Case Report - (2025) Volume 11, Issue 1
Missing Isthmus Endodontic Mishap - A Case Report
Badria Almatrafi1*,
Reem AlIdrisi1,
Hussein Mukhles1,
Hisham Zaidan1,
Abdulmajeed Altakhee1,
Waffa Albusais1,
Mawaheb Alharbi1,
Amal alshehri1,
Saud Alsaif2,
Norah Alotaibi3 and
Mshael Almohaimel3
1Department of Dentistry, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
2Department of Dentistry, Dentistry College, Riyadh Elm University, Riyadh, Saudi Arabia
3Department of Dentistry, Dentistry College, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
*Correspondence:
Badria Almatrafi, Department of Dentistry, Prince Sultan Military Medical City, Riyadh,
Saudi Arabia,
Email:
Received: 04-Oct-2023, Manuscript No. IPPDPD-23-17853;
Editor assigned: 06-Oct-2023, Pre QC No. IPPDPD-23-17853 (PQ);
Reviewed: 20-Oct-2023, QC No. IPPDPD-23-17853;
Revised: 14-Feb-2025, Manuscript No. IPPDPD-23-17853 (R);
Published:
21-Feb-2025, DOI: 10.36648/ 2471-3082.11.1.32
Abstract
Endodontic therapy aims to eliminate diseased pulp tissue and effectively seal the root canal system to prevent reinfection. However, failures can occur if the therapy deviates from established standards. This case report highlights an endodontic mishap involving a missing isthmus, a critical anatomical feature that can compromise treatment success. A 38-year-old female presented with discomfort in the lower right area of her mouth related to an endodontically treated tooth. Despite a wellobturated root canal, Symptomatic Apical Periodontitis (SAP) persisted. Exploratory surgery revealed a missing apical isthmus associated with the mesial canal. An apicoectomy was performed, and the isthmus was sealed with MTA. The case underscores the importance of identifying and addressing isthmus presence to improve treatment outcomes. Modern microsurgical techniques, including the use of magnification and biocompatible materials, are effective in managing such complexities, demonstrating high success rates in long-term follow-ups.
Keywords
Endodontic therapy; Isthmus; Apical periodontitis; Microsurgery; Root canal system
Introduction
Endodontic therapy aims to completely remove all diseased pulp tissue from the root canal system, clean it, and shape it so that it may be filled with an inert substance, reducing or eliminating the possibility of reinfection. Failure occurs though when endodontic therapy strays from accepted clinical standards [1].
For the treatment of persistent apical periodontitis after non surgical endodontic treated teeth the endodontic root-end surgery is indicated. And to make the procedure predictable, safer, and easier to perform various surgical techniques were introduced [2].
Over the past several years, there have been significant technological and procedural advancements in the area of endodontics. The manner surgery is carried out may be the one aspect of endodontics that has seen the most advancement. The distance between biological ideas and the capacity to produce consistently positive therapeutic results has shrunk because to the employment of cutting-edge equipment, novel and enhanced materials, and a surgical operating microscope. Endodontic microsurgery is the term now used to describe the use of these methods [3].
A thin, ribbon-shaped passageway between two root canals called an isthmus contains pulp or tissue deriving from pulp. The isthmus is not an independent entity but a component of the canal system. As a result, it has to be cleaned, shaped, and filled completely. The endodontist should be aware that isthmuses are present in premolars and molars at the 3 mm level from the apex in about 80% to 90% of instances when undertaking apical surgery. And the incidence of isthmus failure in mandibular first molar as shown in study was 83% [4].
Case Presentation
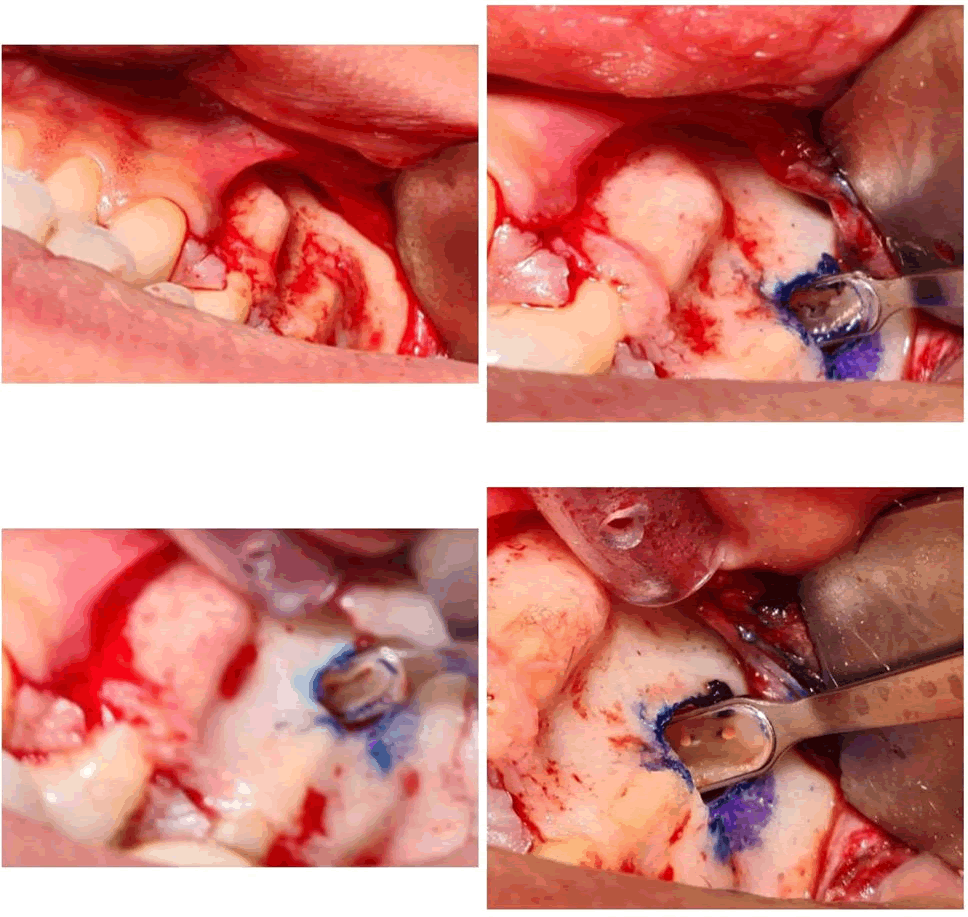
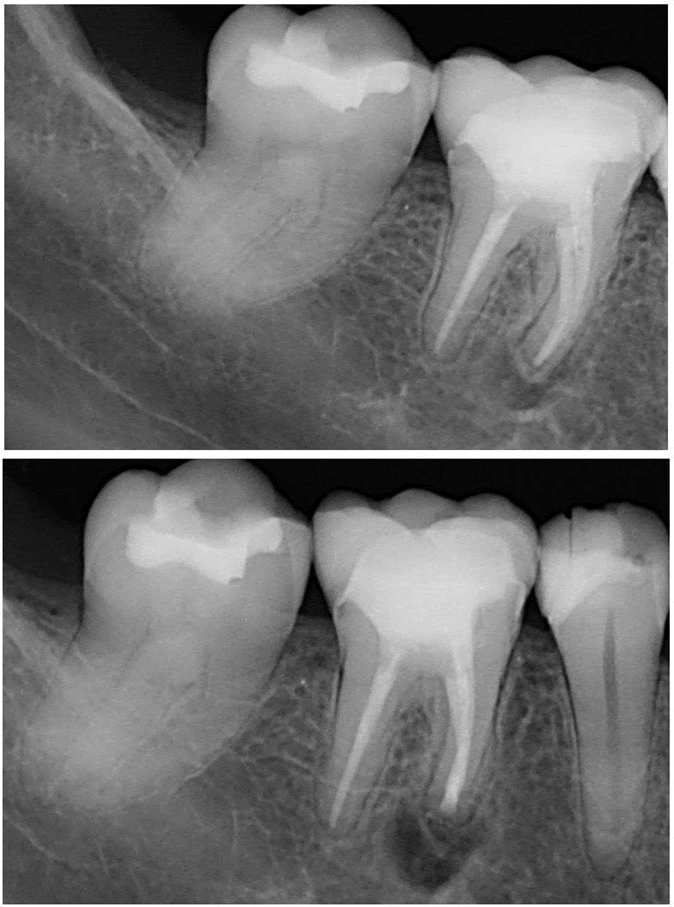
38 years old female, medically fit, came to Princes Sultan Military Medical City (PSMMC) primary care dental center complaining from slightaly discomfort related to lower right area when blending her foundation makeup by beauty blender. After examination tooth #46 is endodontically treated tooth 10 years ago with excellent obturation. And there is Symptomatic Apical Periodontist (SAP) [5]. The endodontist decided to do exploratory surgery to check the reason. He found missing apical isthmus related to mesial canal. Apicectomy done and the isthmus closed with MTA. Figures shown below (Figures 1 and 2).
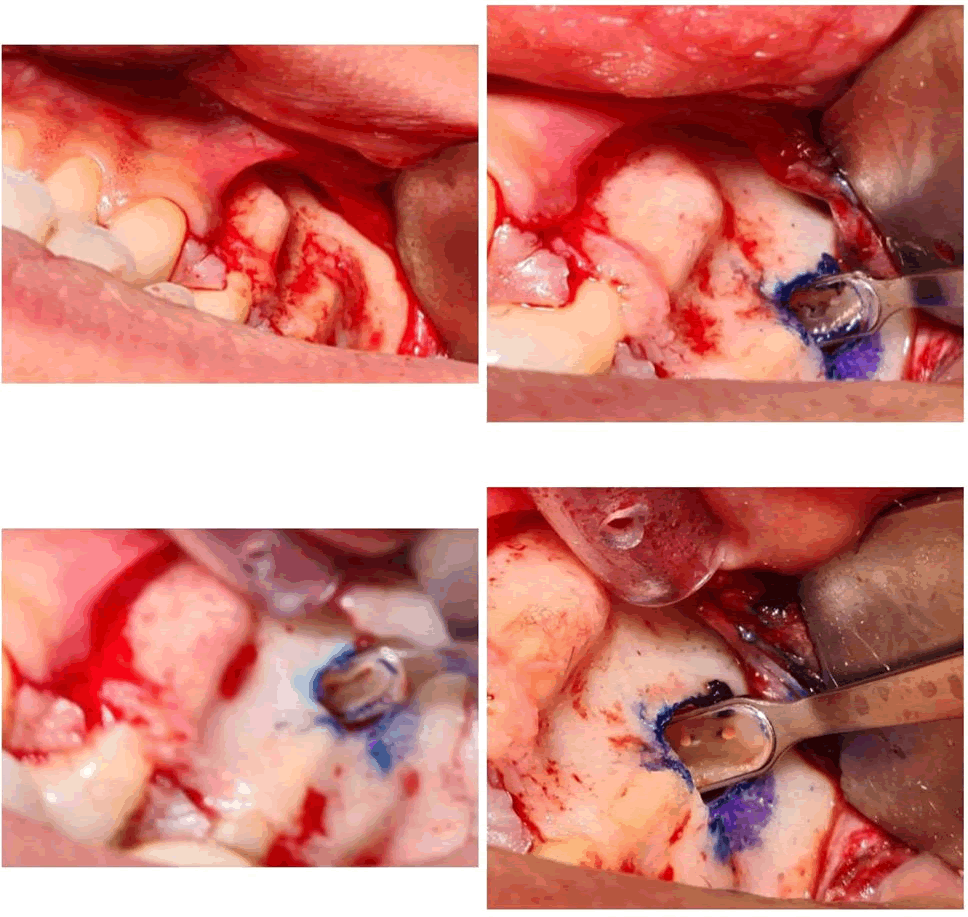
Figure 1: Surgical placement of dental implant with guided pin positioning technique.
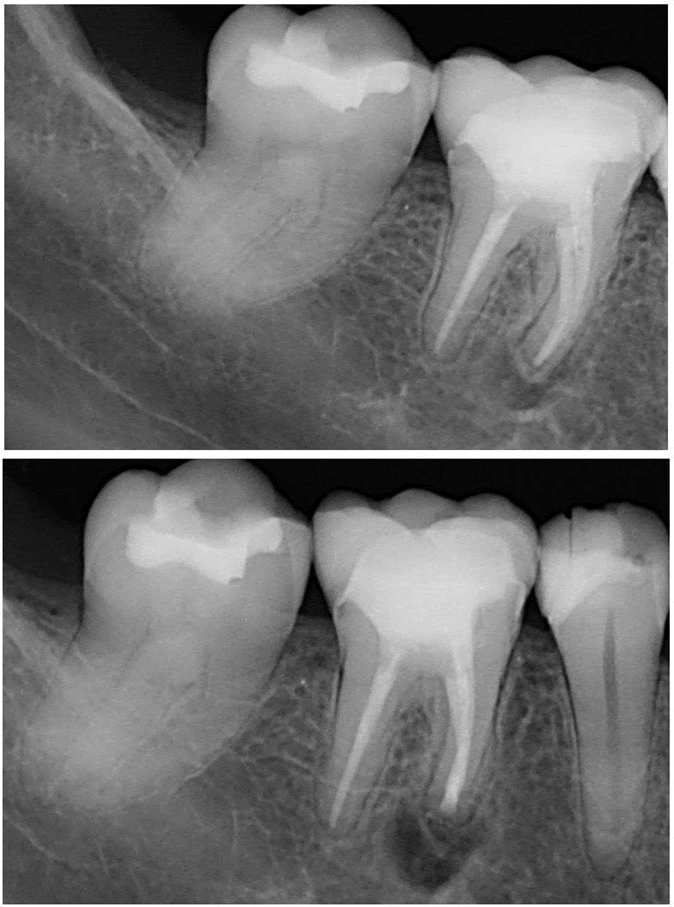
Figure 2: Pre and post-treatment radiographs showing periapical healing progression stages.
Discussion
The intricate anatomical nature of the root canal is one of the root canal treatment's challenges [6]. Anatomic complexity is made up of many different components, such as the fin and lateral canal, and isthmuses in particular present difficulties for endodontists. No precise technique for cleaning and shaping an isthmus has yet been developed, despite the fact that numerous preparation and irrigation procedures have been presented to get around the anatomical complications. The dental operating microscope, ultrasonics, modern microsurgical equipment, and biocompatible root-end filling materials are some of the technological advancements used in modern microsurgical peri-radicular surgery, which has produced highly successful treatment outcomes [7]. The increased success rates were attributed to a superior surgical site examination and the exact preparation of root-ends with micro-instruments using high magnification and improved illumination. In order to create a cavity that can be effectively filled during root end resection surgery, root-end preparation tries to remove filling material, irritants, necrotic tissue, and residues from the canals and the isthmus. The optimal root end preparation is a class I cavity with walls parallel to and inside the anatomic shape of the root canal space that extends at least 3 mm into the root dentin. The prevalent practice in conventional surgical procedures, the use of rotating burs in a micro-hand piece, is no longer able to provide this therapeutic need. The brand or kind of tip is not clinically significant for an effective ultrasonic preparation, but rather how the tip is used. The secret to successful ultrasonic preparation is to repeatedly apply very little pressure. A softer touch improves cutting efficiency, whereas continuous pressure, as that applied by a hand piece, reduces cutting effectiveness. This is so that ultrasound can operate through vibration rather than pressure. To increase the success rates of endodontic microsurgery for posterior teeth, an isthmus must be identified and treated [8]. A missed isthmus can result in failure. According to Sunil Kim et al., isthmus present teeth had a worse success rate for endodontic microsurgery than isthmus absent teeth did. The complexity of the isthmus preparation method itself is one of the causes of the significantly lower success rate in teeth with isthmus presence. In comparison to teeth with an absent isthmus, teeth with an extant isthmus must be more weakened in order to create space for a root canal. This lowers the success rate of the surgery. At the short-term follow-up after one year and the long-term follow-up after five to seven years, the clinical success of cases treated with microsurgery is reported to be as high as 96.8% and 91.5%, respectively. Similar findings have been revealed by recent prospective studies with long-term follow-up.
Conclusion
Even with good endodontic treatment missing isthmus can be found and cause failure of treatment. As studies shown microsurgery is predictable and effective treatment for this mishap.
References
- Siqueira Jr JF (2001) Aetiology of root canal treatment failure: Why wellâ?treated teeth can fail. Int Endod J. 34(1):1-10.
[Crossref] [Google Scholar] [PubMed]
- Friedman S (2011) Outcome of endodontic surgery: A meta-analysis of the literature-part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 37(5):577-578.
[Crossref] [Google Scholar] [PubMed]
- Kratchman SI (2007) Endodontic microsurgery. Compend Contin Educ Dent. 28(6):324-320.
[Google Scholar] [PubMed]
- Floratos S, Kim S (2017) Modern endodontic microsurgery concepts: A clinical update. Dent Clin North Am. 61(1):81-91.
[Crossref] [Google Scholar] [PubMed]
- Von Arx T (2005) Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. Int Endod J. 38(3):160-168.
[Crossref] [Google Scholar] [PubMed]
- Kim S, Jung H, Kim S, Shin SJ, Kim E (2016) The influence of an isthmus on the outcomes of surgically treated molars: A retrospective study. J Endod. 42(7):1029-1034.
[Crossref] [Google Scholar] [PubMed]
- Setzer F, Harley M, Cheung J, Karabucak B (2021) Possible causes for failure of endodontic surgery: A retrospective series of 20 resurgery cases. Eur Endod J. 6(2):235-241.
[Crossref] [Google Scholar] [PubMed]
- Tabassum S, Khan FR (2016) Failure of endodontic treatment: The usual suspects. Eur J Dent. 10(01):144-147.
[Crossref] [Google Scholar] [PubMed]
Citation: Almatrafi B, AlIdrisi R, Mukhles H, Zaidan H, Altakhees A, et al. (2025) Missing Isthmus Endodontic Mishap–A Case
Report. Periodon Prosthodon. 11:32.
Copyright: © 2025 Almatrafi B, et al. This is an open-access article distributed under the terms of the Creative Commons
Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author
and source are credited.