Keywords
COVID-19; Femoral line; Ugular line; Infection prevention and control.
Introduction
Patients admitted in critical units are more vulnerable to get hospital acquired infections, particularly device associated blood stream infections. The current rapidly rising pandemic scenario due to the SARS COVID-19 infection is known to cause acute respiratory distress syndrome (ARDS). Severely ill patients required invasive device like central line. Airborne transmission is a common method of the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and exhalation by infected people or carriers can easily expose healthy people to coronavirus disease 2019 (COVID-19) [1]. According to a report by the World Health Organization, the possibility of transmitting the virus through air during some procedures that generate aerosols, such as endotracheal intubation and bronchoscopy, is higher [2].
Femoral, jugular, and subclavian venous catheterizations are routinely performed during critically ill patient care. These invasive procedures contribute to additional morbidity, mortality, and costs derived from the interactions between mechanical, infectious, and thrombotic complications [3,4] Femoral venous catheterizations, which is rapid to perform, is considered an emergency procedure to gain vascular access, but which should be avoided to limit nosocomial complication [5-8].
Some studies reported a higher incidence of complications associated with femoral vs jugular catheterizations while other studies reported lower or similar incidences with femoral catheterizations [9,10].
Central venous catheterization is one of the most commonly performed procedures in intensive care units. Wearing personal protective equipment (PPE) for placing central venous catheter can make the procedure challenging because of poor visibility. Insertion of central venous catheter becomes even more difficult when the patient is in respiratory distress and is unable to lie flat on the bed. All these increase chances of error and complication rate. Most common route of central venous access is through internal jugular or subclavian veins but slight mistake can lead to grave complications like pneumothorax or haemothorax which are unacceptable in these group of patients [11].
Femoral venous catheterization, which is rapid to perform, is considered an emergency procedure to gain vascular access, but which should be avoided to limit nosocomial complications [12- 14]. Here by we aim to evaluate the rate of infection in femoral and jugular lines in the COVID-19 patients.
Material and Methods
Study setting and design
We conducted a retrospective chart review of adult patients admitted in the COVID unit of Indus hospital, Korangi campus, Karachi with laboratory-confirmed COVID-19 cases. Aged >18 years were seen from 1 August 2020 to 31 October 2020.
Participants
All patients >18, with evidence of SARS-CoV-2 infection by a polymerase chain reaction in nasal swabs, were included. Adult patients from HDU and ICU were included. Admitted patients were monitored for the rate of infections in their line of insertion i-e femoral or jugular. Patient’s data was retrieved from the electronic medical record (EMR) and documented on specifically designed case report forms (CRFs).
Statistical Analysis
SPSS version 20 was used to calculate the frequency of qualitative variable, i.e., gender, site of line insertion, organism and ward. The mean, median, standard deviation, Interquartile range and confidence interval were calculated for quantitative variables, such as age. Chi-square test was applied to compare differences between categorical variables. P-value <0.05 was considered as significant.
Operational definition
HDU: A high-dependency unit is an area in a hospital, usually located close to the intensive care unit, where patients can be cared for more extensively than on a normal ward, but not to the point of intensive care.
ICU: An intensive care unit, also known as an intensive therapy unit or intensive treatment unit or critical care unit, is a special department of a hospital or health care facility that provides intensive care medicine.
Results
Total 37 patients were observed with the mean age was 59.84 ± 16.2, median 61 (21-84) and Interquartile rage 24. Males were 25/37 (67.6%) while females were 12/37 (32.45). Majority of the patients were admitted in ICU 28/37 (75.7%) while 9/37 (24.3%) were admitted in HDU.
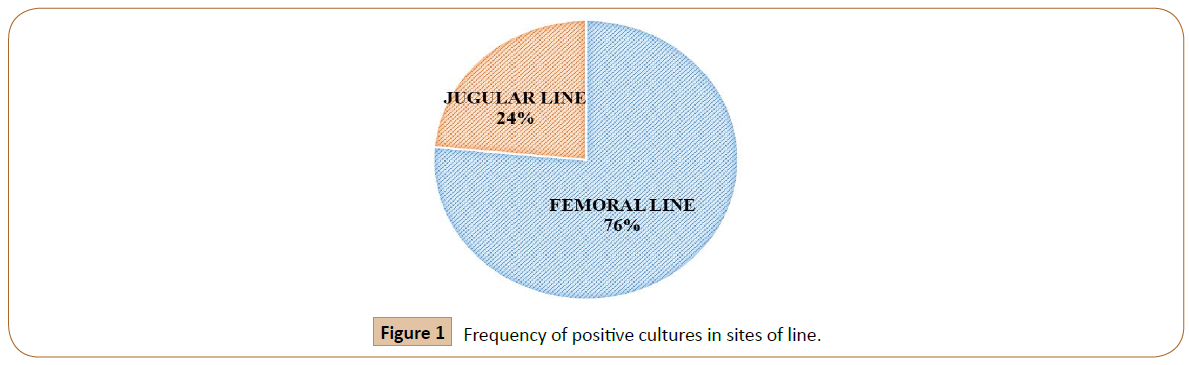
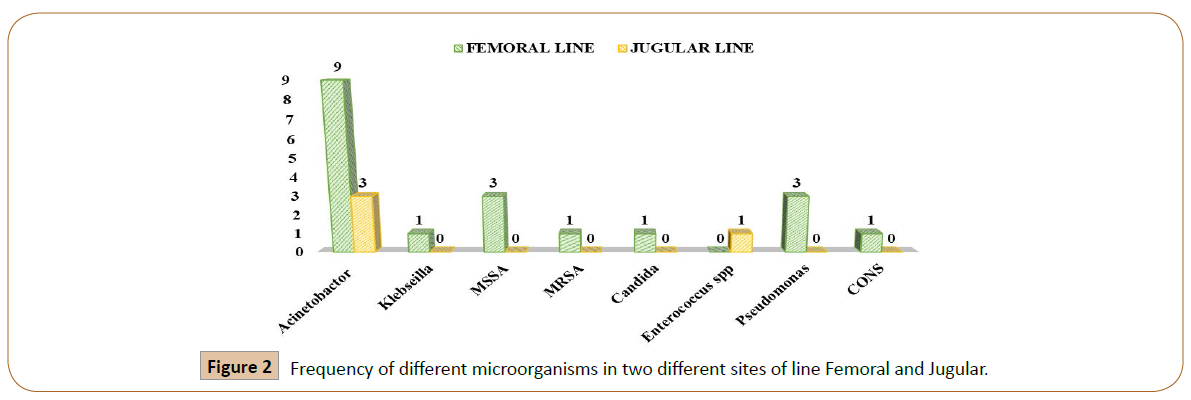
Femoral line was place in 29/37 (78.4%) patients while jugular line was place in 8/37 (21.6%). We have observed the total 17/37 (45.9%) positive culture in our study patients. In these 17 patients 13/17 (76.4%) femoral lines were positive for cultures, while 4/17 (24%) jugular lines were positive for the cultures (Figure 1). In 13 femoral lines, total 19 organisms were found out of which Gram positive bacteria (GPB) were 4/19 (21%), Gram negative bacteria (GNB) 13/19 (69%) while Coagulasenegative staphylococci (CoNS) 1(5%) and Candida albicans 1(5%). In 4 jugular line, total 4 organisms were observed 3 (75%) were GNB and 1(25%) were GPB. The frequency of different microorganisms in two different sites of line insertion were shown in Figure 2.
Figure 1: Frequency of positive cultures in sites of line.
Figure 2: Frequency of different microorganisms in two different sites of line Femoral and Jugular.
Discussion
In this study, we found the less number of infections in the patients that were inserted the jugular line as compare to the femoral line these results are not similar to the study done by Parienti JJ who didn’t detect any clinically relevant benefit of the jugular site catheterization compared with femoral site catheterization for reducing the risk of nosocomial complications in critically ill adults requiring venous access. This result is inconsistent with the widely accepted convention to avoid femoral catheterization to prevent the risk of catheter-related infection [15].
According to Centers for diseases control and prevention CDC guidelines for the Prevention of Intravascular Catheter-Related Infections (2011); that in adults, use of the radial, brachial or dorsalis pedis sites is preferred over the femoral or axillary sites of insertion to reduce the risk of infection [16,17].
Recently an article published laid down a catheter embedding protocol to prevent doctors and nurses from working in COVID-19 wards during central vein catheterization [18]. They decided to utilize the triple-lumen peripherally inserted central catheters as the preferred means of establishing central vein access. Their findings indicated low staff exposure, similar to our findings. Therefore, personal protection equipment is vital for preventing the infection during jugular catheterization. However, in case full protection is impossible, the jugular catheter can be replaced with the femoral catheter to protect the performing surgeons.
The femoral central line is not routinely used in adults mainly due to fear of high risk of catheter related bloodstream infection (CRBSI). There is no conclusive evidence to suggest that femoral access has more risk for CRBSI [19]. But there is one case study in which they successfully inserted an ultrasound guided femoral central line 5cm below the inguinal ligament in a view to further reduce catheter induced infection rate. It has been suggested that the risk of infection will be very much reduced if we use full barrier precaution, ultrasound guidance, low approach, tunneling and medicated catheter. Another advantage of low approach femoral access is that as person doing this procedure is away from the respiratory passage of the patient it may reduce chances of airborne infection during COVID-19 pandemic [20,21].
In conclusion, the COVID-19 pandemic will undoubtedly change many of our clinical behaviors in the future. We hope that in the field of venous accesses, the positive side effect of this experience can take the form of a new awareness of the need to save resources and increase safety even outside of health emergency situations.
References
- WHO Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief.
- WHO (2019) Report of the WHO-China Joint Mission on Coronavirus disease.
- Mermel LA (2000) Prevention of intravascular catheter-related infections. Intern Med 133: 5.
- McGee DC, Gould MK (2003) Preventing complications of central venous catheterization. N Engl J Med 348: 1123-33.
- Timsit J (2003) What is the best site for central venous catheter insertion in critically ill patients. Crit Care 7: 397-9.
- Canaud B, Formet C, Raynal N (2004) Vascular access for extracorporeal renal replacement therapy in the intensive care unit. Contrib Nephrol 144: 291-307.
- Pronovost P, Needham D, Berenholtz S (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355: 2725-32
- Oliver MJ, Callery SM, Thorpe KE, Schwab SJ, Churchill DN (2000) Risk of bacteremia from temporary hemodialysis catheters by site of insertion and duration of use: a prospective study. Kidney Int 58: 2543-45.
- Lorente L, Henry C, Martin MM, Jimenez A, Mora ML (2005) Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care 9: R631-R635.
- Deshpande KS, Hatem C, Ulrich HL (2005) The incidence of infectious complications of central venous catheters at the subclavian, internal jugular, and femoral sites in an intensive care unit population. Crit Care Med 33: 13-20.
- Alan SG, Caroline O, Ken T, Susanna L, Dana AV (2007) Braner Central Venous Catheterization. N Engl J Med 24: 356: e21.
- Timsit JF (2003) What is the best site for central venous catheter insertion in critically ill patients. Crit Care 7: 397-9.
- Canaud B, Formet C, Raynal N (2004) Vascular access for extracorporeal renal replacement therapy in the intensive care unit. Contrib Nephrol 144: 291-307.
- Pronovost P, Needham D, Berenholtz S (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355: 2725-32.
- Parienti JJ, Thirion M, Megarbane B (2008) Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial. JAMA 299: 2413-22.
- Martin C, Saux P, Papazian L, Gouin F (2001) Long-term arterial cannulation in ICU patients using the radial artery or dorsalis pedis artery. Chest 119: 901-6.
- Koh DB, Gowardman JR, Rickard CM, Robertson IK, Brown A (2008) Prospective study of peripheral arterial catheter infection and comparison with concurrently sited central venous catheters. Crit Care Med 36: 397-402.
- Jasinski PT, Tzavellas G, Rubano JA, Rutigliano DN, Skripochnik E, et al. (2019) A protocol for central ve¬nous access in patients with corona¬virus disease (COVID-19). J Vasc Surg.
- Arvaniti K, Lathyris D, Blot S, Apostolidou-Kiouti F, Koulenti D (2017) Cumulative Evidence of Randomized Controlled and Observational Studies on Catheter- Related Infection Risk of Central Venous Catheter Insertion Site in ICU Patients: A Pairwise and Network Meta-Analysis. Crit Care Med 45: e437-e448.
- Pittiruti M, Pinelli F, GAVeCeLT (2020) Working Group for Vascular Access in COVID-19. Recommendations for the use of vascular access in the COVID-19 patients: An Italian perspective. Crit Care 24: 269.
- Ilonzo N, Rao A, Soundararajan K, Vouyouka A, Han D (2020) The importance of a centralized line service during the COVID-19 pandemic. J Vasc Surg 72: 403-404.