Keywords
Pharmaceutical business; Health policy; Clinical health; Health communication
Introduction
Common health communication issues and trends studied by our students include rising prescription drug costs and prices, direct-to-consumer advertising (DTCA), and the impact of recent regulations, including the Affordable Care Act of 2010 (ACA) and Health Information Technology for Economic and Clinical Health Act of 2009 (HITECH), on the U.S. Healthcare System. When students select topics related to health communication, they tend to focus on issues of platform integration for telemedicine (and telehealth) and dissemination of health information through the public health infrastructure. However, the most popular topic is DTCA; the use for patient awareness and the DTCA-associated costs in the drug development process. It is the opinion of this author that health communication needs to be a larger part of educating students in both graduate and undergraduate programs that focus on healthcare. The main reason for this perspective is that as providers, and the healthcare system at large are incentivized to communicate more effectively through use of e-systems, key healthcare stakeholders need to learn about the role of health communication before they enter the workforce. Further, as health and healthcare education integrates health communication into the curriculum, we should focus on the importance of interoperability because communication across our fragmented healthcare system should be a top priority.
Health System Evaluation
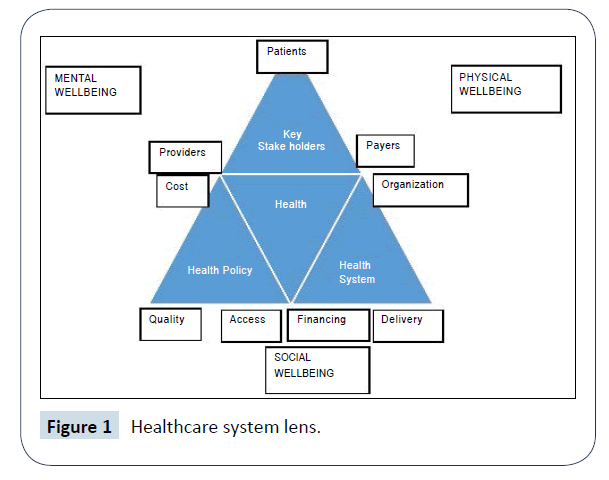
Before I go any further, I should address the lens through which I lecture students when focusing on healthcare systems. When evaluating health systems, we look at the convergence of the three main triangles of health care: 1) Stakeholders, 2) Systems, and 3) Policy (Figure 1). The stakeholder triangle represents the main players within a health system. It is composed of patients, providers, and payers. The second triangle describes how health systems are arranged and funded. The system triangle is composed of: 1) Financing, 2) Delivery, and 3) Organization [1]. The last triangle, policy, reflects the areas of healthcare that can be affected by policy makers. The health policy iron triangle is composed of: 1) Cost, 2) Quality, and 3) Access [2]. These three areas also represent the focus of experts describing the current issues and trends within health and healthcare. For the purpose of this paper, the World Health Organization’s (WHO) definition of ‘health’ is used, which describes health as the “complete physical, mental and social well-being and not merely the absence of disease or infirmity” [3].
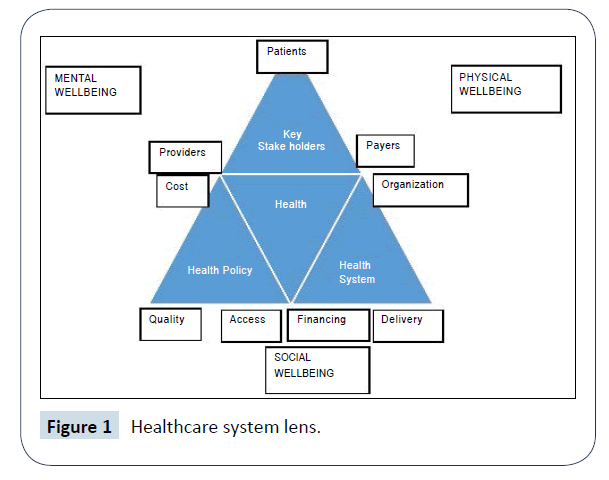
Figure 1: Healthcare system lens.
Triangles which are seldom brought together for a complete view of healthcare systems. Second, with this lens in place, it should be tautologous that health communication is an integral part of each of the outer triangles, which all converge to better the individual and population health. Or at least this is the hope of health system software like Electronic Health Records (EHRs). Evaluation of EHRs through the lens begs the question of whether or not all e-health systems communicate effectively.
A Fragmented Healthcare System and Interoperability
The organization of the U.S. Healthcare System is anything but centralized. This can be seen in evaluating the Financing and Stakeholder sections of the health system triangle (Figure 1). Financing of health care comes in many forms. There are public programs, also known as welfare programs, which are funded by the government through taxation. Medicare, Medicaid, the Veterans Affairs, and Indian Health Services are just a few examples of these public programs. Because there is a mixture of payers, providers can opt to participate in a mix of these programs resulting in ‘preferred provider’ networks and physicians that are ‘out-of-network’. There are private health insurers, which are usually employer-based, as well as government funded welfare programs. As a result of this patchwork, the organization of the U.S. Healthcare System is described as a mixed market.
In this mixed market, healthcare is a privilege and patients are described as consumers because they consume the healthcare products and services. In a more traditional sense of the role of consumer, U.S. patients also play the role of ‘payer’ in that they share the cost of health care with insurers through co-pays and deductibles. But the brunt of the cost is taken on by third party payers. On the provider side, they can be self-employed or work for a government program and/or participate in providing care for private and/or public programs. Providers can also opt to take no insurance programs and all their services are paid ‘outof- pocket’ by the patient. This, however, is the exception and not the rule.
This brief look at healthcare in the U.S. through the Healthcare System Lens shows just how complex and fragmented the U.S. System is with multiple payers, out-of-network services, and unknown coverage for primary care provider referred services. The last of which can be a shot in the dark without due diligence by the patient/consumer. And let us not forget that the due diligence is required on the part of the patient, who is seeking medical treatment when they are not feeling well, or may be incapacitated due to dramatic injury. The structure of healthcare may not be such a complex problem for policy wonks and the macro institutions of healthcare such as insurance companies and large health systems. These institutions have software with algorithms to protect their interests. But for the patient, their decisions can have devastating financial consequences.
Interoperability
For those outside the field of Health Communications, terms like interoperability or concepts like meaningful use are not well known. For the lay person who must navigate the U.S. Healthcare System in times of need, they are not aware and may not even care about The Office of National Coordinator for Health Information Technology’s 10-year initiative for Connecting Health and Care for the Nation [4]. This initiative lays out a strategic map that acknowledges the past and present state of health information technology, and attempts to address what is needed to meet the future of health information technology and interoperability head on. And why is this important? It is important because the U.S. Healthcare System is not a system at all, but a quilted patchwork of fragmented systems that do not communicate in a way which individuals can successfully navigate for routine care without the surprise of services being ‘not covered’ or ‘denied’.
Interoperability: what has been done?
To their credit, Epic Systems Corporation has collaborated with federal agencies on national interoperability [5]. Epic has developed EHRs that work within healthcare systems and with outside vendors such as central laboratories. And to the federal government’s credit, they continue to work towards international health information interoperability seen in their commitment to the Memorandum of Understanding between the Department of Health and Human Services and the European Commission [6]. Although Epic has been the most widely used EHR system for over 5 years, there are still over a thousand different healthcare information systems available and that number continues to grow. This begs the questions of whether or not 1,000-plus pieces of software can effectively communicate with one another.
The quick answer to this question is yes. Epic, along with other health information companies have been making strides towards interoperability. However, the main issue for comprehensive interoperability may not be whether software companies can make this happens, but instead whether healthcare organizations are purchasing and utilizing health information software effectively.
There are federal incentives for healthcare organizations to adopt health information software. But adoption is just one piece of the puzzle. The other measurable piece is effective use of the software. For example, under the HITECH (2009), in order to participate in Medicare and Medicaid HER Incentive programs, healthcare organizations had to show and meet the different levels of Meaningful Use of EHRs. In 2015, the Mathematica Policy Research and Harvard School of Public Health reported that approximately 75% of hospitals had adopted some form of EHRs, but many were not ready to meet the Meaningful Use criteria to attain federal incentives [7]. Although it could be argued, that there is more to be done, this study shows significant adoption of EHRs and the ability of hospitals to work towards attaining Meaningful Use goals through federal incentives. At the very least, this shows a national commitment by the largest component of healthcare expenditures (hospitals) to interoperability, which is promising [8].
Conclusion
It is a difficult task to evaluate the effectiveness of current health communication education in the United States. Colleges and Universities offer undergraduate and master’s degrees, PhD programs, and certificates in health communications. Additionally, healthcare organizations have developed ad hoc programs to internally train providers how to use EHRs. It’s hard to believe that healthcare system corporations have been involved with federal agencies since the 1960s and EHRs in their current form are approximately 25 years old. Still we ask the question of whether or not we are effectively using this technology. This situation must be put in context of incentives for using health information programs like EHRs. For example, uptake of EHRs, although an ongoing process, grew significantly over the last 8 years because HITECH (2009) called for adoption incentive programs based on Meaningful Use criteria [7].
The future of interoperability is here. Working together government and private enterprise can, and have to great extent, achieved interoperability. The nature of a fragmented system has caused multiple issues for healthcare in the U.S. Interoperability has been shown to work effectively through incentive programs brought about by clear health policy initiatives like HITECH. HITECH did catalyse the adoption of EHRs in the U.S. The next step is evaluating whether or not interoperability translates to better health and healthcare. And this is where health communication education comes into play.
The evolving nature of health communication in a post-HITECH world shows the needs for effective health communication programs. Now that the horse is out of the barn, educators and researchers need to start asking themselves questions about the validity, reliability, and meaningfulness of the data. And if the data meets this criterion, then what can be done with this information. Can data be used in conjunction with datasets like the Medical Expenditure Panel Survey to explore the cost-benefit relationship of the U.S. Healthcare System? Will the U.S. finally rid itself of the stigma from the WHO’s World Health Report 2000-Health Systems: Improving Performance where its health system was ranked 37th? [9-11] or will the data show the report accurate? These questions lead me to believe that we have moved on from whether or not health systems can communicate with one another. Instead we are moving on to what we can now do with this data and how we can better prepare tomorrow’s healthcare leaders to utilize this impressive advancement in health communication [12]. And more importantly, can we use technology to better serve the patient-consumer and alleviate the financial burden and uncertainties surrounding healthcare in the United States?
References
- Barr D (2007) Introduction to U.S. Health Policy: The Organization, Financing, and Delivery of Health Care in America (3rd edn.) Baltimore: Johns Hopkins University Press.
- Kissick W (1994) Medicine's dilemmas: Infinite needs versus finite resources. New Haven: Yale University Press.
- The World Health Organization (WHO) (1946) Preamble to the constitution of the world health organization as adopted by the international health conference. New York: World Health Orgainization.
- HealthIT.gov. (2014) Connecting health and care for the nation: a 10-year vision to achieve an interoperable health IT infrastructure. The office of the national coordinator for health information technology.
- https://www.healthit.gov/archive/archive_files/FACA%20Hearings/2014/2014-08-15%20Policy%3A%20Governance%20Subgroup/GSG_TestimonySupport_CarlDvorak_2014-08-15_04.pdf
- https://www.healthit.gov/sites/default/files/HHS_EC_MOU_CooperationHealthInfo_and_ComTechSigned.pdf
- https://www.rwjf.org/en/library/research/2015/09/health-information-technology-in-the-united-states-2015.html
- https://www.cdc.gov/nchs/fastats/health-expenditures.htm
- The World Health Organization (WHO) (2000) World health report 2000-health systems: improving performance. World Health Organization.
- Reeve C, Humphreys J, Wakerman J (2015) A comprehensive health service evaluation and monitoring framework. Eval Program Plann 53: 91-98.
- Boon H, MacPherson H, Fleishman S, Grimsgaard S, Koithan M, et al. (2007) Evaluating complex healthcare systems: a critique of four approaches. Evid Based Complement Alternat Med 4: 279-285.
- Borgès Da Silva R, Contandriopoulos AP, Pineault R, Tousignant P (2011) A global approach to evaluation of health services utilization: concepts and measures. Healthc Policy 6: e106-e117.