Keywords
Kerstersia; Chronic otitis; Ciprofloxacin resistant
Introduction
Chronic otitis media (COM) is an insidious, slowly progressive inflammatory disease affecting the mucosal and bone structures of the medium ear and prone to persist and to produce severe sequelae [1].
Suppurate COM is known as chronic ear discharge through a tympanic drilling, lasting for at least 6 weeks with periods of inactivity [1]. Well-known risk factors for developing a COM are overcrowded living conditions, recurrent respiratory tract infections and smoking [2].
Staphylococcus aureus following by gram negative bacillus as Proteus spp., Klebsiella spp., Escherichia spp. and Haemophilus influenza are common pathogens causing COM. Bacteroides spp. and Fusobacterium spp. are the anaerobes more frequently isolated. There are also mixed infections and several cases of COM produced by less known bacteria as Bordetella, Achromobacter, Alcaligenes and Kerstersia [2-5] have been described.
We presented a case of COM by Kerstersia gyiorum, the third case described resistant to ciprofloxacin.
Case Presentation
The case is a male patient, 88 years old, with a history of type 2 diabetes mellitus, hypertension, dyslipidemia, chronic renal failure, chronic heart failure and prostatic hypertrophy. In 2004, he was diagnosed a right tympanic perforation and otorrhea with good clinical outcome after medical treatment.
In May 2016, the patient went to his family doctor complaining of a right otalgia and otorrhea for three weeks and being referred to an ENT specialist. Then, the presence of a foreign body (cotton) in the right ear canal and a tympanic perforation already known was shown. The foreign body was removed and topical corticosteroids (solution dipropionate/ clioquinol beclomethasone; Menaderm eardrops® 0.25 mg/10 mg/ml, 3 drops tid, 7 days) were prescribed and monthly reviews were scheduled.
After persistent otorrhea, two regimens of topical ciprofloxacin (Cetraxal ótico® 1.2 mg/0.4 ml solution ear drops, 3 drops tid, 7 days) are prescribed. So this torpid evolution the patient was again referred to an ENT specialist on July. After his physical exam, a profuse suppuration inside the right ear was observed and a sample of the exudate was taken for microbiological studies.
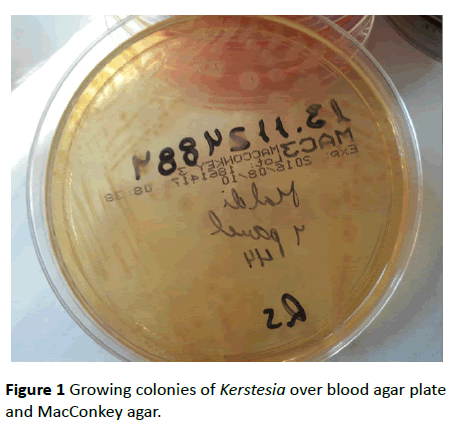
Direct Gram stain showed Gram-positive Cocci and Gramnegative Bacilli but no leukocytes. After incubation for 24 h, a few colonies of Staphylococcus aureus were isolated on Columbia agar (Oxoid, Germany) and Chocolate agar (Chocolate Agar Base, GC Medium, BD DifcoTM, Beckton Dickinson, US). In all media including MacConkey agar (No. 3, Oxoid, Germany), abundant slightly convex colonies with extended edges, colorful from gray hue to clear lavender (Figure 1), oxidase and catalase negative and indol positive were isolated. In the Gram stain from the grown colonies, gram-negative bacilli were observed and then identified by mass spectrometry using the technique of MALDI-TOF (matrixassisted laser desorption ionization time-of-flight) Biotyper 3.1 (Bruker Daltonic GmbH, Bremen, Germany) as Kerstersia gyiorum with a score of 2.1.
Figure 1 Growing colonies of Kerstesia over blood agar plate and MacConkey agar.
Antibiotic susceptibility test (Table 1) was performed by broth microdilution method using the automated system MicroScan WalkAway® (Siemens Healthcare, Spain currently Beckman Coulter) and the MicroScan® panels (Neg MIC Panel Type 44) were used. The interpretation of the minimum inhibitory concentration (MIC) was performed according to the breakpoints for non-Enterobacteriaceae gram-negative bacilli set by CLSI (Clinical and Laboratory Standards Institute) [6].
| Antibiotic |
MIC (µg/mL) |
Interpretationa |
| Cefotaxime |
≤ 1 |
S |
| Ceftazidime |
≤ 1 |
S |
| Cefepima |
≤ 1 |
S |
| Gentamicin |
≤ 2 |
S |
| Tobramicin |
≤ 4 |
S |
| Amikacin |
≤ 8 |
S |
| Piperacilin-tazobactam |
≤ 8 |
S |
| Trimetoprim-sulfametoxazol |
≤ 2/38 |
S |
| Meropenem |
≤ 1 |
S |
| Imipenem |
≤ 1 |
S |
| Ciprofloxacin |
>2 |
R |
| Levofloxacin |
>4 |
R |
Table 1 Antibiotic susceptibility profile.
Isolates were susceptible to cefotaxime ≤ 1 μg/ml, ceftazidime ≤ 1 μg/ml, cefepime ≤ 1 μg/ml gentamicin ≤ 2 μg/ml, tobramycin ≤ 2 μg/ml, amikacin ≤ 8 μg/ml, piperacillintazobactam ≤ 8 μg/ml tetracycline ≤ 4 μg/ml, trimethoprimsulfamethoxazole ≤ 2/38 g/ml, meropenem ≤ 1 μg/ml, imipenem ≤ 1 μg/ml and resistant to ciprofloxacin >2 μg/ml and levofloxacin >4 μg/ml.
K. gyiorum identification was confirmed by sequencing the 16S rRNA gene. The sequence was 99.8% identical to K. gyiorum type strain LMG …… using the NCBI 16S rRNA gene database.
After antibiotic susceptibility report was known, the patient was treated with topical gentamicin (gentamicin/ dexamethasone eye drops solution Colircusi Gentadexa® 1/3 / 0.5 mg, 3 drops tid) plus oral cloxacillin (cloxacillin 500 mg, 1 tablet tid) for 7 days. After that, a clinical improvement and otorrhea dry up was clearly observed.
Discussion
Kerstersia genus belongs to the family Alcaligenaceae. It includes two kinds of species (Kerstersia gyiorum and Kerstersia similis). It is a gram-negative, small (1-2 μm), coccobacilli in pairs or short chains. It grows well on standard culture media between 28 and 42°C. On nutrient agar, the colonies are flat or slightly convex with smooth edges and white to light brown. They are strict aerobes, non- fermenter, catalase positive [7,8]. The biochemical features of our strain were similar to those reported in the literature.
K. gyiorum appears as a human pathogen described in the literature reviewed in nine occasions, being isolated from urine samples [9], ulcers [10,11] sputum [12] and causing chronic otitis in five cases [2-5].
The first isolation associated with chronic otitis was reported in 2012 by Almuzara et al. It was in a 16 years-oldmale patient diagnosed with chronic otitis media associated to cholesteatoma [2]. In the other cases K. gyiorum has been isolated together with other microorganisms, being difficult to determine its pathogenic role attributable solely to K. gyiorum (Table 2).
| Reference |
Age |
Background |
Isolation in culture |
Ciprofloxacin
(MIC µg/mL) |
Directed therapy |
Outcome |
| [2] |
16 |
- AOM and retroauricular abscess
-Overcrowding and unhealthy conditions |
Monomicrobial |
1(S) |
Ceftriaxone 2 g iv then
Ciprofloxacin 500 mg bid po plus Amoxicilin/clavulanic, 1 g bid po |
Favourable |
| [3] |
55 |
- Otorrhoea in childhood
-Smoking
-Bilateral mastoid surgery |
Polymicrobial Corynebacterium amycolatum |
>32(R) |
Trimetoprim/sulfametoxazol |
Favourable |
| [4] |
53 |
- Chronic otorrhea in adulthood
-Smoking |
Polymicrobial Proteus mirabilis |
1 (I) |
Topical ciprofloxacin |
Favourable |
| [4] |
33 |
- Chronic otorrhea in adulthood |
Polymicrobial Staphylococcus aureus E. coli |
1 (I) |
Topical ciprofloxacino |
Favourable |
| [5] |
25 |
- Otorrhoea
In childhood |
Polymicrobial Pseudomonas aeruginosa |
>2 (R) |
Imipenem 500 mg/qid iv,
10 days |
Favourable |
| Present Case |
88 |
- Chronic otorrhea in adulthood
- Tympanum drilling |
Polymicrobial
Staphylococcus aureus |
>2 (R) |
Topical gentamicin
Cloxacilin po 500 mg tid
7 days |
Favourable |
Table 2 Summary of reported cases of chronic otitis media caused by K. gyioruma.
In our case, Staphylococcus aureus was also isolated however we considered Kerstersia gyiorum as a true pathogen in view of the chronicity of the disease, the poor response to treatment with ciprofloxacin, the observation of bacilli in the Gram stain and, the abundant growth into the inoculated plates. The cases reported so far in literature, were patients with chronic ear disease, as our patient, so it is deductible K. gyiorum has a pathogenic role in these patients. In our case there was no history of smoking or overcrowded conditions, described by other authors [2-4].
Currently, the identification of new species by MALDI-TOF and 16S rRNA sequencing are essential for microbiological diagnosis.
There are no cutoffs of antibiotic susceptibility in CLSI or EUCAST (European Committee on Antimicrobial Susceptibility Testing) specific to this genus. We used the CLSI criteria for non-Enterobacteriaceae.
According to Harris et al. [13] about the use of quinolones and aminoglycosides in the treatment of chronic suppurative otitis media, quinolones are bactericidal allowing different routes of administration and therefore outpatient treatments. They also are less ototoxic than aminoglycosides and have the same efficacy in resolving otorrhea all of which makes them a first-line option in chronic otitis, especially in cases with tympanic perforation.
Kerstersia isolates are generally susceptible to ciprofloxacin and cefotaxime [8] although recently there have been described two strains resistant to ciprofloxacin [3,5]. Treatment failure is considered when otorrhea persists approximately three weeks after medical therapy. Causes of failure include the presence of resistant microorganisms, the presence of cholesteatoma or a poor adherence to treatment, being therefore necessary a microbiological analysis including an antibiotic susceptibility study [14].
Our case would be the third case resistant to ciprofloxacin reported in the literature. The prior long treatment with ciprofloxacin may be the clue of further selection of resistant strains.
In summary, K. gyiorum is therefore a novel pathogen to be considered in the differential diagnosis of microorganisms causing chronic otitis media.
Microbiological diagnosis is the important key to guide the antimicrobial treatment because of the lack of homogeneity in its antibiotic susceptibility.
Conflict of Interest
The authors declare not to have an association that might pose a conflict of interest.
There is no fund, non-financial support received by the authors of the manuscript.
References
- Mittal R, Lisi CV, Gerring R, Mittal J, Mathee K, et al. (2015) Current concepts in the pathogenesis and treatment of chronic suppurative otitis media. J Med Microbiol 64: 1103-1106.
- Almuzara MN, Barberis CM, Traglia GM, Ordonez AM, Famiglietti AMR, et al. (2012) Isolation of Kerstersia gyiorum from a Patient with Cholesteatomatous Chronic Otitis Media. J Clin Microbiol 50: 3809-3811.
- Pence MA, Sharon J, Elvania TE, Pakalniskis BL (2013) Two Cases of Kerstersia gyiorum Isolated from Sites of Chronic Infection. J Clin Microbiol 51: 2001-2004.
- Mwalutende A, Mshana SE, Mirambo MM, Mushi MF, Chalya PL, et al. (2014) Two cases of chronic suppurative otitis media caused by Kerstersia gyiorum in Tanzania: is it an underappreciated pathogen in chronic otitis media. Int J Infect Dis 29: 251-253.
- Uysal EB, Celik C, Tuzcu N, Can F, Dogan M, et al. (2015) A case of chronic suppurative otitis media caused by Kerstersia gyiorum. APMIS 123: 986-989.
- CLSI (2016) Performance standards for antimicrobial susceptibility testing 26th ed. CLSI supplement M100S. Clinical and Laboratory Standards Institute, Wayne, PA,USA.
- Wirsing C, Riffelmann M, Coenye TB, Pfaller MA, Richter SS (2015) Manual of Clinical Microbiology 11th ed. Washington DC. American Society of Microbiology 838-850.
- Coenye T (2003) Kerstersia gyiorum gen. nov., sp. nov., a novel Alcaligenes faecalis-like organism isolated from human clinical samples, and reclassification of Alcaligenes denitrificans Ruger and Tan 1983 as Achromobacter denitrificans comb. nov. Int J Syst Evol Microbiol 53: 1825-1831.
- Ogawa Y, Lee ST, Kasahara K, Koizumi A, Chihara Y, et al. (2016) A first case of isolation of Kerstersia gyiorum from urinary tract. J Infect Chemother 22: 265-267.
- Greninger AL, Kozyreva V, Truong CL, Longoria R, Chaturvedi V (2015) Draft Genome Sequence of Kerstersia gyiorum CG1, Isolated from a Leg Ulcer. Genome Announc 3: e01036-15.
- Bostwick AD, Zhang C, Manninen K, Touchberry J, Greene SR, et al. (2015) Bacteremia Caused by Kerstersia gyiorum. J Clin Microbiol 53: 1965-1967.
- Deutscher M, Severing J, Balada L (2014) Kerstersia gyiorum Isolated from a Bronchoalveolar Lavage in a Patient with a Chronic Tracheostomy. Case Rep Infect Dis 1-3.
- Harris AS, Elhassan HA, Flook EP (2016) why are ototopical aminoglycosides still first-line therapy for chronic suppurative otitis media? A systematic review and discussion of aminoglycosides versus quinolones. J Laryngol Otol 130: 2-7.
- Karov I (1996) Preoperative treatment of children with chronic suppurative otitis media. Folia Med (Plovdiv) 38: 63-69.