Murugesan Raju1*, Matthew Chisholm2, Abu Saleh Mohammad Mosa3,4, Chi-Ren Shyu4 and Frederick W Fraunfelder1*
1Department of Ophthalmology, Mason Eye Institute, University of Missouri School of Medicine, Columbia, Missouri, USA
2Department of Biomedical Engineering, University of Missouri, Columbia, Missouri, USA
3Health Management and Informatics, University of Missouri, School of Medicine, Columbia, Missouri, USA
4MU Informatics Institute, University of Missouri, Columbia, Missouri, USA
*Corresponding Authors:
Murugesan Raju
Department of Ophthalmology, Mason Eye Institute
University of Missouri School of Medicine, Columbia, Missouri, USA
Tel: 573-882-8481
Fax: 573-884-4100
E-mail: rajum@health.missouri.edu
Frederick W Fraunfelder
Department of Ophthalmology, Mason Eye Institute
University of Missouri School of Medicine, One Hospital Drive
Columbia, Missouri, USA
Tel: 573-882-1029
Fax: 573-884-5575
E-mail: fraunfelderf@health.missouri.edu
Received date: January 09, 2017; Accepted date: February 15, 2017; Published date: February 20, 2017
Citation: Raju M, Chisholm M, Mohammad Mosa AS, Chi-Ren Shyu, Frederick W Fraunfelder (2017) Investigating Risk Factors for Cataract Using the Cerner Health Facts® Database. J Eye Cataract Surg 3:19. doi: 10.21767/2471-8300.100019
Copyright: © 2017 Raju M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Cataract; Risk factor; Lacrimal disorders, Lens, Disease
Introduction
The human lens is located at the anterior part of the eye and is made of a high concentration of crystalline protein that focuses the image of the visual field on the retina [1]. With little protein turnover, crystalline protein in the lens must survive for a lifetime of an individual, leading to a reduction of focusing ability and lens transparency with age. This reduction is a result of the long living crystalline proteins being continuously challenged by endogenous and exogenous agents that drive the lens proteins to undergo a wide variety of alteration and eventually form larger light scattering aggregates [2,3]. Clinically significant alteration and formation of larger light scattering aggregates leads to the development of cataract. Cataract may also occur either from congenital due to mutation in genetic materials or from traumatic incidents. However, most cataracts are age related. Cataracts can be broadly classified into nuclear cataract, cortical cataract and sub capsular cataract based on the anatomy location and pathophysiology. According to the World Health Organization, cataracts are the leading cause of blindness among people age 40 and above worldwide [4]. The economic burden of cataract has been rising worldwide [5], however, the actual cause for increased prevalence of cataract is not known. Studies have suggested that it either could be due to age demographic shifts upward in the population or increased exposure to risk factors that accelerates development of lens opacification. In the United States, the prevalence of cataracts rose by 20% from 20.5 million in 2000 to 24.4 million in 2010 and is expected to double by 2050 [6]. Consequently, the Medicare cost for treatment of cataract is continually increasing [7]. A study by the World Health Organization showed that a delay of 10 years of the onset of cataracts would cut the number of people who need cataract surgery in half [8]. Therefore, understanding the risk factors associated with cataract would pave the way for better preventive measure, which may help to delay the onset of cataracts and subsequently decrease the financial burden of this disease.
A literature review revealed that the severity of the light scattering aggregates in the lens is accelerated by several factors including lifestyle, educational status, medication, smoking, sunlight exposure, diabetes, body mass index, tobacco use, alcohol consumption, and many other risk factors [9,10]. It also suggested possible protective factors including intake of anti-oxidants, higher physical activity, and use of certain medications such as aspirin, beta-carotene, and multivitamins [11,12] however, the conclusions from a large number of studies are inconsistent [10]. Thus, there is a necessity for a more robust approach which looks at a large number of patients to determine risk factors for the development of cataracts.
To determine risk factors for cataracts, data available in the Cerner Health Facts® database was utilized. The database captures and stores de-identified, longitudinal electronic health records (EHR) which includes data on patient demographics, encounter, diagnosis, medications, procedures, laboratory tests, hospital information, and billing. This database facilitated a unique opportunity to study more patient variables than previously possible. The aim of this study was to identify potential risk factors for the development of cataracts.
Methods
Data source
This study utilized the Cerner Health Facts® electronic database which complies with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act (HIPAA). Data in Health Facts is extracted directly from the EMR from hospitals in which Cerner has a data use agreement. Encounters may include pharmacy, clinical and microbiology laboratory, admission, and billing information from affiliated patient care locations. All admissions, medication orders and dispensing, laboratory orders and specimens are date and time stamped, providing a temporal relationship between treatment patterns and clinical information. Cerner Corporation has established operating policies consistent with the HIPAA Laws to establish de-identification for Health Facts. The database contains unique clinical data on more than 48.9 million patients and uses an automated electronic medical record system to capture clinical events. Over 600 individual sites from 90 health systems participate in contributing data to the database. MU has agreements with Cerner’s to use this data for research purposes. The institutional review board (IRB) at the University of Missouri approved the study protocol.
Study cohort
All patients diagnosed with an eye-related disease, age 35 and above, were included in this study to investigate risk factors for cataracts. Eye-related visits were determined using ICD-9 codes (361-379) and those with cataracts were then identified using ICD-9 ontology codes (366.01-366.04 and 366.10-366.19). Congenital cataract and traumatic cataracts were not included for this study. Data was extracted on the resulting 947,059 patients.
Inclusion/ exclusion criteria
Data processing was performed to ensure the quality of the data. Patients with incomplete demography information were excluded from analysis, reducing the study to 830,125 patients. Patients with none of the selected risk factors were also excluded from the study, yielding a total of 699,680 unique patients for odds ratio analysis.
Risk factor assessment
A data-driven approach was used to determine risk factors. The medication and diagnosis tables were summarized and variables that had at least 4% of the samples were selected from each table. From the summarized tables, variables were selected, these included hypertension, lipoid metabolism disorder, diabetes type I & II, glaucoma, obesity, ischemic heart disease, hypotension, atherosclerosis, lacrimal disorder, aspirin, multivitamins, steroids, atropine, bacitracin, gentamicin, allopurinol and alcohol use.
Statistical analysis
The association between cataract and potential risk factors was assessed by univariate analysis. Odds ratio (ORs) and 95% confidence interval (CI) were calculated using SAS software package (version 9.4 SAS Institute Inc) to determine risk factors. Risk factors were chosen that had 20% higher incidence in the cataracts patients group compared to patients without cataract.
Results
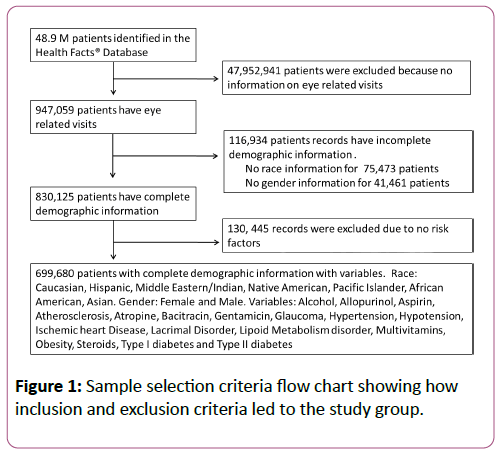
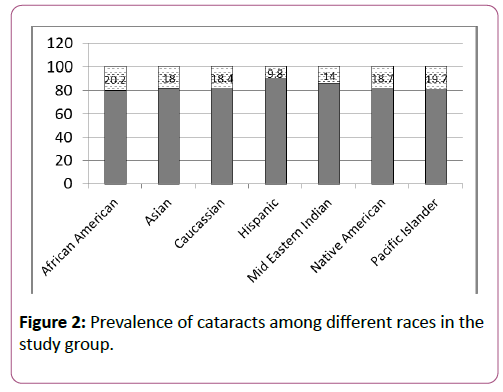
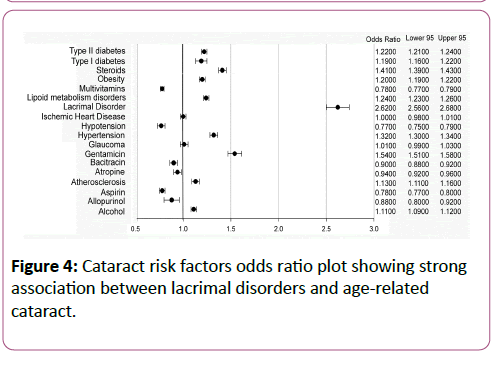
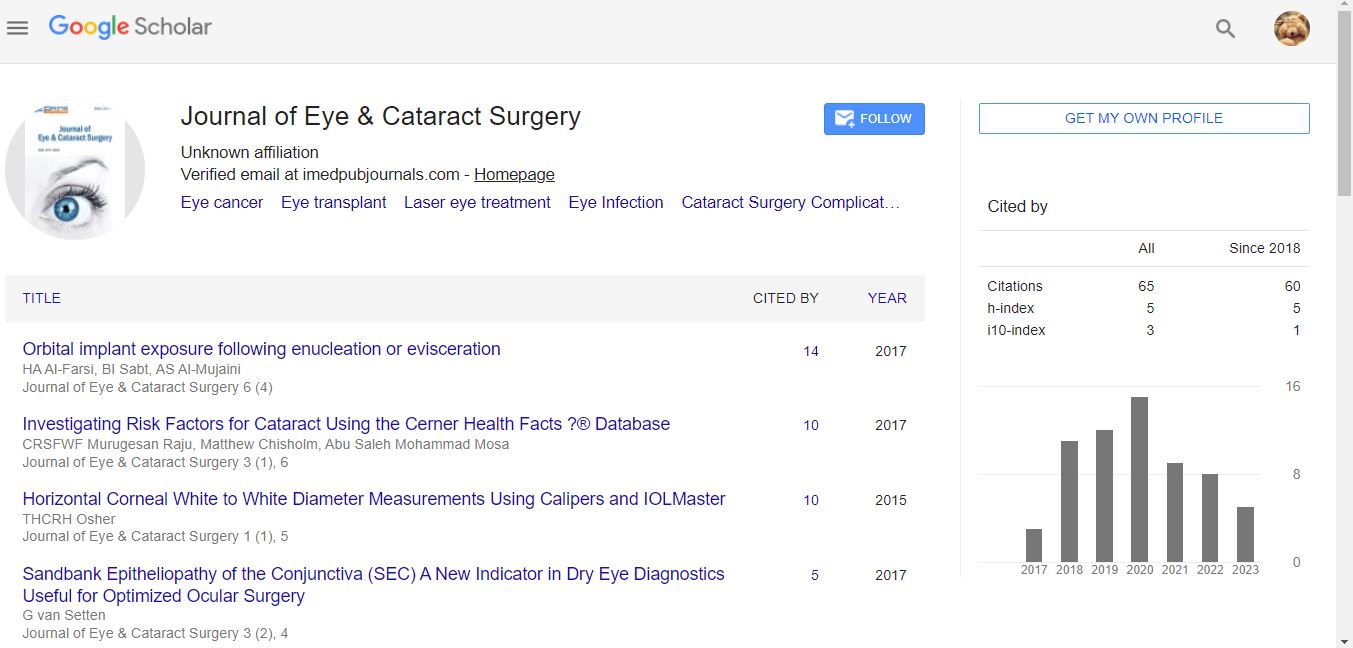
A total of 699,680 patients with cataract were identified from the Cerner Health Facts® database from 2000 to 2015 that satisfied inclusion/exclusion criteria of the study (Figure 1). The study group was 58% female (age range 35-93 years) and 42% male (age range 35-89 years) (Table 1). The majority of individuals were aged 60 years and higher at the time of cataract diagnosis. Gender based analysis showed that 19% of females and 18% of males were diagnosed with cataracts. Race distribution of those diagnosed with cataracts was 20.2% of African-Americans, 19.7% of Pacific Islanders, 18.7% of Native Americans, 18.4% of Caucasians, 18.0% of Asians, 14% of Middle Eastern Indians, and 9.8% of Hispanics (Figure 2).
Figure 1: Sample selection criteria flow chart showing how inclusion and exclusion criteria led to the study group.
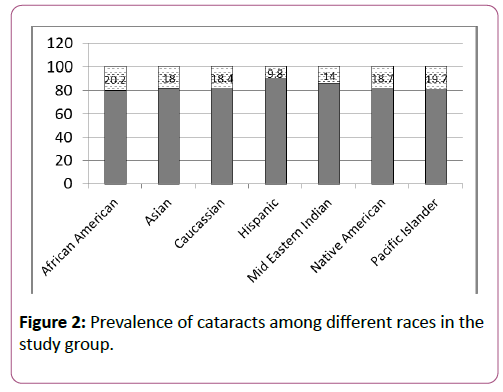
Figure 2: Prevalence of cataracts among different races in the study group.
| |
|
Total patients |
Cataract |
No Cataract |
| |
|
N |
% |
N |
% |
N |
% |
| Gender |
Total |
699680 |
100 |
130678 |
18.67 |
569002 |
81.32 |
| Female |
408697 |
58.42 |
78322 |
11.19 |
330375 |
47.21 |
| Male |
290983 |
41.58 |
52356 |
7.48 |
238627 |
34.1 |
| Race |
Total |
699680 |
100 |
130678 |
18.67 |
569002 |
81.32 |
| African American |
137231 |
19.61 |
27728 |
3.962 |
109503 |
15.65 |
| Asian |
13382 |
1.91 |
2404 |
0.343 |
10978 |
1.56 |
| Caucasian |
534517 |
76.39 |
98600 |
14.09 |
435917 |
62.3 |
| Hispanic |
8649 |
1.23 |
845 |
0.123 |
7804 |
1.11 |
| Mid-Eastern Indian |
157 |
0.02 |
22 |
0.003 |
135 |
0.01 |
| Native American |
5268 |
0.752 |
985 |
0.14 |
4283 |
0.61 |
| Pacific Islander |
476 |
0.068 |
94 |
0.013 |
382 |
0.05 |
Table 1: The study group was 58% female (age range 35 -93 years) and 42% male (age range 35-89 years).
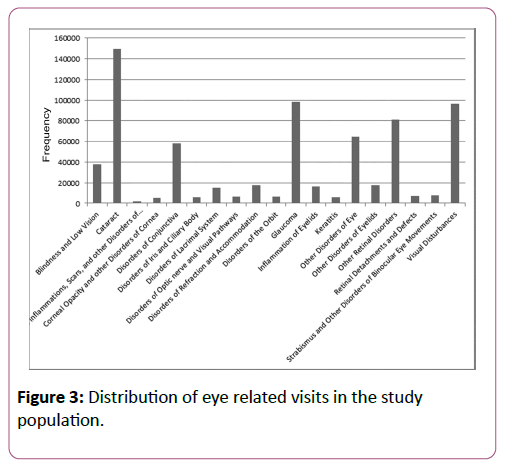
The distribution pattern of eye disease among the study population were as follows: cataract (21.34%), glaucoma (14.04%), visual disturbances (13.74%), other retinal disorders (11.64%), other disorders of the eye (9.20%), disorders of the conjunctiva (5.43%), blindness and low vision (5.43%), other disorders of eyelids (2.53%), disorders of refraction and accommodation (2.49%), inflammation of eyelids (2.40%), disorders of the lacrimal system (2.12%), strabismus and other disorders of binocular eye movements (1.13%), retinal detachments and defects (1.03%), disorders of optic nerve and visual pathways (0.9403%), disorders of the orbit (0.922%), keratitis (0.893%), disorders of the iris and ciliary body (0.840%), corneal opacity and other disorders of cornea (0.815%), chorioretinal inflammation, scars, and other disorders of choroid (0.223%) (Figure 3).
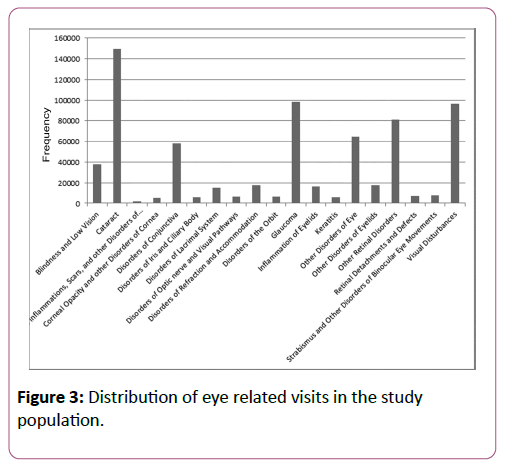
Figure 3: Distribution of eye related visits in the study population.
This study looked at 18 different variables to determine their effect on cataract formation (Figure 4). Odds ratio analysis showed that 7 out 18 variables had a 20% or higher odds of a cataract diagnosis: gentamicin (OR 1.54-95% CI 1.51-1.58), hypertension (OR 1.32-95% CI 1.30-1.34), lacrimal disorder (OR 2.62 95% CI 2.56-2.68), lipoid metabolism disorder (OR 1.24-95% CI 1.23-1.26), obesity (OR 1.20-95% CI 1.19-1.22), steroids (OR 1.41-95% CI 1.39-1.43), and type-two diabetes (OR 1.22 95% CI 1.21-1.24). The type-one diabetes, is close to the 20% cut off (OR 1.19-95% CI 1.16-1.22). It was determined that 3 factors had lower than 20% odds of cataract association: aspirin (OR 0.78-95% CI 0.77-0.80), multivitamins (OR 0.78-95% CI 0.77-0.79), and hypotension (OR 0.77 95% CI 0.75-0.79).
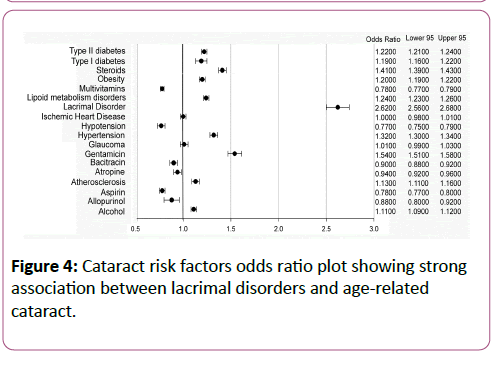
Figure 4: Cataract risk factors odds ratio plot showing strong association between lacrimal disorders and age-related cataract.
Discussion
This study utilized Cerner Health Facts® database to investigate risk factors for cataract. Several others studies, ranging from case-control to population-based, have also attempted to investigate these factors [13-18]. West et al. performed a meta-analysis and addressed several risk factors including education, gender, smoking, alcohol, blood pressure/ hypertension, ultraviolet radiation, and diabetes [10]. Older age is also widely reported as a vital risk factor [10,19,20]. Odds Ratio analysis in this study identified 7 risk factors with a 20% or higher odds of leading to cataract. Of these 7 risk factors, 6 have also been identified in the literature: gentamicin, hypertension, lipid metabolism disorder, obesity, steroids and type-two diabetes. Most significant is that this study identified lacrimal disorders as a risk factor. This is the first report of lacrimal disorders being linked to cataract formation.
Hypertension is a well-known risk factor for cataract [10,21]. It may be possible that blood pressure is a surrogate for the cataractogenic effects of certain anti-hypertensive medications [22]. Tyler Rim et al. have reported the results of the Korean National Health and Nutrition Survey and found that hypercholesterolemia, a type of lipoid metabolism disorder, is a risk factor for cataract development [23]. Many studies have shown that type two diabetes is associated with significantly higher odds of developing cataracts [19,20,24,25]. However, the colloquial is what causes the increased cataract among the diabetic patients is not known, whether it is just the elevated sugar level or a subsequent complication of the disease. The biochemical analysis of cataract lenses in patients with diabetes showed abnormalities in the levels of electrolytes, glucose, galactose, and glutathione and can lead to hypersonic effects like fiber cell swelling, vacuole formation, and lens opacification [26-28]. The consensus in the literature is that steroids are a risk factor for cataracts [10,29]. While widely accepted as a risk factor, the mechanism behind steroid-induced cataract formation is not generally agreed upon. Studies have shown an association between gentamicin toxicity and vision loss [30] however its role in the development of cataracts is unknown. Overall there are mixed views about obesity in the literature [31-33]. Our study found all 6 of these risk factors to have 20% or high odds of leading to development of cataract.
This study is the first to show that lacrimal disorders have a strong positive correlation with cataract (OR 2.62 95% CI 2.56-2.68). It is well known that a lacrimal disorder is associated with dry eye syndrome. The lacrimal gland contributes multiple components to the tear film to maintain the health and transparency of the eye and it may have a role on lens opacity as well. Further study is required to understand the biological consequence of lacrimal disorders and its association with the development of cataract. It important for physicians to create awareness amongst patients who have lacrimal disorders, as consequentially they may be at a higher risk to develop cataract. Routine follow-up and preventive measure will enable them to delay or take timely care of the cataract.
Beyond these 7 risk factors, several others have been investigated including: gender, ethnicity, alcohol consumption, multivitamin and aspirin use. Studies have found altered occurrence of lens opacities among menopausal women who have had hormonal therapy, suggesting a hormonal influence involved in lens opacification. This study showed negligible difference in the prevalence of cataract between males (18%) and females (19%). Eye Disease Study (AREDS) reported that age, gender, education, smoking, and diabetes are strong risk factors for cataracts [19]. Their study also reported that African Americans were at a higher risk of developing cataracts than Caucasians. The present study found in increased incident of cataract among African Americans compared to other ethnic groups. The race-based data reveals that the Hispanic race has less prevalence of cataract among the study groups. The reason behind this trend is unknown, but it could be due to lack of eye clinic visits among the Hispanic population due to their socioeconomic status. The literature has mixed results on alcohol's effect on cataract formation. Some affirm that light drinking is a protective factor [10], while others say that drinking is a risk factor [8,15,34]. West et al. reported that only heavy drinking is a risk factor for cataract development [10]. This study found that alcohol is associated with marginally higher odds of cataract formation. The underlying mechanism of how alcohol induces cataract is not clear. It has been suggested in the literature that conversion of alcohol to acetaldehyde is a harmful factor as the acetaldehyde can react with lens proteins and form light scattering changes [35]. Studies have shown that multivitamins offer a protective effect against cataract development [19,36,37], while another has shown that there was no protective effect [38]. This study found that multivitamins are associated with lower odds of cataract development. It is important to determine what part of these vitamins is leading to the reduction in cataracts. Similarly, aspirin has mixed reports in the literature. A few studies have shown a protective effect [19] and others reported no effect [10]. Gritz et al. reported that aspirin is a risk factor of cataract [34]. This study found that aspirin is associated with significantly lower odds of cataract development. The proposed mechanism of aspirin mediated protection against cataract formation is not known, however studies have shown that lowering plasma tryptophan levels and reduced aldose reductase activity may be involved [39]. Further, the use of allopurinol suggested that it may be a risk factor for cataract formation [40]. A proposed mechanism for allopurinol reducing the odds of cataract formation is through the inhibition of the antioxidant xanthine oxidase. This study shows no association between allopurinol and development of cataract. Studies have shown also that excess of antioxidants are also risk factors for cataract [41-43].
While there are many advantages of a retrospective analysis including large population size, ability to study more variables, and a constant database that others can analyze, there are some limitations to the study. The information available is limited by the data that the hospitals provide. Data is also limited to institution and geographical regions that Cerner’s reporting hospitals serves. There is also incomplete history on the patients in the database and patients may have other conditions or have been diagnosed earlier and it was not recorded in the database. Longitudinal information varies between patients as well. For instance, some patients may have 15 years of information while others only have 3 years of data. Another limitation does not know the length of exposure or frequency of the drug used. While these limitations are typical of a retrospective analysis, the conclusions are still significant.
Acknowledgments
Matthew Chisholm expresses his sincere thanks to Dr. Calyam Prasad of the Computer Science Department for financial support. We thank Bree Jensvold-Vetsch for providing editing services during the preparation of the manuscript.
References
- Iribarren R, Morgan IG, Nangia V, Jonas JB (2012) Crystalline lens power and refractive error. Invest Ophthalmol Vis Sci 53: 543-550.
- Baruch A, Greenbaum D, Levy ET, Nielsen PA, Gilula NB, et al. (2001) Defining a link between gap junction communication, proteolysis, and cataract formation. J BiolChem 276: 28999-29006.
- Bassnett S (1997) Fiber cell denucleation in the primate lens. Invest Ophthalmol Vis Sci 38: 1678-1687.
- WHO (2010) Global Data on Visual Impairments 2010 (WHO/NMH/PBD/12.01) world Health Organization, Geneva.
- Pascolini D, Mariotti SP, Pokharel GP, Pararajasegaram R, Etya'ale D, et al, (2004) 2002 global update of available data on visual impairment: a compilation of population-based prevalence studies. Ophthalmic Epidemiol 11: 67-115.
- https://neinihgov/eyedata accessed October 2016.
- Salm M, Belsky D, Sloan FA (2006) Trends in cost of major eye diseases to Medicare, 1991 to 2000. Am J Ophthalmol 142: 976-982.
- Brian G, Taylor H (2001) Cataract blindness--challenges for the 21st century. Bull World Health Organ 79:249-256.
- Foster PJ, Wong TY, Machin D, Johnson GJ, Seah SK (2003) Risk factors for nuclear, cortical and posterior subcapsular cataracts in the Chinese population of Singapore: the TanjongPagar Survey. Br J Ophthalmol 87:1112-1120.
- West SK, Valmadrid CT (1995) Epidemiology of risk factors for age-related cataract. Surv Ophthalmol 39:323-334.
- Mamatha BS, Nidhi B, Padmaprabhu CA, Pallavi P, Vallikannan B (2015) Risk Factors for Nuclear and Cortical Cataracts: A Hospital Based Study. J Ophthalmic Vis Res 10:243-249.
- Williams PT (2009) Prospective epidemiological cohort study of reduced risk for incident cataract with vigorous physical activity and cardiorespiratory fitness during a 7-year follow-up. Invest Ophthalmol Vis Sci 50:95-100.
- Gunnlaugsdottir E, Arnarsson A, Jonasson F (2008) Prevalence and causes of visual impairment and blindness in Icelanders aged 50 years and older: the Reykjavik Eye Study. Acta Ophthalmol 86:778-785.
- Jonas JB, Xu L, Wang YX (2009) The Beijing Eye Study. Acta Ophthalmol 87:247-261.
- Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT (1998) Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol 116:653-658.
- Klein R, Klein BE (2013) The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci 54: 5-13.
- Mitchell P, Cumming RG, Attebo K, Panchapakesan J (1997) Prevalence of cataract in Australia: the Blue Mountains eye study. Ophthalmol ogy 104:581-588.
- Rosman M, Zheng Y, Lamoureux E, Saw SM, Aung T, et al. (2012) Review of key findings from the Singapore Malay Eye Study (SiMES-1). Singapore Med J 53:82-87.
- Chang JR, Koo E, Agron E, Hallak J, Clemons T, et al. (2011) Risk factors associated with incident cataracts and cataract surgery in the Age-related Eye Disease Study (AREDS): AREDS report number 32. Ophthalmol ogy 118:2113-2119.
- Richter GM, Choudhury F, Torres M, Azen SP, Varma R, et al. (2012) Risk factors for incident cortical, nuclear, posterior subcapsularand mixed lens opacities: the Los Angeles Latino eye study. Ophthalmol ogy 119:2040-2047.
- Yu X, Lyu D, Dong X, He J, Yao K (2014) Hypertension and risk of cataract: a meta-analysis. PLoS One 9:e114012.
- Rodriguez-Sargent C, Berrios G, Irrizarry JE, Estape ES, Cangiano JL, et al. (1989) Prevention and reversal of cataracts in genetically hypertensive rats through sodium restriction. Invest Ophthalmol Vis Sci 30:2356-2360.
- Rim TH, Kim MH, Kim WC, Kim TI, Kim EK (2014) Cataract subtype risk factors identified from the Korea National Health and Nutrition Examination survey 2008-2010. BMC Ophthalmol 14:4.
- Congdon NG (2001) Prevention strategies for age related cataract: present limitations and future possibilities. Br J Ophthalmol 85:516-520.
- Waudby CJ, Berg RL, Linneman JG, Rasmussen LV, Peissig PL, et al. (2011) Cataract research using electronic health records. BMC Ophthalmol 11:32.
- Bhatnagar A, Srivastava SK (1992) Aldose reductase: congenial and injurious profiles of an enigmatic enzyme. Biochem Med MetabBiol 48:91-121.
- Drel VR, Pacher P, Ali TK, Shin J, Julius U, et al. (2008) Aldose reductase inhibitor fidarestat counteracts diabetes-associated cataract formation, retinal oxidative-nitrosative stress, glial activation, and apoptosis. Int J Mol Med 21:667-676.
- Reddy PY, Giridharan NV, Reddy GB (2012) Activation of sorbitol pathway in metabolic syndrome and increased susceptibility to cataract in Wistar-Obese rats. Mol Vis 18:495-503.
- Na KS, Park YG, Han K, Mok JW, Joo CK (2014) Prevalence of and risk factors for age-related and anterior polar cataracts in a Korean population. PLoS One 9:e96461.
- Lartey S, Armah P, Ampong A (2013) A sudden total loss of vision after routine cataract surgery. Ghana Med J 47:96-99.
- Lee DS, Han K, Kim HA, Lee SY, Park YH, et al. (2015) The Gender-Dependent Association between Obesity and Age-Related Cataracts in Middle-Aged Korean Adults. PLoS One 10:e0124262.
- Pan CW, Lin Y (2014) Overweight, obesity, and age-related cataract: a meta-analysis. Optom Vis Sci 91:478-483.
- Park S, Kim T, Cho SI, Lee EH (2013) Association between cataract and the degree of obesity. Optom Vis Sci 90:1019-1027.
- Gritz DC (2001) Can cataracts be prevented? Bull World Health Organ 79:260-261.
- Harding JJ, van Heyningen R (1989) Beer, cigarettes and military work as risk factors for cataract. Dev Ophthalmol 17:13-16.
- Glynn RJ, Rosner B, Christen WG (2009) Evaluation of risk factors for cataract types in a competing risks framework. Ophthalmic Epidemiol 16:98-106.
- Seddon JM, Christen WG, Manson JE, LaMotte FS, Glynn RJ, et al. (1994) The use of vitamin supplements and the risk of cataract among US male physicians. Am J Public Health 84:788-792.
- Rautiainen S, Manson JE, Lichtenstein AH, Sesso HD (2016) Dietary supplements and disease prevention-a global overview. Nat Rev Endocrinol 12:407-420.
- Cotlier E, Sharma YR (1981) Aspirin and senile cataracts in rheumatoid arthritis. Lancet 1:338-339.
- Gupta VB, Rajagopala M, Ravishankar B (2014) Etiopathogenesis of cataract: an appraisal. Indian J Ophthalmol 62:103-110.
- Cui YH, Jing CX, Pan HW (2013) Association of blood antioxidants and vitamins with risk of age-related cataract: a meta-analysis of observational studies. Am J ClinNutr 98:778-786.
- Rautiainen S, Lindblad BE, Morgenstern R, Wolk A (2014) Total antioxidant capacity of the diet and risk of age-related cataract: a population-based prospective cohort of women. JAMA Ophthalmol 132:247-252.
- Wang A, Han J, Jiang Y, Zhang D (2014) Association of vitamin A and beta-carotene with risk for age-related cataract: a meta-analysis. Nutrition 30:1113-1121.