakeholders to evaluate vascular access
products, practices and utilization patterns with the primary aim
of determining and addressing device-associated complication
rates, primarily CLABSI. The findings led to the development of a
novel process and QI strategy specific to patients’ vascular access
needs called P5. The core pillars of the methodology include
Promise, People, Process, Policy/Procedure and Products.
We are reporting on the development and implementation of the
P5 methodology at our institution, a 690-bed acute care hospital.
Additionally, we are reporting on the observational, retrospective
clinical outcomes data resulting from the implementation of this
QI initiative.
Methods and Design
The correlational approach to evaluating the P5 Pillars required
quantitative evaluation of CLABSI cases and quantitative
evaluation of tPA, midline, and PICC usage. The study period
was January 1, 2018 through December 31, 2018. The primary
research question was to determine the potential relationship
between the device manufacturer and three areas of impact
(device utilization, usage of tPA, and CLABSI).
The first pillar of P5, Promise, defined the primary purpose to
identify potential weaknesses/limitations in vascular access
care delivery and products and to develop a roadmap for the
improvement. A secondary purpose of the initiative was to create
an improvement platform that would be transferable to other QI
projects across the organization.
The second pillar, People, was established to determine all
the stakeholders whose participation was required for a
comprehensive vascular access program review. Additionally, a
review of stakeholder activities for the success of the program
was evaluated. The team consisted of the Administrative Director
of Critical Care (lead) along with Critical Care Management,
Vascular Access Team (VAT) members, Infection Prevention
Director, Chief Medical Officer, Clinical Practice Coordinators
(educators) and supply chain staff. Outside stakeholders included
the educators and vendors from the company currently supplying
the PICCs and Midlines (heretofore referred to as Company A)
along with a second company (heretofore referred to as Company
B), chosen to provide another perspective for the full review. A
third company was considered, but was eliminated early as a
non-contender due to inability to meet the product needs of the
facility for this type of device.
The third pillar, Process, consisted of evaluating criteria and
process for ordering Central Venous Catheters (CVC), Peripherally Inserted Central Catheters (PICC), or midline catheters. A review
of evidence-based practice was conducted using the Michigan
Appropriateness Guide for Intravenous Catheter (MAGIC) tool
developed by Chopra et al. [11].
The fourth pillar, Policy/Procedure was developed to provide
for review of vascular access insertion and removal practices,
as well as care and maintenance protocols to determine if
evidence-based practices were being utilized. A specific focus of
this review was to evaluate practices for removal of unnecessary
lines and de-escalation of line referrals to the most appropriate
access type (e.g. PICC vs. Midline). Additionally, a review of the
pharmacy protocol was conducted to ensure that infusate type
was considered in the process of appropriate device selection.
The fifth pillar, Products, was established to determine what
products were available specific to PICC and midline device
characteristics and manufacturers. At the time of the review,
there was a single vendor (Company A) for PICC and midline
products including 1) single-lumen midline full insertion kit, 2)
single-lumen midline catheter only kit, and 3) dual and triple
lumen maximum barrier full insertion PICC kit with tip location
stylet.
Two catheter manufacturing companies (Bard Access Systems,
Salt Lake City, UT, and Angio Dynamics, Inc., Latham, NY) were
invited to provide a comprehensive review of the vascular access
program at the hospital utilizing the P5 Methodology model. The
companies were given a week of access on separate occasions
during the same month to the facility’s four-person Vascular
Access Team to follow during vascular access device insertions,
removals and maintenance. The companies were allowed access
to ancillary department information and personnel including
supply chain, pharmacy and nursing leadership.
Hospital policies were shared with each company to determine
the need for any evidence-based changes. Finally, the vendors
were allowed to present the findings and recommendations for
any of the five layers of the P5 methodology. The devices under
consideration were midlines (Power Glide by Bard Access Systems,
Salt Lake City, UT and BioFlo by Angio Dynamics, Inc., Latham, NY)
and peripherally inserted central catheters (PowerPicc Solo2 by
Bard Access Systems, Salt Lake City, UT and BioFlo PASV PICC by
Angio Dynamics, Inc., Latham, NY).
Methods for the statistical analysis for identifying the primary
outcome of CLABSI was conducted through normal daily Infection
Prevention surveillance activities as part of the facility’s ongoing
infection prevention program. The CLABSIs were identified using
definitions as outlined by the Centers for Disease Control and
Prevention National Healthcare Safety Network (NHSN) Patient
Safety Component Manual [12]. The Chi-square test statistic was
calculated using IBM SPSS Statistical Software Version 25.0 to
validate that evidence was sufficient to reject the null hypothesis
of no association between the device company and CLABSI or tPA
at the significance level of a=0.05. A P-value <0.05 was considered
statistically significant. The remainder of the statistical analysis
was conducted using a simple quarter to prior quarter or year to
prior year percentage change.
Results
Promise
The initiative was successful in identifying specific areas of
improvement needed in the area of vascular access. The primary
issue identified issue was central-line associated bloodstream infections. Additionally, evidence-based device selection,
adherence to policies/procedures for catheter insertion, care and
maintenance, and vascular access device efficacy and proper use
were identified as areas of needed improvement.
Maintenance of PICCs and midlines were not consistently being
adhered to for all bundle elements such as maintaining clean,
dry and intact dressings for jugulars including antimicrobial disc
placement. Insertion issues were identified with one of the PICC
team members relative to sterile technique.
Utilization of multi-lumen lines being inserted was concerning
based on the guideline to choose the least number of lumens
for management of the patient [5]. Nine out of every ten PICCs
inserted were triple lumen. The policies did not clearly define the
evidence-based guidelines including proper line usage based on
appropriate reason. The order sets were misleading and resulted
in confusion and allowed for inappropriate vascular access
choices. The need for order clarification by the PICC team and
intervention by the physician was determined to be a source of
delays and care.
The midline catheter utilized by the hospital at the time of the
program inception had high technical insertion failure resulting in
wastage of multiple catheters to gain venous access. These failures
resulted in additional midline use of catheter only kits at a rate of
over 100 per month. There was also an unacceptably high rate of
failure to complete IV therapy using the midline device. Failures
resulted in treatment delays associated with device replacement
and also unnecessary procedures for patients. Failure reasons
observed by team members (inserters and educators) were
clotting or malfunction of the midline.
Furthermore, the device was not easily identifiable as a midline,
which led to inappropriate device use. For these reasons, the
midlines currently in use were a dissatisfier for the inserters, the
physicians and the patients.
Based on these identified areas of improvement, outcomes
measures were established in order to measure the success of the
program in terms of patient safety, product utilization and cost-
effectiveness (Table 1). Baseline data for the outcome measures
were compiled from a retrospective review of CLABSI data from
January 2018 through December 2018 and all other measures
from prior calendar year 2017 compared to 2018.
| QI Improvement need identified |
Outcome measure established |
Result |
| High utilization of triple lumen PICC use |
Reduce the use of triple lumen PICCs by 50% within 6 months |
98% reduction |
| Inability to complete prescribed therapy with midline initially placed |
Reduce the number of additional midlines needed to complete therapy by at least 25% within 6 months |
100% reduction |
| High tPA usage |
Decrease the usage of tPA by 60% within 6 months |
96% reduction |
| CLABSI rate unacceptably high |
Decrease the incidence of CLABSI related to PICCs within 6 months |
53% reduction |
Table 1: Quality improvement measures and outcomes for measure of
success.
People
The project team identified that re-validation of clinical
competencies was needed in order to improve care. The PICC
team skills were re-validated based on rigorous competency
criteria [13]. Where new products were implemented as part
of the program, members unable to achieve appropriate skills
or to adjust to work flow changes using the new products were
reassigned.
Additionally, the education and re-validation of clinical
competencies for Registered Nurses (RNs) and Certified Nurse
Assistants (CNAs) were accomplished through didactic and hands
on education for dressing maintenance, sterile glove technique
and vascular access continuation indications.
Daily conversations during leadership patient safety huddles
amongst Nursing, Quality, and Executive leaders led with nursing
personnel were highly encouraged to attempt to a de-escalation
of any vascular access device when possible and prompt removal
when no longer clinically indicated.
The PICC team job description was elevated to “Vascular
Access Specialists” to encourage ongoing specialty knowledge
achievement in the field of vascular access.
Process
In order to improve the criteria and process for ordering of
vascular access devices, the order sets were revised to clarify and
standardized to ensure appropriate guidance for the ordering
provider based on an algorithmic approach. Variability in device
selection and appropriate device utilization was eliminated.
Policies and procedures
Policy and procedure review resulted in a revision of the vascular
access policy to reflect the most recent guidelines for appropriate
device utilization based on infusate characteristics (vesicant,
length of time or osmolarity) [9,11,13,14]. As a result of this review,
procedures for insertion were updated based on evidence-based
protocols including the elimination of X-ray by use of intracavitary
technology where clinically indicated. The practice was being
completed this way, but the policy was not updated to reflect
this protocol. Finally, maximum barrier precautions for midline
insertion as recommended by the Infusion Nursing Society (INS)
Guidelines were integrated into protocol [14].
Products
As a result of the review of specific product type and manufacturer
being used, and in order to meet the objectives of the P5
implementation, new products (Company B) were implemented
and included 1) single and dual lumen midline maximum barrier kit 2) single and dual lumen midline catheter only kit, and 3)
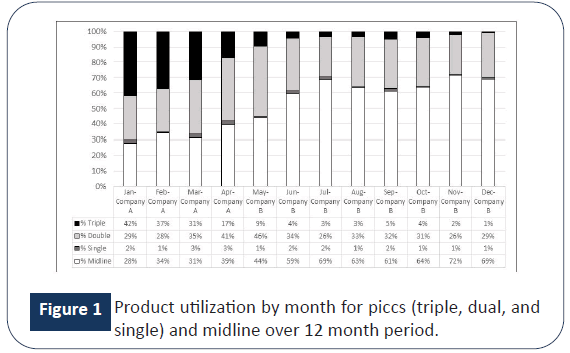
single, dual and triple maximum barrier PICC kit. Figure 1 outlines
the timeline for the transition of products from Company A to
Company B.
Figure 1: Product utilization by month for piccs (triple, dual, and
single) and midline over 12 month period.
A novel anti-thrombogenic catheter technology, Endexo® present
in Company B’s PICC and midline catheters was a critical factor
in choosing this product line. This was primarily because of the
potential for cost savings through avoidance of complications.
Additionally, the anti-thrombogenic property provided an
opportunity to increase patient satisfaction through the reduction
of catheter complications.
Based on the known increased risk of infection with each
additional lumen in use (or not in use but present), the reduction
of triple lumens was critical [9]. The use of triple lumen PICCs
equaled 42% of the total PICCS and midlines in use at the start of
the review in January 2018 as seen in Figure 1. Eight months post-
change triple lumens represented approximately 1% of the total
PICC insertions with a total count reduction of 216. The associated
cost reduction for utilizing a double lumen PICC instead of a triple
lumen during this period was almost $39,000.
Product utilization improved for midlines as a result of adherence
to appropriate device selection protocols with an increase in
midline insertions by 41%. The usage in 2017 for the original
midlines was 1,341 single sterile midlines (non-kits). For the
switch in 2018, the hospital purchased 48 single sterile midlines
(non-kits) from Company B. No single sterile midlines were
required for successful patient placement after the switch to
Company B which resulted in a cost savings of almost $ 60,000.
The pharmaceutical consideration was related to the cost of
using tPA. The tPA is used to assist with dissolving blood clots
that may be blocking central venous catheters in an attempt to
avoid the need to replace the line. The tPA administration was
reduced from 55 to two between Quarter 1, 2018 and Quarter
4, 2018. This was a 96% reduction in use with a cost savings of
approximately $ 18,000.
Clinical outcomes
The rate of PICC Line-related CLABSI for Company A was double
the rate of Company B (3.09 versus 1.44 per 1,000 PICC Insertions)
(Table 2). The overall reduction in PICC-related CLABSI was 53%. Table 3 demonstrates that the relation between these variables
was significant, X2 (1, N=1917)=5.896, p=0.015. Patients with a
catheter from Company B were significantly less likely to develop
a CLABSI than were patients with a catheter from Company A.
| |
#Weeks present in 2018 |
PICC Line related CLABSI |
PICC insertion volume |
Annualized insertion volume |
CLABSI Rate per 1.000 PICC Line insertions |
| Company A |
14 |
6 |
522 |
1939 |
3.09 |
| Company B |
38 |
2 |
1018 |
1393 |
1.44 |
Table 2: Comparison of CLABSI rates based on insertions pre-change and post-change.
| Clabsi developed*device company cross tabulation |
| Count |
Device Company |
|
| Company A |
Company B |
Total |
| Clabsi Developed |
No |
652 |
1257 |
1909 |
| Yes |
6 |
2 |
8 |
| Total |
|
658 |
1259 |
1917 |
| Chi-square tests |
| |
|
|
|
|
|
| |
Value |
df |
Asymptotic significance (2-Sided) |
Exact Sig. (2-Sided) |
Exact Sig. (1-Sided) |
| Pearson Chi-Square |
5.896a |
1 |
0.015 |
|
|
| Continuity Correctionb |
4.223 |
1 |
0.04 |
|
|
| Likelihood Ratio |
5.541 |
1 |
0.019 |
|
|
| Fisher's Exact Test |
|
|
|
0.023 |
0.023 |
| N of Valid Cases |
1917 |
|
|
|
|
a1 cells (25.0%) have expected count less than 5. The minimum expected count is 2.75.
bComputed only for a 2 × 2 table
Table 3: CLABSI versus device company SPSS output.
The overall reduction in tPA-usage was more than 95% in the adult
population. A chi-square test of independence was performed to
examine the relationship between tPA use and device company. Table 4 demonstrates that the relation between these variables
was significant, X2 (1, N=1917)=36.041, p<0.001. Patients with a
catheter from Company B were significantly less likely to require
tPA for line declotting than were patients with a catheter from
Company A.
| TPA used for the line?*device company cross tabulation |
| Count |
Device company |
Total |
|
| Company A |
Company B |
|
| TPA Used for the line |
No |
651 |
1164 |
1815 |
|
| |
Yes |
7 |
95 |
102 |
|
| Total |
|
658 |
1259 |
1917 |
|
| Chi-Square Tests |
| |
Value |
df |
Asymptotic significance (2-sided) |
Exact Sig. (2-Sided) |
Exact Sig. (1-Sided) |
| Pearson Chi-Square |
36.041a |
1 |
0 |
|
|
| Continuity Correctionb |
34.766 |
1 |
0 |
|
|
| Likelihood Ratio |
45.744 |
1 |
0 |
|
|
| Fisher's Exact Test |
|
|
|
0 |
0 |
| N of Valid Cases |
1917 |
|
|
|
|
a0 cells (0.0%) have expected count less than 5. The minimum expected count is 35.01.
bComputed only for a 2 × 2 table
Table 4: TPA usage versus device company SPSS output.
Discussion
As a result of this project, we were able to improve clinical
outcomes in term of tPA usage and CLABSI associated with PICCs,
and completion of therapy for midline devices. The outcomes
included a reduction in CLABSI by almost 90% for adult patients
with a PICC present (6 pre-change versus 2-post-change).
CLABSI was identified at significantly lower rates in patients with
Company B catheter versus Company A catheter (p=015). The
PICCs from Company A were inserted at a higher rate of 5.3 per
day versus Company B at a rate of 3.8 per day (Table 1).
The reduction of tPA usage may have further contributed to the
reduction of CLABSI in our project. In a study of 3,723, Thakarar
et al. reported that an adjusted odds of developing a CLABSI was
3.59 times greater in those patients with PICCs who received tPA
compare with those who did not (95% confidence interval (CI:
1.86-6.94) [9]. Furthermore, studies have shown that patients
with sepsis often have central line-related thrombosis based on
the presence of microbial colonization on most vascular catheters
within a fibrin sheath [8].
Economic considerations related to product and pharmaceutical
utilization were also an essential aspect of our project. The final
triple lumen reduction was 98% by December, 2018 with a cost savings of approximately $ 39,000. The implementation of a
stellar midline product resulted in an increase in usage of 41% and a 100% decrease of wasted nursing time with the product by
the end of 2018.
Limitations
The research was limited to adult populations due to the devices
under consideration. While this review resulted in a change of
product which added value, it is conceivable that a consistent
review of all other elements without a product change might
have impacted the outcome measures.
Conclusion
This project represents a systematic, multi-disciplinary approach
to improving the quality of care delivery related to vascular
access in our institution. While each pillar of the P5 methodology
was complex, the multi-disciplinary approach allowed success in
achieving the outcomes of interest, primarily CLABSI reduction.
It is conceivable that this framework for quality improvement
related to vascular access outcomes may be reproducible by
other institutions.
Implications for Practice
The P5 methodology can assist hospital administrators or vascular access program managers with improving clinical and
financial outcomes. The application of a single pillar may identify
opportunities for improvement; however the implementation
of all five pillars will maximize the overall potential program
improvement possibilities. The framework for P5 methodology
follows the Six Sigma quality improvement model: Plan, Do,
Check, Act (PDCA) which encourages continuous evaluation.
Further Research or Scope
The scope of the project for future research could include external
validation at other sites and in specific population needs such as
pediatrics, oncology or dialysis.
Disclaimer: This research was supported (in whole or in part)
by HCA Healthcare and/or an HCA Healthcare affiliated entity.
The views expressed in this publication represent those of the
author(s) and do not necessarily represent the official views of
HCA Healthcare or any of its affiliated entities.
Conflicts of Interest and Source of
Funding
None were declared for the authors.
References
- (2019) Ambulatory care improvement guide: Ways to approach the quality improvement process. Agency for Healthcare Research and Quality.
- Furterer SL (2016) Lean six sigma in service: Applications and case studies. (edn) CRC press.
- Barnes‐Daly MA, Pun BT, Harmon LA, Byrum DG, Kumar VK, et al. (2018) Improving health care for critically ill patients using an evidence‐based collaborative approach to ABCDEF bundle dissemination and implementation. Worldviews Evid Based Nurs 15: 206-216.
- Clark DM, Silvester K, Knowles S (2013) Lean management systems: Creating a culture of continuous quality improvement. J Clin Pathol 66: 638-643.
- O'grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, et al. (2011) Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 52: e162-e193.
- Centers for Disease Control and Prevention, 2011. Vital signs: Central line-associated blood stream infections-United States, 2001, 2008, and 2009. Ann Emerg Med 58: 447-450.
- Chopra V, Ratz D, Kuhn L, Lopus T, Chenoweth C et al. (2014) PICC-associated bloodstream infections: Prevalence, patterns, and predictors. Am J Med 127: 319-328.
- Raad I, Darouiche R, Dupuis J, Abi-Said D, Gabrielli A, et al. (1997) Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections: A randomized, double-blind trial. Ann Intern Med 127:267-274.
- Thakarar K, Collins M, Kwong L, Sulis C, Korn C, et al. (2014) The role of tissue plasminogen activator use and systemic hypercoagulability in central line-associated bloodstream infections. Am J Infect Control 42:417-420.
- (2019) Quality improvement vs research. Children’s Hospital of Philadelpia Research Institute.
- Chopra V, Flanders SA, Saint S, Woller SC, O'Grady NP, et al. (2015) The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): Results from a multispecialty panel using the RAND/UCLA appropriateness method. Ann Intern Med 163:S1-S40.
- (2019) Centers for disease control and prevention. National Healthcare Safety Network Patient Safety Component Manual.
- Wyckoff MM, Sharpe EL (2015) Peripherally inserted central catheters: Gideline for practice. (3rd edn), National Association of Neonatal Nurses, Chicago, Illinois.
- Infusion Nurses Society (2016) Infusion therapy standards of practice. J Infus Nurs 39:S1-114.