Research Article - (2023) Volume 8, Issue 5
Impact of Software Change on Workflow and Satisfaction of Intensive Care Staff
Philippe Delrez1*,
Luc-Marie Jacquet1,
Jean-Louis Bachy1 and
Pierre-François Laterre2
1Department of ICU, Cliniques Universitaires Saint-Luc, Brussels, Belgium
2Department of ICU, Pole Hospitalier JOLIMONT, Belgium
*Correspondence:
Philippe Delrez,
Department of ICU, Cliniques Universitaires Saint-Luc, Brussels,
Belgium,
Email:
Received: 04-Oct-2023, Manuscript No. IPJHCC-23-18257;
Editor assigned: 06-Oct-2023, Pre QC No. IPJHCC-23-18257 (PQ);
Reviewed: 20-Oct-2023, QC No. IPJHCC-23-18257;
Revised: 25-Oct-2023, Manuscript No. IPJHCC-23-18257 (R);
Published:
01-Nov-2023, DOI: 10.36846/2472-1654-8.5.8048
Abstract
Background: The use of electronic patient record software at the bedside can have a significant impact on critical care practice and therefore potentially on workflow. Data recording is essential for good patient follow-up. We looked at the impact of a change in computer software in the critical care administrative workload and in the time spent at the bedside for patient care.
Methods: Qualitative prospective research in 2 ICU (58/18 beds) in 2 hospitals who worked with the same software. Hospital 1 changed the software in ICU to an EMR software and Hospital 2 did not modify his software. 10 months after the change of software, we evaluated the satisfaction of the ICU staff in the 2 institutions.
Results: Over 6-week period, 154 participants responded to a satisfaction questionnaire on the computerization of their respective ICU. In Hospital 1, the impact on general satisfaction and daily work of the medical nursing staff was 40.6% compared with 80.9% in Hospital 2 (p<0,0001).The time spent at the patient's bedside was 50% in Hospital 1 compare with 77% in Hospital 2 (p<0,0001). In Hospital 1, an additional time of 76.87 minutes over per shift of 8 hours compared Hospital 2 which did not change software. The software was adapted to ICU practice at 95.5% in Hospital 2. Only 17% of responders felt that saved administrative work with the new software in Hospital 1.
Conclusion: The change in software not specifically adapted to ICU practice results in more laborious coding 10 months after it implementation. It reduces the time spent for patient care and increases the administrative workload. Further studies with longer timeframes after implementation of a new system in other countries are needed to confirm our study on the impact of additional administrative workload for the nursing staff.
Keywords
Electronic health record; Digital strategy; Workload; Intensive care unit; Nursing
Introduction
Over the last decade, the healthcare system has been
severely challenged and hospital teams have faced exhausting
conditions, as highlighted by the recent Covid-19 pandemic.
Studies have demonstrated that a low nurse-to-patient ratio
is associated with high mortality, lack of care, and prolonged
ICU stays due to surgical complications [1-8]. Therefore, every
effort should be made to improve working conditions for
nursing staff.
As of today, few, if any, studies exploring the benefits of hospital
computerization, in particular when switching from paper to
computers, have evaluated software that was satisfactory
compared with new software considered to be better.
Nekoei-Moghadam et al., for instance, pointed out that the first
step to reduce medical errors was to improve patient safety
in healthcare organizations. Developing health information
systems, encouraging employees to report errors, and planning
to reduce nurses' workload can be effective in achieving the
desired health outcome [9].
It has also been proven that Electronic Nursing Handover Systems are more efficient than paper-based ones, and that
they ensure better care continuity [10,11]. However, systematic
and prospective studies identifying Electronic Health Record
(HER)-related errors across the entire medication management
process are scarce [12].
In 2016, the World Health Organization set the record straight
by stating several advantages of EHRs in the report of the
third global survey on eHealth, which was conducted by the
Global Observatory for eHealth [13]. EHRs improve the quality
[13,14], the accuracy, and the timeliness of patient information
at the place of care, and provide insights on healthcare costs,
use, and outcomes. EHRs also promote quality of care, reduce
costs, support patient mobility, increase information reliability,
and give access to patient information to multiple healthcare
providers [15]. Moreover, EHR data analyses can highlight
areas of concern and health service delivery [16].
Administrative procedures in medicine are obviously
increasing, which is extremely time-consuming for physicians
and nurses, increasing their respective workloads [17-19].
Thus, Mohammadnejad et al. underlined that technological
solutions should be considered on a contextual basis and
that attention should be paid when selecting technologies to
support nursing workload [20]. The nursing staff is well aware
that time devoted to patient care is essential in the therapeutic
process, hence their preference for the use of information
technology (IT) tools that can help them save time spent on
administrative processes and focus more on patient care, the
core activity of their profession [21].
The digitalization of intensive care units (ICUs) in our institutions
began in 1994 and has since been able to adapt to the reality
of the field, thus providing valuable medical decision-making
support (Artificial Intelligence [AI]) based on the needs of the
various players in the sector [22]. Therefore, we have gradually
witnessed a transition from paper patient files to a Patient Data
Management System (PDMS). The data recorded in a structured
manner enabled the ICUs to enter the world of big data and to
evolve towards advanced technologies that will be extended to
the rest of acute medicine (anesthesia, pediatric, neonatology,
and emergencies). The specifications for the latter were written
by Belgian intensive care physicians and nurses, who were
brought together in a working group on clinical informatics
and applied research in intensive care. By 1987, informatics
had enabled the development of comprehensive data storage
and processing programs, prognostic scores, improved clinical
research, and treatment adequacy. In 2019, the evolution of
the software used has been accredited by Accreditation Canada
International (ACI) [23,24].
The implementation of an EMR mobilizes enormously both
hospital management and political decision-makers. This
requires a lot of energy and requires considerable financial
budgets in a sometimes-complicated context in terms of health
policies. Reason why the subject can be considered sensitive.
The satisfaction survey presented in this article was meant to
be constructive, to strive for excellence in healthcare, and to
improve the quality of critical care in Europe and abroad. The
nursing staff is well aware of the complexity of hospital IT and
its necessity. Having a fully centralized electronic file format
accessible in one place is beneficial, provided that “IT is a tool
to help humans to care for humans. IT is malleable and must be
adapted as much as possible to the way of working and to the
needs of the user” [25].
Indeed, IT is there to support healthcare workers and facilitate
care evaluation [26]. In other parts of the world, Electronic
Medical Record (EMR)-type systems were shown to reduce
medical cost and improve healthcare quality and health
outcomes in general [10]. The largest potential savings from
health information technologies (HITs) come from a reduction
of hospitalization durations, nurses' administrative time, and
drug consumption in hospitals, as well as a reduction of drug
consumption and radiology equipment use in outpatient care
[17].
However, the complexity and variety of this often unstructured
information have contributed to the mistrust and gradual
rejection of IT tools and its formalized requirements, thus
underlining the need for a new organization regarding the
writing, coding, and hierarchy of medical information, as
pointed by A. De Wever [27]. The users will not like it and in case
it does not satisfy the needs, the users would ignore it, and they
even might consider the system an intruder and irritating factor
as pointed by S. Rostami [15]. Tool appropriation by healthcare
professionals is essential to ensure proper management of the
validity of each user's information.
Factors Associated with Nursing Time
The factors associated with working time are, according to two
Nursing Activities Score (NAS) studies in Belgium, body mass
index, length of stay outliers, Acute Physiology And Chronic
Health Evaluation (APACHE) II score, patients who died, as well
as patients undergoing mechanical ventilation and continuous
dialysis, as mentioned by Bruyneel et al in their article on
nursing workload measurement in intensive care with the NAS
[28,29].
Description of all Processes
The ICUs of both institutions have been equipped with the same
ICU-specific PDMS created by intensive care doctors and nurses
(GTICRASI), and running since 1994 with regular adjustments
(upgrading and updating). The ICU software used in both
institutions was known as Qcare PDMS (Group Evolucare-GPI).
One of the two institutions changed its software in November
2020 to an institutional EMR known as EPIC (also deployed
in the ICU). The objective of the study was to assess and
compare staff satisfaction in these two institutions regarding
the software used in intensive care. For the first institution
associated with the software change, we waited for 10 months
after the implementation of a new EMR to allow medical and
nursing staff to adapt for the new system before sending the
questionnaire to the two hospital staff members.
What are the expected benefits of an EMR like EPIC software
and the advantages of critical care software like Qcare PDMS?
The EMR software allows physicians, nurses, and healthcare
professionals to track healthcare information of their patients
[30]. It allows for greater accessibility (centralized information
updated immediately), efficiency, and security for both the
provider and the patient. It offers a better communication
between the different providers, a quick access to medical information (patient medical history, allergies), coordination
of care, a digital record of a patient's health information, and
decision-making support. EMR software helps reduce medical
errors (drug interactions, prescription errors, etc.) [16].
At the critical care level, the Qcare PDMS software, which is
specific to critical care such as intensive care, anesthesia,
emergency room, and neonatology, will provide, in addition to
the aforementioned elements, granularity in the precision of the
digital recording of structured information, rapid information
visualization, precision and quality of the hydroelectrolytic
balance, simplicity of use, adaptability and scalability of the
software according to the pharmacological, practical, or
ministerial modifications. Moreover, it is user-friendly unique
multilingual software. Since the structured digital information
reported at the patient's bedside is of high quality, the data
can easily be extracted for scientific studies involving artificial
intelligence.
Aim of the Study
We assessed the satisfaction of heterogenous ICU staff group
in two hospitals 25 years after the beginning of this adventure
[31]. We sought to answer the following research question:
Does changing software in an ICU impact nursing clinical
workload, time devoted to patient care, and satisfaction?
Methods
Design and Setting of the Study
This is qualitative study was conducted in two hospitals including 7 intensive care units, with a total of 76 mixed intensive care beds (surgical and medical). The two institutions employed 255 intensive care professionals and received all types of pathologies. Regarding the sample size calculation, the total number of healthcare professionals in the nursing staff of the two teams was lower than the theoretical number needed to meet the optimal statistical sample size.
The study was performed between two COVID-19 waves and outside the workload registration period requested by the Belgian Ministry of Health, which requires a specific coding of nursing procedures that is used as a tool to fund hospitals and critical care [32].
Survey
A questionnaire was developed to assess the satisfaction of ICU staff and the impact of IT tools on their daily work. The items of the questionnaire were based on an analysis of a similar survey, on other questionnaires included in the complementary training courses, and on the institution's own “homemade” format. A pre-test was carried out to validate the questionnaire.
This satisfaction survey on the computerization of intensive care included a four-page questionnaire with 20 questions in paper format (to ensure anonymity) (Annexure).
The main themes of the questionnaire were classified into several dimensions:
• User profile and experience duration
• Numerical evaluation of the satisfaction regarding the IT tool and its quality
• IT tool impact on daily work
• IT tool functions needing improvement or working well.
One or more answers were allowed depending on the type of question and participants could also add free hand-written comments. The most relevant questions are presented in the results section and the answers to the other questions can be found in the Table 1.
Statistical Analysis
The encoding was carried out electronically using the Survey Manager V7 software from Soft Concept. For satisfaction scoring and all questions, a Chi-square test was used. A p-value value <0.05 was considered statistically significant. To calculate the minimum sample size, we used the Cochran's equation with a precision level of 5%, a confidence level of 95%, an estimated proportion of 0.5 and a population size of 255. The appropriate sample size given the population size and specified combination of precision, confidence and variability was 154.
Ethical Considerations
A unique and anonymous number was randomly assigned to each questionnaire completed by the healthcare teams in each institution. We have respected the law on privacy and the subjects' anonymity was assured. The agreement of the department heads was sought and granted. No nonanonymized data were included in the study. The study was submitted to the Ethical Commission of the Hospital for approval. As no data collected in our study had an impact on privacy, no consent was required.
Results
Data were collected between September 20, 2021 and
October 31, 2021. Out of the 255 critical care professionals,
154 questionnaires were fully answered and analyzed. The
participation rate in the study was 56% for Hospital #1 (a
tertiary care hospital with a larger staff) equipped with the
new EMR EPIC and 75% for Hospital #2 (a general hospital)
equipped with Qcare PDMS, a specific ICU software.
Characteristics of the Participants
The study included 154 participants, 109 from Hospital #1
(computerized with EMR EPIC) and 45 from Hospital #2
(computerized with Qcare PDMS). The mean age of the
responders was 39.3 years (interquartile range: 22-64) with
a higher proportion of women than men. The education
degree was higher in Hospital #1, with a higher proportion of
respondents with a university level than in Hospital #2. The
confirmed professional field experience was over 10 years in
both institutions (Table 1).
The satisfaction results were analyzed according to age groups:
20 years-35 years old, 36 years-50 years old, and >50 years
old. The satisfaction level did not differ according to age, with
an average score per group of 5.2/10, 5.6/10, and 5.3/10,
respectively.
Table 1: Characteristics of the heterogenous participants. EMR, electronic medical record; ICU, Intensive Care Unit
| Total n=154 |
Total n=154 |
Hospital #1 |
Hospital #2 |
| EMR software |
ICU software |
| (n=109) |
(n=45) |
| Gender: Male/Female |
29%/72% |
33 males/73 females/3 unknown |
10 males/35 females |
| Age: Average |
39.3 years |
38 years |
42.5 years |
| Youngest/Oldest |
22 years/64 years |
22 years/64 years |
23 years/59 years |
| Maximum educational level |
| Primary school |
- |
- |
- |
| Lower secondary school |
- |
- |
- |
| Higher secondary school |
8 (5%) |
5 |
3 |
| Non-university higher studies |
96 (63%) |
63 |
33 |
| Academic studies |
48 (32%) |
40 |
8 |
| What is your profession in the intensive care unit? |
| Healthcare assistant |
|
4 |
4 |
| Nurse |
83 |
32 |
| Physiotherapist |
3 |
2 |
| Doctor |
16 |
4 |
| Technical staff |
1 |
1 |
| Secretary |
- |
2 |
| Dietician |
- |
- |
| Other |
- |
- |
| How many years have you been working in intensive care? |
| <1 year |
17 |
14 |
3 |
| 1-3 years |
15 |
11 |
4 |
| 3-5 years |
18 |
15 |
3 |
| 5-10 years |
20 |
15 |
5 |
| 10-15 years |
17 |
13 |
4 |
| 15-20 years |
16 |
9 |
7 |
| 20 years |
50 |
31 |
19 |
| No response |
1 |
1 |
- |
| Participation rate in the study |
|
56% |
75% |
Satisfaction Score
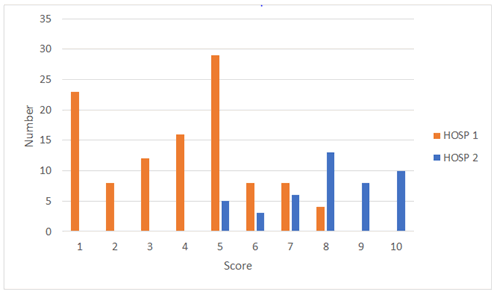
Figure 1 shows the extent to which the IT tools ease the
administrative tasks, according to participants. The mean
satisfaction score was 3.89 in Hospital #1 compared with 8.02
in Hospital #2 (p<0.0001). The score obtained in Hospital #2
would have probably been equivalent to that of Hospital #1
before the software change (or even higher), as some additional
functionalities existed and others had been programmed. This
could explain some of the dissatisfaction expressed by the staff.
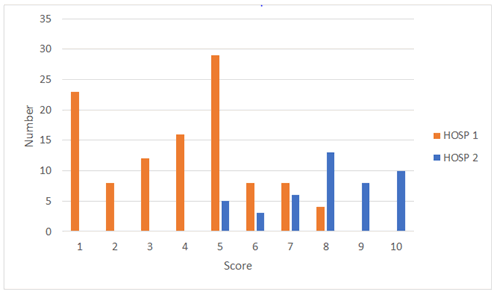
Figure 1: Assessment of the extent to which the information technology
tools ease the administrative tasks, as rated on a scale from 0 to 10
by participants. Hospital #1 was equipped with the EMR software and
Hospital #2 was equipped with the QCare PDMS software, specific to
ICUs
Evaluation of IT Tool Quality
Assessment of the IT tool quality was 30.5% for Hospital #1
vs. 54.5% for Hospital #2 (p<0.0001). Regarding the item
“insufficiently advanced for my position,” we obtained 20.5%
for Hospital #1 vs. 2.25% for Hospital #2 (p<0.0001). For the
item “just right for position,” we obtained 16.5% for Hospital
#1 vs. 41% for Hospital #2 (p<0.0001). For the item “not very
advanced for my position,” we obtained 12.5% for Hospital #1
vs. 2.25% for Hospital #2 (p<0.0001) (Table 2).
Table 2: Evaluation of IT tool quality. EMR, electronic medical record; ICU, Intensive Care Unit
| Functionalities |
Hospital #1 |
Hospital #2 |
| EMR software |
ICU software |
| No change at all for my position |
12 (11.5%) |
- |
| Quite advanced for my position |
31 (30.5%) |
24 (54.5%) |
| Insufficiently advanced for my position |
21 (20.5%) |
1 (2.25%) |
| Just right for my position |
17 (16.5%) |
18 (41%) |
| Not very advanced for my position |
13 (12.5%) |
1 (2.25%) |
| Too advanced for my position |
9 (8.5%) |
- |
| No answer |
6 |
1 |
IT Description
For the description of the IT tools, in Hospital #1 using the
EMR Epic, 41% of the respondents estimated that there was a
work overload and 24% that the tool was less advanced than in
the past, compared with 0% in Hospital #2 using Qcare PDMS.
In Hospital #2, 79% expressed that it was a precious help in
everyday life compared with 26% in Hospital #1. 6% of the
participants considered that it was impossible to work without
an IT tool in Hospital #1 (Table 3).
Table 3: Description of the IT tool
| Several choices are possible |
Total |
Hospital #1 |
Hospital #2 |
| n=154 |
EMR software (n=109) |
ICU software (n=45) |
| It is an overload of work |
52 |
52 (41%) |
- |
| The tool is less advanced than in the past |
30 |
30 (24%) |
No software change |
| This does not change anything |
6 |
5 (4%) |
1 (2%) |
| It is a precious help in everyday life |
70 |
33 (26%) |
37 (79%) |
| I could not work without it |
16 |
7 (6%) |
9 (10%) |
Ratio of Time Spent for Patient Care to Computer
Tasks
Table 4 shows the proportion of time devoted to patient care
vs. time spent working on the computer. In Hospital #1, 56% of
the nursing staff expressed that the time spent on the computer
was equivalent to the time devoted to patient care. By contrast,
in Hospital #2, 76% considered that the time devoted to patient
care represented three quarter of their time shift.
Time Saved for Patient Care
In Hospital #1, an average of 93.75 minutes was saved daily
for patient care as opposed to 237.12 minutes in Hospital #2
(Table 5).
Satisfaction Regarding IT Tools
Concerning the satisfaction regarding the IT tools on a scale
from 1 to 10, the mean score was 4.06 in Hospital #1, equipped
with the EMR software, and 8.09 in Hospital #2, equipped with
the ICU software (p<0.0001) (Table 6).
Table 4: Ratio of time spent for patient care to computer tasks. EMR, electronic medical record; ICU, intensive care unit
| Ratio |
Total n=154 |
Hospital #1 |
Hospital #2 |
| EMR software |
ICU software |
| (n=109) |
(n=45) |
| 50% patients/50% computer |
66 |
61 (56%) |
5 (11%) |
| if >50 % computer |
16 |
15 (14%) |
0 |
| 40% patients/60% computer |
- |
5 |
- |
| 25% patients/75% computer |
7 |
| 20% patients/80% computer |
3 |
| 60% patients/40% computer |
|
1 (1%) |
0 |
| 75% patients/25% computer |
33 |
21 (19%) |
12 (27%) |
| 80% patients/20% computer |
13 |
2 (2%) |
11 (25%) |
| 90% patients/10% computer |
11 |
4 (3.5%) |
7 (15%) |
| 95% patients/5% computer |
4 |
0 |
4 (9%) |
| No answer |
11 |
5 (4.5%) |
6 (13%) |
Table 5: Time saved for patient care. EMR, electronic medical record; ICU, Intensive Care Unit
| |
Total n=154 |
Hospital #1 |
Hospital #2 |
| EMR software |
ICU software |
| (n=109) |
(n=45) |
| Time saved for patient care per shift (8h) |
60 |
19 (17%) |
41 (91%) (p<0.0001) |
| Time saved during 8-hour shifts (minutes) |
|
31.25 minutes |
79.04 minutes |
| (12 answers/19) |
 (21 answers/41) |
| (From 10 to 60 minutes) |
(From 15 to 120 minutes) |
| Time saved daily |
|
93.75 minutes |
237.12 minutes |
| Time lost for administrative work per shift (8h) |
90 |
88/109 |
2/45 (p<0.0001) |
| Time lost during 8-hour shifts (minutes) |
|
76.87 minutes |
No answer |
| Â (47 answers/88) |
| (From 15 to 400 min) |
| Time lost daily |
|
230.61 minutes |
Not applicable |
| Lost time for administrative work-Saved time for patient care |
|
230.61-93.75=136.86 minutes per day |
Not applicable |
| No answer |
4 |
2 (2%) |
2 (4.5%) |
Table 6: Satisfaction assessment regarding the IT tools used in both hospitals
| Score |
Hospital #1 |
Hospital #2 |
| EMR software |
ICU software |
| (n=109) |
(n=45) |
| 1 |
1 |
0 |
| 2 |
9 |
0 |
| 3 |
17 |
1 |
| 4 |
23 |
0 |
| 5 |
13 |
3 |
| 6 |
15 |
1 |
| 7 |
9 |
9 |
| 8 |
11 |
12 |
| 9 |
6 |
9 |
| 10 |
1 |
10 |
| Mean |
4.066 |
8.089 |
Discussion
This study shows that the software change in one of the
institutions had a significant impact on the administrative
workload of nursing staff and reduced the time devoted
to patient care. Other studies [33,34] have shown that
implementing an IT system as opposed to handwritten
documentation has reduced the time devoted to administrative
work and increased the time spent at the patient bedside,
as nursing work documentation was handwritten. However,
we can see that administrative procedures in medicine are
increasing. They are highly time-consuming for physicians and
nurses, with a major impact on patient care. As mentioned
by the British Medical Association, doctors in England spend
more than 13.5 million hours each year due to inadequacies
and malfunctions in IT systems and equipment, equivalent to
nearly 8,000 full-time medical jobs or just under £ 1 billion
[2]. As previously mentioned, other studies explored in detail
the quality of data collection and error reduction, but few
reported data on nursing satisfaction and time spent working
on computers. By contrast, they presented a lot of data on
satisfaction regarding the switch from paper to IT tools, but
did not explore the impact of a new IT system on the nursing
satisfaction and time spent on the computer compared with
the time devoted to patient care.
IT tools can improve or reduce the administrative workload
if they are adapted to the specific condition of the ICU. The
most important aspect is to have a computer system adapted
to the field, especially in the ICU, emergency department,
or anesthesia department. The requirements include a userfriendly
computer system fully connected to record clinical
data and prescription data. Some programs are more adapted
for outpatient services, consultation, and general services, as
the information list is more restricted.
Evaluating the implementation of software is not an easy task
due to the complexity of the criteria. However, we believe
that a period of 10 months after the launch of new software
was sufficient to use it optimally. Of note, hospital staffs are
very mobile during their clinical training and hospitals are
increasingly working with temporary staff, which leaves little
time for training and the acquisition of IT subtleties.
When analyzing the socio-demographic characteristics of the
participants, we observed that the education level in intensive
care was very high. The proportion of participants with a
university level was higher in Hospital #1 than in Hospital #2,
which is expected as Hospital 1 was academic.
The staff of Hospital #1 was very well trained, and a quarter of
the intensive care nurses had a university degree in addition to
their specialization in intensive care. In terms of field practice,
more than 50% of the ICU staff had at least 10 years of clinical
experience. It can be concluded that medical informatics
requirements were very high. For both hospitals, the analysis
of the average satisfaction level according to age led to the
conclusion that younger staff, more used to computer systems,
did not show a different satisfaction level with the new system.
The participation rate was high, which highlights an interest
from healthcare professionals in the issues affecting their daily
work. The key observation was the major satisfaction difference
between the two hospitals.
A third of the responders in Hospital #1 found the tool fairly
advanced for their position and less than a fifth found it fully
adapted to the needs of the field. These figures almost doubled
in Hospital #2.
Since Hospital #2 has not undergone any change in the
computerized patient file system, this former question was not
applicable. It can also be observed that the respondents who
rated the software as an overload of work are all in Hospital #1.
This additional workload can be explained by a data encoding
process that is more laborious 10 months after the launch than
with the previous software, which was adapted to care practice
and could effortless be used at the patient's bedside thanks to
its easily accessible configuration. Similar remarks were found
in the literature in England in 2014, in Denmark in 2019, and in
Switzerland in 2020 [35-37].
Various elements could explain the loss of time devoted to
patient care, but they were not explored in our study. The
administrative workload may induce some under-coding of
information and data, and may have an impact on hospital
financing if it is based on the objective critical care workload
[29]. This dimension was not explored by our questionnaire,
but further studies should address this point. Knowing that the
staffing standard for an ICU is 2.5 full-time equivalents per bed
(FTEB), the daily nursing time spent on administrative tasks
would correspond to 0.28 FTEB [28].
Limitations of the Study
This study was performed in only two institutions and 7 ICUs.
The number of participants was limited. The questionnaire
was based on the institution's own “homemade” format and
was not a scientifically validated standard questionnaire. The
qualitative approach of the questionnaire could be combined
with more objectives and defined criteria to obtain greater
significance of the results through a mixed method approach.
Moreover, the study should be repeated after a more
prolonged adaptation period (for example 6 months and 12
months) to reevaluate the satisfaction of nursing and medical
staff regarding the software and have a comparison with the
target groups. The strength of this study is that we looked at the impact of a software change in the ICU and not a switch
from paper to electronic format. Strength is that we were able
to compare the ratings of the same employees who worked at
the patient bedside with both software (Table 7).
Table 7: Summary table
| Summary table |
Hospital #1 |
Hospital #2 |
| IT satisfaction in intensive care |
Software EMR |
Software ICU |
| Number of participants N=154 |
109 |
45 |
| Software adapted to the care practice |
47% |
95.5% |
| Proportion of paper/computer work (PC) |
13%pap/87% PC |
25%pap/75% PC |
| IT is overworked and less advanced than in the past |
65% |
0% |
| Valuable help/difficult to do without |
32% |
89% |
| Time spent with the patient |
50% |
77% |
| Estimated loss of time |
82% |
2,5% |
| Average: Min/shift/person |
76,87 min |
-min |
| Estimated time saving |
17,43% |
95% |
| average: Min/shift/person |
-min |
79,04 min |
| General level of satisfaction |
40.66% |
80.89% |
Conclusion
The volume of information produced in hospitals is quite
considerable, hence the importance of having correct and
precise data recording corresponding to the reality on the
ground. The change from one software to another had a major
impact on the time devoted to patient care by the nursing
and medical staff, as part of patient care time may turn into
administrative work time.
In intensive care, the software used must be specific to the
discipline and easily adapted according to the needs and the
evolution of the ICU field practice.
Before any change from software to another, the ICU
specificities must be considered by the decision-making teams.
This way, the medical and nursing staff will be able to continue
to correctly enter as much data as possible in a structured way
and in a minimum of time. It will be essential to assess staff
satisfaction on several occasions. This will enable all levels of
management to improve the quality of care and the financing
of healthcare institutions. The main objective of healthcare
computerization must remain “to help people to care for
people” in a simple, fast, and efficient way…
Availability of Data and Materials
The data are available from the corresponding author on
simple request.
Acknowledgement
The authors would like to highlight the contributions of the
GTICRASI and emphasize the vital importance of including
users in the design and development of an effective IT tool.
However, users must be able and willing to spend time with IT
specialists to define their needs.
Competing Interests Statement
The authors declare that they have no known competing
financial interests or personal relationships that might appear
to influence the work reported in this article. Ph. DELREZ
declares to have a complementary independent activity to give
trainings and consultations.
Funding Statement
No funding was received to assist with the preparation of this
manuscript.
Declaration Of Generative AI In Scientific Writing
During the preparation of this work the authors not used
generative AI in scientific writing. The authors reviewed and
edited the content and takes full responsibility for the content
of the publication.
References
- West E, Mays N, Rafferty AM, Rowan K, Sanderson C (2009) Nursing resources and patient outcomes in intensive care: A systematic review of the literature. Int J Nurs Stud. 46(7):993-1011.
[Crossref] [Google Scholar]
- Aiken LH, Sloane DM, Bruyneel L, Van Den Heede K, Griffiths P, et al. (2014) Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet. 383(9931):1824-30.
[Crossref] [Google Scholar]
- Cho SH, Yun SC (2009) Bed-to-nurse ratios, provision of basic nursing care, and in-hospital and 30-day mortality among acute stroke patients admitted to an intensive care unit: Cross-sectional analysis of survey and administrative data. Int J Nurs Stud. 46(8):1092-101.
[Crossref] [Google Scholar]
- Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ (2007) The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Med Care. 45(12):1195-1204.
[Crossref] [Google Scholar]
- West E, Barron DN, Harrison D, Rafferty AM, Rowan K, Sanderson C (2014) Nurse staffing, medical staffing and mortality in intensive care: An observational study. Int J Nurs Stud. 51(5):781-94.
[Crossref] [Google Scholar]
- Neuraz A, Guérin C, Payet C, Polazzi S, Aubrun F, et al. (2015) Patient mortality is associated with staff resources and workload in the ICU: A multicenter observational study*. Crit Care Med. 43(8):1587-1594.
[Crossref] [Google Scholar]
- Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, et al. (2018) Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. Int J Nurs Stud. 78:10-15.
[Crossref] [Google Scholar]
- Dang D, Johantgen ME, Pronovost PJ, Jenckes MW, Bass EB (2002) Postoperative complications: Does intensive care unit staff nursing make a difference? Heart Lung. 31(3):219-228.
[Crossref] [Google Scholar]
- Nekoei-Moghadam M, Raadabadi M, Heidarijamebozorgi M (2020) Patient safety culture in university hospital's emergency departments: A case study. Int J Health Plann Manage. 35(4):852-858.
[Crossref] [Google Scholar]
- Coughlan JJ, Mross T, Gul F, Abbott A, Say R, et al. (2018) Implementing an electronic clinical handover system in a university teaching hospital. Ir J Med Sci. 187(2):309-312.
[Crossref] [Google Scholar]
- Saraswasta IWG, Hariyati RTS, Yetti K, Nuraini T (2021) Implementation of effective nurse communication in hospital through Electronic Nursing Documentation (END). Indian J Public Health Res Dev. 12(1):294-299.
[Google Scholar]
- Walsh KE, Adams WG, Bauchner H, Vinci RJ, Chessare JB, et al. (2006) Medication errors related to computerized order entry for children. Pediatrics. 118(5):1872-1879.
[Crossref] [Google Scholar]
- World Health Organization (2016) Global diffusion of eHealth: Making universal health coverage achievable: Report of the third global survey on eHealth.
- Uslu A, Stausberg J (2021) Value of the electronic medical record for hospital care: Update from the literature. J Med Internet Res. 23(12):e26323.
[Crossref] [Google Scholar]
- Rostami S, Sarmad A, Mohammadi M, Cheleie M, Amiri S, et al. (2015) Evaluating hospital information systems from the point of view of the medical records section users in medical-educational hospitals of Kermanshah 2014. J Med Life. 8:232-240.
[Crossref] [Google Scholar]
- Malliarou M (2009) Advantages of information systems in health services. Choregia. 5:8-10.
[Google Scholar]
- Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, et al. (2005) Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 24(5):1103-1117.
[Crossref] [Google Scholar]
- British Medical Association (2022) Building the future: Healthcare infrastructure reports Digital infrastructure
- Wallace S (2021) What's next blog.
- Mohammadnejad F, Freeman S, Klassen-Ross T, Hemingway D, Banner D (2023) Impacts of technology use on the workload of registered nurses: A scoping review. J Rehabil Assist Technol Eng. 10:20556683231180189.
[Crossref] [Google Scholar]
- Lee TT, Yeh CH, Ho LH (2022) Application of a computerized nursing care plan system in one hospital: Experiences of ICU nurses in Taiwan. J Adv Nurs. 39(1):61-67.
[Crossref] [Google Scholar]
- Hashimoto DA, Witkowski E, Gao L, Meireles O, Rosman G (2020) Artificial intelligence in Anesthesiology: Current techniques, clinical applications, and limitations. Anesthesiology. 132(2):379-394.
[Crossref] [Google Scholar]
- Hanique G (2003) SAPI: Score of activities and pathologies in intensive care or integrate intensive function in hospital function.
- Accreditation Canada (2023) Internationally Accredited Organizations.
- Torki A (2022) Impact of the Patient Information Patient Record on the quality of care, the experience of a hospital in Luxembourg. Proj Proyéctica Proj. pp:57-79.
[Crossref] [Google Scholar]
- Naveed M, Al-Serkal Y, Al-Nuaimi S, Al-Blooshi K, Majed Al-Mahiri N, et al. (2019) Improved efficiency and patient safety through bespoke electronic thalassaemia care module. BMJ Health Care Inform. 26(1):e100094.
[Crossref] [Google Scholar]
- De Wever A (2017) Does computer science improve the functioning of the hospital? Le Journal Du Medecin-FR.
- Bruyneel A, Tack J, Droguet M, Maes J, Wittebole X, et al. (2019) Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): A prospective study in 16 hospitals in Belgium. J Crit Care. 54:205-11.
[Crossref] [Google Scholar]
- Bruyneel A, Gallani MC, Tack J, d'Hondt A, Canipel S, et al. (2021) Impact of COVID-19 on nursing time in intensive care units in Belgium. Intensive Crit Care Nurs. 62:102967.
[Crossref] [Google Scholar]
- Alpert JS (2016) The electronic medical record in 2016: Advantages and disadvantages. Digit Med. 2(2):48.
[Google Scholar]
- Delrez P, Hantson P, Jaquet LM, Laterre PF (2021) Computerization of intensive care from Bic to Click: A look back over 25 years of experience.
- Sermeus W, Van den Heede K, Michiels D, Van Herck P, Delesie L, et al. (2006) Revision of the Belgian nursing minimum dataset: From data to information. Stud Health Technol Inform. 122:616-618.
[Crossref] [Google Scholar]
- Lin SC, Jha AK, Adler-Milstein J (2018) Electronic health records associated with lower hospital mortality after systems have time to mature. Health Aff Proj Hope. 37(7):1128-1135.
[Crossref] [Google Scholar]
- Torki A (2022) Impact of the electronic health record on the quality of care: Electronic health record, quality, Luxembourg, digital strategy. Proj Proy Proj. 17(HS):57-79.
[Google Scholar]
- Hertzum M, Ellingsen G (2019) The implementation of an electronic health record: Comparing preparations for Epic in Norway with experiences from the UK and Denmark. Int J Med Inf. 129:312-317.
[Crossref] [Google Scholar]
- Allen A (2019) Lost in translation: Epic goes to Denmark. POLITICO.
- Meier C (2020) New computer system has brought the barrel over.
Citation: Delrez P, Luc-Marie J, Bachy JL, Laterre PF (2023) Impact of Software Change on Workflow and Satisfaction of Intensive Care Staff. J Healthc Commun. 8:8048.
Copyright: © 2023 Delrez P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.