Goknur Bilen1, Bengu Cevirgen Cemil1, Fatma Fulya Köybasioglu2, Muzeyyen Gonul1
1Department of Dermatology, Ministry of Health Diskapi Yildirim Beyazit Education and Research Hospital, Ankara, Turkey
2Department of Pathology, Ministry of Health Diskapi Yildirim Beyazit Education and Research Hospital, Ankara, Turkey
- *Corresponding Author:
- Bengu Cevirgen Cemil
Department of Dermatology, Ministry of Health Diskapi Yildirim Beyazit Education and Research Hospital, Ankara, Turkey.
Tel: +90 312 5962083/+90 533 6296195
Fax: +90 312 472 95 34
E-mail: vivek03sharma@rediffmail.com
Received Date: October 15, 2015; Accepted Date:November 18, 2015; Published Date: November 25, 2015
Citation: Bilen G, Cemil BC, KöybaÃÆÃââââ¬Ã¦ÃÆââ¬Å¡Ãâ¦Ã¸ÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñoÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâ¦Ã¸lu FF, et al. Lichen Striatus: A Case Report. Clin Pediatr Dermatol. 2016, 1:1 Doi: 10.21767/2472-0143.100006
Keywords
Lichen striatus; Erythematous papules; Dermatoses; Hypopigmentation.
Introduction
Lichen striatus (LS) is rare, self-limited dermatoses [1]. It can be seen in all age groups, and mostly affecting 3-15 years old female patients [2]. It is characterized by small linear, pink, likenoid, initially discrete but rapidly coalescing papules [3]. The diagnosis is given by clinicians but there can be difficult to differentiate it from other linear dermatosis [1]. The histopathological findings are non-specific but this is significant for making a differentiation for LS and other linear dermatosis [3]. Herein, we present a case of a young girl developing LS on the trunk.
Case Report
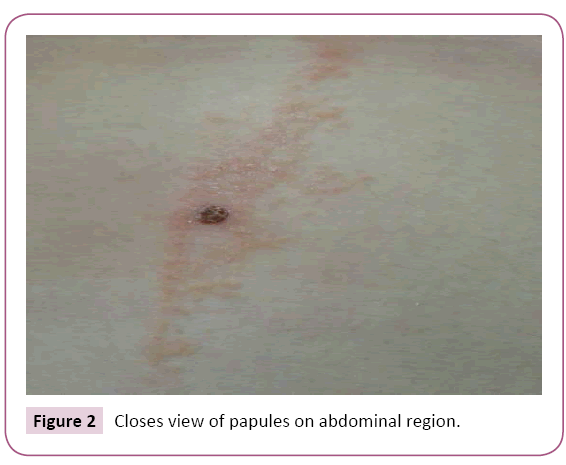
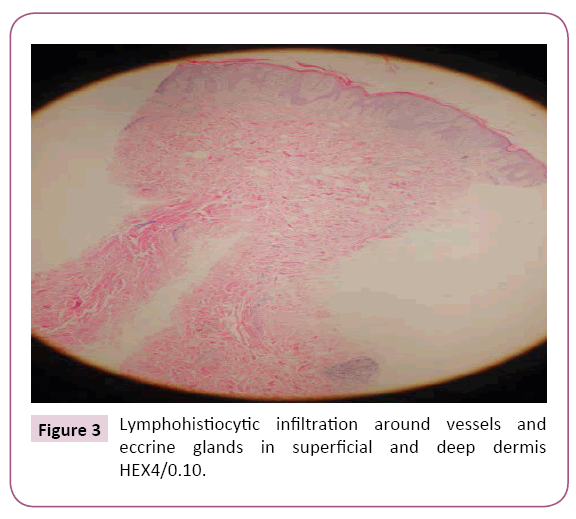
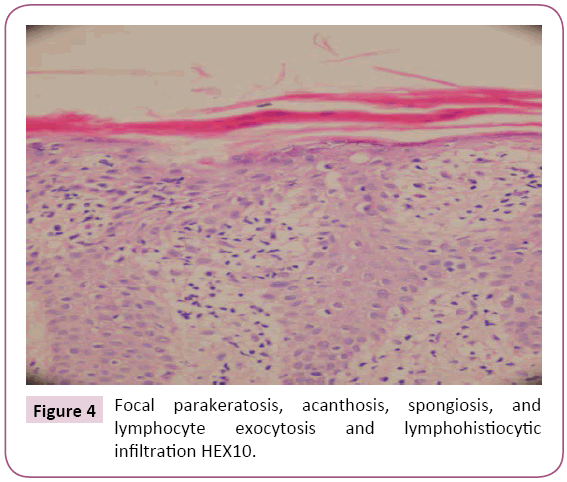
A 15 year old girl presented with a 4-month history of lesions start from upper part of umbilicus and spread towards the left axilla. She was asymptomatic with no history of vaccination, infection, drug abuse and atopy. Her medical history and family history were unremarkable. Dermatological examination revealed erythematous, smooth surfaced, linear papules starting from central trunk and spreading toward left breast and left axilla resembling Blaschko lines (Figures 1 and 2). There were no lesions on mucosa and nails. Skin biopsy from the papules on the trunk revealed parakeratosis and acanthosis in the epidermis, thinning in papillary dermis, infiltration of lymphocytes, and histiocytes, and degeneration at basal layer (Figures 3 and 4). On the basis of the clinical course and histopathological characteristics, the lesions on the patient’s trunk were diagnosed as LS. After 1 month steroid treatment the lesions have disappeared. Still there is no recurrence of the lesions.
Figure 1: Linear erythematous papules on the trunk following the Blaschko line.
Figure 2: Closes view of papules on abdominal region.
Figure 3: Lymphohistiocytic infiltration around vessels and eccrine glands in superficial and deep dermis HEX4/0.10.
Figure 4: Focal parakeratosis, acanthosis, spongiosis, and lymphocyte exocytosis and lymphohistiocytic infiltration HEX10.
Discussion
LS is characterized by shiny, flat, erythematous papules that vary from 2 to 4 mm, following Blaschko lines, which coalesce in liner disposition, forming a band that can be discontinuous [1,2]. The papules appear over 2 to 3 weeks and often have a lichenoid appearance without Wickham’s striae [4]. Lesions are generally asymptomatic and rarely can be accompanied by pruritus [5]. LS lesions are typically solitary and unilateral [2,3]. Unilateral or bilateral multiple lesions are very rare. Lesions are generally distributed on the extremities but also on the neck and trunk [3].
Nail involvement occurs exclusively in children, and is most often restricted to one nail [6]. Longitudinal ridging and splitting are common clinical features of nail involvement in LS [7]. The course of the disease is prolonged between 6 months to 5 years when nail involvement exists [6]. It has a sudden onset and the mean duration of this self limited disease is about 9 months frequently with residual hypopigmentation [1,3,4].
LS etiology is as yet unknown [2,4]. Studies have shown that LS is a T cell mediated inflammatory skin disease [3]. LS are defined in inflammatory acquired Blaschko-linear dermatoses [6]. Blaschko lines have an embryologic origin and correspond to the direction of growth of the cutaneous cells, resulting in a cutaneous mosaicism [8]. In acquired Blaschko-linear dermatoses, initially the abnormal clone of keratinocytes is not clinically obvious [9]. According to many authors, presence of epithelial cells genetically abnormal that through a triggering event can be known by the immune system and alternatively, the affected skin may respond to a precipitant with an over T cell mediated inflammatory response, apparent in Blaschko lines [1,9]. A majority of cases occur in the spring and summer, suggesting that the infections and environmental factors are associated with LS [1]. Vaccinations, trauma and pregnancy have been reported as other precipitating factors [9]. Our patient did not have any triggering factors.
Histopathologically a perivascular inflammatory infiltrate of lymphocytes and histiocytes in the upper dermis, which occasionally extends to the deep dermis, is seen. Epidermal features may include spongiosis, exocytosis, and dyskeratosis. A lichenoid pattern with inflammatory infiltrate near the dermoepidermal junction may be present [2]. A finding that is quite characteristic of lichen striatus is the presence of a fairly dense peri-eccrine and periadnexal infiltrate of lymphocytes. This finding alone may serve to differentiate lichen striatus from other eczematous dermatoses [10].
The differential diagnosis of LS includes other dermatoses following the Blaschko lines such as the inflammatory linear lichen planus, linear lichen nitidus, linear lichenoid drug eruption, linear psoriasis, lichenoid graft-versus-host disease, lupus erythematosus, atopic dermatitis, lichen planopilaris, lichen nitidus, vitiligo, pemphigus vulgaris, and porokeratosis [1,4]. Histopathological examination provided definite diagnosis.
The most common treatment is topical corticosteroids and there are reports on the satisfactory use of tacrolimus and pimecrolimus for persistent cases [1,3]. In our patient after 1 month topical corticosteroid treatment, lesions were rapidly improved.
Conclusion
LS are a rare dermatosis following the lines of Blaschko. LS should be considered at the differential diagnosis of diseases following the Blaschko lines. Knowledge of benign course of disease protects patients from unnecessary tests and treatments.
References
- Fogagnolo L, Barreto JA, Soares CT, Marinho FC, Nassif PW (2011) Lichen striatus on adult. An Bras Dermatol 86: 142-145.
- Taniguchi Abagge K, Parolin Marinoni L, Giraldi S, Carvalho VO, de Oliveira, et al. (2004) Lichen striatus: description of 89 cases in children. Pediatr Dermatol 21: 440-443.
- Vukicevic J, Milobratovic D, Vesic S, Milosevic-Jovcic N, Ciric D, et al. Unilateral multiple lichen striatus treated with tacrolimus ointment: a case report. Acta Dermatovenerol Alp Pannonica Adriat 181: 35-38.
- Dragos V, Mervic L, Zgavec B (2006) Lichen striatus in a child after immunization. A case report. Acta Dermatovenerol Alp Pannonica Adriat 15: 178-180.
- Mittal R, Khaitan BK, Ramam M, Verma KK, Manchanda M (2001) Multiple lichen striatus-an unusual presentation. Indian J Dermatol Venereol Leprol67: 204.
- Müller CS, Schmaltz R, Vogt T, Pföhler C (2011) Lichen striatus and blaschkitis: reappraisal of the concept of blaschkolinear dermatoses. Br J Dermatol164: 257-262.
- Inamadar AC (2001) Lichen striatus with nail involvement. Indian J Dermatol Venereol Leprol67: 197.
- Mun JH, Park HJ, Kim HS, Kim SH, Ko HC, et al. (2012) Lichen striatus occurring after allogenic peripheral blood stem cell transplantation in an adult with aplastic anemia. Ann Dermatol24: 87-89.
- Keegan BR, Kamino H, Fangman W, Shin HT, Orlow SJ, et al. (2007) Pediatric blaschkitis: expanding the spectrum of childhood acquired Blaschko-linear dermatoses. Pediatr Dermatol24: 621-627.
- Joshi R (2013) Interface dermatitis. Indian J Dermatol Venereol Leprol 79: 349-359.