Kartal D1*, Levent Çinar S1,Gül Kirkas Ö2, Ünal E2, Canöz Ö3 and Borlu M1
1Department of Dermatology and Venereology, School of Medicine, Erciyes University, Kayseri, Turkey
2Department of Pediatric Hematology, School of Medicine, Erciyes University, Kayseri, Turkey
3Department of Pathology, School of Medicine, Erciyes University, Kayseri, Turkey
- *Corresponding Author:
- Kartal D
Dermatology and Venereology Department, School of Medicine, Erciyes University, 38039-Kayseri, Turkey.
Tel: +903522076666-21916
Fax: +903524377615
E-mail: demetkartal@hotmail.com
Received Date: February 11, 2016 Accepted Date: March 01, 2016 Published Date: March 10, 2016
Citation: Kartal D, Çinar SL, Kirkas ÖG, et al. Leukemia Cutis Mimicking Kerion Celsi: A challenging Diagnosis for Clinicians. Clin Pediatr Dermatol. 2016, 2:1 Doi: 10.21767/2472-0143.100014
Introduction
Acute lymphoblastic leukemia (ALL) is an acute form of leukemia, characterized by the overproduction of immature white blood cell progenitors, known as lymphoblasts [1]. ALL is the most common form of malignancy in children with an incidence of 30%. The peak incidence occurs between two and five years of age.
Each year approximately 2500 to 3500 new cases of ALL are diagnosed in children in the United States. Nearly 70 to 80 percent of cases of childhood ALL are of B-precursor lineage (i.e., precursor B cell leukemia or early pre-B cell ALL). The most common presenting symptoms of ALL are nonspecific (e.g., bleeding, fever, lymphadenopathy, bone pain) [2,3]. Herein we report the case of a three year old girl with B cell ALL presenting with a nodule on the scalp skin, mimicking kerion celsi (tinea capitis profunda).
Case Report
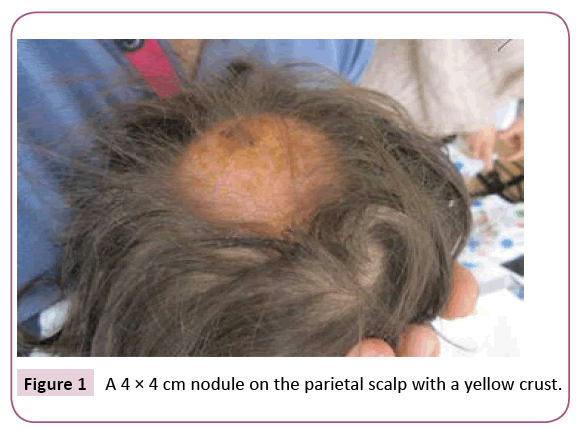
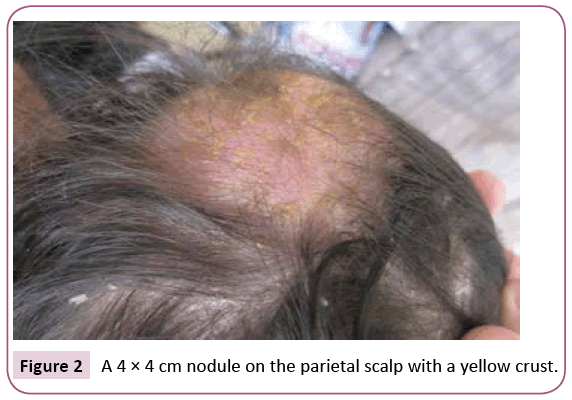
A 3 year old girl presented to our dermatology outpatient clinic with a nodule on the scalp of 4 weeks duration. She used topical and oral antibiotics and antifungals, without any improvement. She was healthy otherwise. On examination, there was a 4 × 4 cm nodule on the parietal scalp with a yellow crust (Figures 1 and 2). The hair on the nodule came out in clumps with gentle tugging. She had also multiple swollen posterior cervical lymph nodes. A possible differential diagnosis for her presentation includes kerion celsi or dissecting cellulitis of the scalp. A native preparate examination was made but no hyphae were seen. A fungal culture of the scale was sent.
Figure 1: A 4 × 4 cm nodule on the parietal scalp with a yellow crust.
Figure 2: A 4 × 4 cm nodule on the parietal scalp with a yellow crust.
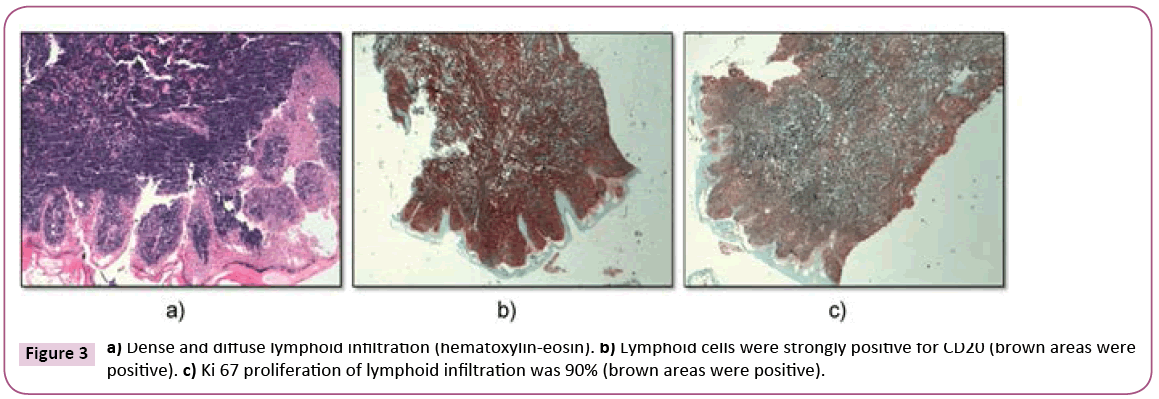
Oral griseofulvin 12.5 mg/kg was given for 6 weeks and topical selenium sulfide shampoo was added. On review a month later, there was no improvement. The culture on Sabouraud dextrose agar did not show any growth. A skin biopsy was performed. Histopathologic examination showed malignant lymphoid infiltration.
She was referred to the pediatric hematology department. Her complete blood count was as follows: WBC: 41 × 109/L, Hb: 16.3, Plt: 375. Physical examination showed hepatosplenomegaly cervical lymphadenopathy in addition to the nodule. Bone marrow aspiration was performed and morphological and flow cytometric analysis was consistent with B cell ALL. The ALL-IC BFM chemotherapy protocol [4] was started. On the 8th day the peripheral smear blast count was >1000/mm3 and on the 15th day bone marrow aspiration there were blasts >25% (nonremission). Therefore the patient was enrolled in the high risk group. The patient’s general condition deteriorated. Vomiting, abdominal distension, constipation and fever were observed. On the abdominal tomography, images of typhlitis were obtained. Despite granulocyte suspension and intravenous immunoglobulin, antibiotherapy and plasma exchange, the patient did not improve and eventually died (Figure 3).
Figure 3: a) Dense and diffuse lymphoid infiltration (hematoxylin-eosin). b) Lymphoid cells were strongly positive for CD20 (brown areas were positive). c) Ki 67 proliferation of lymphoid infiltration was 90% (brown areas were positive).
Discussion
Herein we describe a 3-year-old girl with a nodule on the scalp resembling kerion celsi as a clinical presentation of leukemia cutis. Kerion is the inflammatory extreme form of dermatophyte infection, caused by a vigorous T-cell-mediated host response to the dermatophyte infection [5]. It manifests as painful and suppurative plaques or nodules, accompanied by purulent drainage. The most affected area is the scalp, and it may result in scarring alopecia if treatment is delayed. Common pathogens to trigger kerion include Trichophyton mentagrophytes, Trichophyton verrucosum, Microsporum canis, Trichophyton tonsurans and Microsporum gypseum [6].
Leukemic skin infiltrates are a rare feature of ALL. A biopsy reveals a diffuse infiltrate of leukemic blasts around blood vessels and between collagen bundles [7]. In childhood, it is seen more commonly in congenital leukemia and acute myelogenous leukemia (10%) than in pediatric acute lymphoblastic leukemia (1%).
There are no preferred sites of involvement in leukemia cutis (LC). Until recently, there were few studies about leukemia cutis presentation in childhood. To date, the largest study with 1359 children (1259 children with ALL, 100 with LBL) was reported by Millot and colleagues [8]. Twenty four children had skin lesions at the time of diagnosis of the hematologic malignancy. The most commonly involved areas were the head. They described the lesions asymtomatic papules and nodules brown- red to violence without ulceration. Another study comprising seventy five children reported the nodule as the most common lesion and the extremities as the most frequent localization [9]. There have been many studies about B-cell proliferative disorders mimicking other dermatologic disorders (e.g., granuloma annulare, rosacea, rhinophyma) [10-12]. However there are no reports about B-cell proliferative disorders mimicking dermatophytosis in the literature.
Our patient presented with a solitary cutaneous nodule with a yellow crust. The native preparate examination was negative. However due to the fact that she had used topical antifungals we accepted the nodule as dermatophytosis. One other fact which supported our diagnosis was that the hair on the nodule came out in clumps with gentle tugging, so we tried to treat our patient with a systemic antifungal. As we did not observe any improvement after one month with antifungal treatment, a skin biopsy was made. Histopathology showed neoplastic lymphoid infiltration. High grade B cell lymphoma was diagnosed. LC often has rapid disease progression and poor prognosis. The mean interval between diagnosis of LC and death was reported as 3.8 and 4.8 months respectively in different studies [13,14]. The interval time was 2 months for our patient. An early diagnosis is essential in LC. The dermatologist plays a pivotal role in determining these suspected patients and in referring them to a hematologist.
References
- Sahu GR, Das BR (2005)Alteration of p73 in pediatric de novo acute lymphoblastic leukemia.BiochemBiophys Res Commun 327: 750-755.
- Ward E, DeSantis C, Robbins A, Kohler B, Jemal A (2014) Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin 64: 83.
- Shafer D, Wu H, Al-Saleem T, Reddy K, Borghaei H, et al. (2008) Cutaneous precursor B-cell lymphoblastic lymphoma in 2 adult patients: clinicopathologic and molecular cytogenetic studies with a review of the literature. Arch Dermatol 144:1155.
- Kolenova A, Kaiserova E, Makohusova M, Subova Z, Bubanska E, et al. (2015) Improved outcome for children and adolescent with acute lymphoblastic leukemia in the first decade of the 21st century: A report from the Slovak Republic. Neoplasma62: 812-820.
- Proudfoot LE, Higgins EM, Morris-Jones R (2011) A retrospective study of the management of pediatric kerion in Trichophyton tonsu-rans infection. Pediatr Dermatol28:655-657.
- Isa-Isa R, Arenas R, Isa M (2010) Inflammatory tinea capitis: kerion, dermatophytic granuloma and mycetoma. Clin Dermatol 28: 133-136.
- BurghdorfWHC, Gerami P, Yan AC (2011) Bening and malignant tumors. London Mosby, Pp: 1181-1218.
- Milllot F, Report A, Bertrand Y, Mechinaud F, Genevieve L, et al. (1997) Cutaneous involvement in children with acute lymphoblastic lymphoma. Pediatrics 100:1.
- Bernard A, Murphy SB, Melvin S, Bowman WP, Caillaud J, et al. (1982) Non-T, non-B lymphomas are rare in childhood and associated with cutaneous tumor. Blood59:549-554.
- Fullen DR, Jacobson SN, Valdez R, Novice FM, Lowe L (2003) Granuloma annulare-like infiltrates with concomitant cutaneous involvement by B-cell non-Hodgkin’s lymphoma: report of a case. Am J Dermatopathol25: 57.
- Di Meo N, Stinco G, Trevisan G (2013) Cutaneous B-cell chronic lymphocytic leukaemia resembling a granulomatousrosacea. Dermatol Online J19:13.
- Sokumbi O, Gibson LE, Comfere NI, Peters MS (2012) Granuloma annulare-like eruption associated with B-cell chronic lymphocytic leukemia. J Cutan Pathol 39:996-1003.
- Jang IG, Lee DW, Han CW, Kim CC, Cho BK (1996)A clinical observation on leukemia cutis. Korean J Dermatol 34: 507-514.
- Jang KA, Chi DH, Choi JH, Sung KJ, Moon KC, et al. (2000) Leukemia cutis:a clinico-pathologic study of 23 patients. Korean J Dermatol 38: 15-22.