Keywords
HIV; HAART; Anemia; Thrombocytopenia;
Neutropenia; Eosinophilia; Leukopenia; Thrombocytosis;
Leukocytosis; Neutrophilia; Transfusion; Cameroon
Abbreviations
ARV: Anti-Retroviral Therapy; HAART: Highly Active
Antiretroviral Therapy; UPEC: Unit In charge of People Living
with HIV/AIDS; AZT: Zidovudine; 3TC: Stavudine, NVP:
Nevirapine; EFV: Efavirenz; TDF: Tenofovir Disoproxil Fumarate;
LPV/r: Liponavir/Ritonavir
Introduction
In Cameroon, the percentage of HIV positive patients on
treatment was approximately 6.5% between 2012 and 2013 [1].
By the end of December 2013, 131,531 HIV positive patients
were on treatment in the country with coverage of 47.4%. In the
south west region of Cameroon, 454 children and 13,473 adults
are on treatment [1], making them the fourth largest cohort in
the region receiving treatment. The regimens commonly used
for adults in the south west region of Cameroon comprise of
lamivudine (3TC), tenofovir (TDF), stavudine (d4T) or zidovudine
(AZT), and nevirapine (NVP) or efavirenz (EFV), which are
grouped as regimen A(AZT/3TC/NVP), B(AZT/3TC+EFV),
C(TDF/3TC+NVP), D(TDF/3TC/EFV) and 2C(TDF/3TC+LPV/r).
Studies have shown associations between Hematological-related
disorders with antiretroviral drugs (ARV) [2,3]. But, studies on
the prevalence of hematological abnormalities with respect to
duration on Highly Active Antiretroviral Therapy (HAART) have
not been documented in Cameroon. The adverse effects of
lamivudine in combination with zidovudine include neutropenia,
anemia, thrombocytopenia and transient rise in liver enzymes
[4], while that of nevirapine has been reported as eosinophilia,
granulopenia and jaundice. On their part, anemia, neutropenia,
and thrombocytopenia have also been reported as adverse
effects of stavudine [5]. A global total of 36,700,000 people were
living with HIV in 2015, of which 6,400,000 of them were
identified in West and Central Africa. The Antiretroviral therapy
(ART) coverage in West and Central Africa stands at 28%, with a
total of 1,796,460 patients on HAART [6]. By the year 2020,
programme managers in the Cameroon National AID committee
plan to provide coverage for more than 80% of the people (aged
15 and older) who need ART. This will help to prevent new
infections and equally reduce the number of people in need of
treatment, and decrease the resources required for ART in the
future [7,8]. Data on the prevalence of hematological disorders
in Cameroon are scarce. Studies have shown that over 65% of
patients with HIV infection at some point become anemic [2].
Anemia is of varied etiology and hence requires careful workup.
Similarly, thrombocytopenia of immune origin is common
and often an early manifestation of the disease. Although less
commonly discussed, neutropenia also occurs in these patients.
Hematology parameters are important monitoring tools for
assessing treatment and prognosis in HIV [9-11]. First-line ART
regimens recommended for adults in Cameroon include
lamivudine (3TC), tenofovir (TDF), stavudine (d4T) or zidovudine
(AZT), and nevirapine (NVP) or efavirenz (EFV) in a combination
of two Nucleotide or Nucleoside Reverse Transcriptase
Inhibitors/Non-Nucleoside Reverse Transcriptase Inhibitors
(NRTIs/NNRTI) A(AZT/3TC/NVP), B(AZT/3TC+EFV), C(TDF/3TC
+NVP), D(TDF/3TC/EFV) [12]. Mathews, 2013 [13] demonstrated that the hematological abnormalities (anemia,
thrombocytopenia, neutropenia, eosinophilia and leucopenia)
are prevalent through all stages of the disease, and that some of
these may serve as indicators of clinical progression. Being one
of the major direct causes of death in most HIV/AIDS patients on
treatment, anemia comes with the need to know the prevalence
of such abnormalities during treatment. Furthermore, studies
have shown that some severely immune-suppressed HIV- 1
infected patients receive transfusions in the course of their
illness. The Frequency of multiple infections of varied types and
origins, and zidovudine (AZT) therapy can contribute to the
anemia that necessitates transfusion. However, whether
transfusion increases the likelihood of opportunistic infection in
such patients has not yet been resolved [14]. A previous study of
HIV-l-infected patients not receiving AZT suggests that
transfusion has a deleterious effect on survival [15]. But,
transfusion records and its association with duration,
sociodemographic and ART regimens during ARV treatments in
Cameroon have not been documented. This study, therefore
seeks to ascertain the magnitude of hematological related
disorders in patients on ART in the south west region of
Cameroon, with respect to duration on HAART and the
frequency of transfusion in relation to other factors among
these patients after initiation on ARV treatment.
Methodology
Study design
A cross-sectional study was conducted on 285 adult patients
with HIV, who received HAART in selected HIV treatment centres
in the south west region of Cameroon between January 2015
and May 2015.
Study population
Eligible participants, with adherence level on HAART >95%
were solicited for the study. The study population was divided
into four groups based on the duration of ART. Group one (6
months-1 year), group two (>1 year-3 years), group three (>3
years-5 years) and group four (>5 years). Adult HIV positive
pregnant women, children and patients on other medications
(Traditional herbs, anti-malarial, anti-tuberculosis) at the time of
sampling were excluded from the study (Table 1).
| Variables |
ARV patients |
DURATION |
| (n = 285) |
6 months - 1year |
> 1 year - 3 years |
> 3 years - 5 years |
> 5 years |
| (n = 71) |
(n = 72) |
(n = 71) |
(n= 71) |
| Age |
| 20-35 |
93 (32.6%) |
36 (50.7%) |
27 (37.5%) |
19 (26.8%) |
11 (15.5%) |
| 36-45 |
106 (37.2%) |
25 (35.2%) |
31 (43.1%) |
26 (36.6%) |
24 (33.8%) |
| >45 |
86 (30.2%) |
10 (14.1%) |
14 (19.4%) |
26 (36.6%) |
36 (50.7%) |
| Sex |
| Male |
69 (24.2%) |
22 (31.0%) |
17 (23.6%) |
13 (18.3%) |
17 (23.9%) |
| Female |
216 (75.8%) |
49(69.0%) |
55 (76.4%) |
58 (81.7%) |
54 (76.1%) |
| Regimen |
| A(AZT/3TC/NVP) |
51 (17.9%) |
6 (8.5%) |
8 (11.1%) |
16 (22.5%) |
21(29.6%) |
| B(AZT/3TC+EFV) |
8 (2.8%) |
0(0%) |
4 (5.6%) |
1 (1.4%) |
3 (4.2%) |
| C(TDF/3TC+NVP) |
48 (17.2%) |
16 (22.5%) |
15 (20.8%) |
9 (12.7%) |
9 (12.7%) |
| D(TDF/3TC/EFV) |
172 (60.4%) |
47 (66.2%) |
45 (62.5%) |
44 (62.0%) |
36 (50.7%) |
| 2C(TDF/3TC+LPV/r) |
5 (1.8%) |
2 (2.8%) |
0 (0%) |
1 (1.4%) |
2 (2.8%) |
| Mean |
| CD4+ T CELL (cell/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
- |
391.2 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 83.4 |
477.3 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 121.9 |
655.3 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 232.8 |
649.1 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 370 |
| CD8+ T CELL (cell/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
- |
901.3 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 342.4 |
884.9 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 331.2 |
920.2 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 370 |
900.7 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 274.9 |
Table 1 Demographic characteristics of study participants.
Study sites/settings
The study was carried out in the south west region of
Cameroon, precisely in the following health institutions: Buea
Regional Hospital, Limbe Regional Hospital, Kumba District
Hospital, Mamfe District Hospital and Muyuka District Hospital.
These are government institutions with authorised HIV
treatment centres. The treatment centres have Unit in-charge of
patients with HIV (UPEC) where all patients go to receive
treatments and consult, and a sample collection unit where
samples are collected before being sent to the laboratory for
analysis.
Laboratory procedure
Venous blood (4 ml) was collected and stored in two 5 ml
ethylene-diamine-tetra-acetate (EDTA) vacutainer tubes, and the
whole blood sample was processed within 5 h after collection.
The full blood count parameters measured consisted of
hemoglobin (Hgb), hematocrit (HCT), white blood count (WBC),
platelet (PLT) and differential T lymphocytes with the Auto
Hematology Analyzer (Hematology analyzer Sysmex KX-21).
Before analysis, blood samples in the 5 ml EDTA tubes (k3-EDTA
salt) were homogenised on a rotary mixer for two minutes. The
tubes were uncapped and the probe of the analyzer immersed
into the tubes. The probe sipped approximately 15 μL of blood,
and results were generated within 30-45 s. Five microlitres (5 μL)
of venous blood, was used to prepare a thin film.
Variables taken, data sources and data collection
Hemoglobin, eosinophils, platelets, total white cell count, and
neutrophils were used to determine the hematological
disorders. Anemia classification was as follows: non-anemic
(Hgb>12 g/dL), mild (9.6-11.9 g/dL), Moderate (8.0-9.5) and
severe (<8.0 g/dL) [16]. Eosinophilia was defined as >3%;
thrombocytopenia was define as platelets <150 cells/μL;
leukopenia was define at WBC<4000 cells/μL and neutropenia
was define at <40%. Data on the socio-demographic and clinical
characteristics of the study participants were collected through
a pre-tested structured questionnaire, interviews and a review
of medical records. Findings from the patients’ records and
questionnaires were used to evaluate the adherence on
treatment and transfusion rate. A review of patients’ records
was also done to check for any other health complication that
might influence the hematology results within the time of data
collection. This was intended to note the number of time the
patient has been transfused for whole blood since the
commencement of HAART and any situation or period of pause
in taking treatment. Questionnaires were used to further
confirm or correlate some information collected from the records and also to obtain information on the demography of
participants.
Data analysis
Collected data were checked, edited for completeness and
processed before they were keyed into Excel 2013 and
transported to Statistical Package for Social Sciences (SPSS)
version 18 (SPSS Inc., Chicago.IL. USA) for Windows by a trained
technician. Analysis for any discrepancies between records of
the same patients was carried out in two databases. A
descriptive analysis was carried out to obtain the percentages
while ANOVA was used to test for differences between the
means in different duration. The Chi square test was used to
determine the relationships between transfusion and other
variables. P-value <0.05 was considered as statistically
significant.
Ethical consideration
Ethical clearance authorization letter was obtained from the
Institutional Review Board of the faculty of Health Sciences (IRBFHS),
University of Buea. A permission to conduct the study was
equally obtained from the regional delegation of public health
south west region of Cameroon, and from the treatment centres
of the hospital involved. Participants were informed about the
objectives of the study and they were assured of confidentiality
of every piece of information they provided. The participants
were equally given the right to withdraw in case they no longer
wanted to continue along the line. Written informed consents
were obtained from all participants.
Results
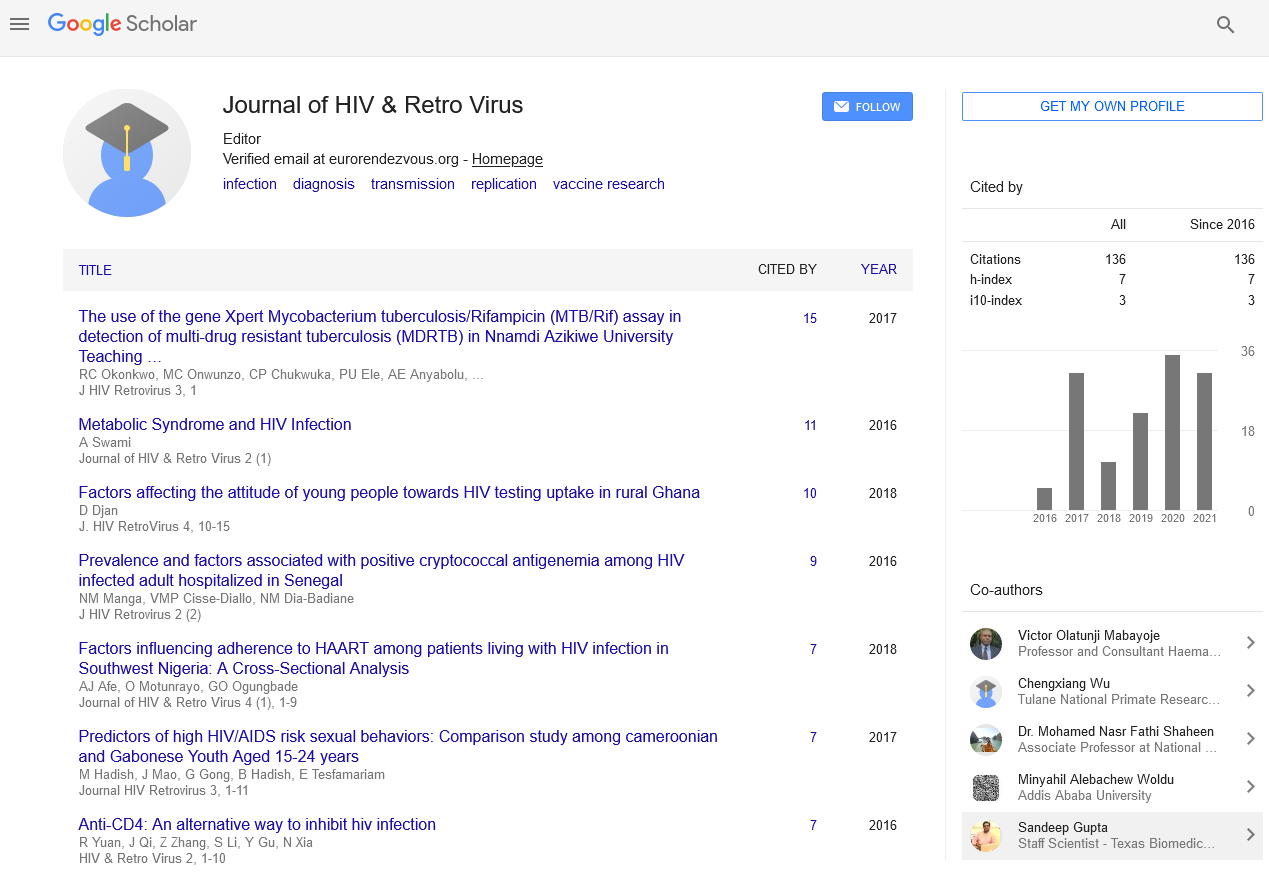
The hematological profiles of 285 HIV positive patients on
HAART were studied and transfusion occurrence recorded. Of
the 285 patients, 216 (75.8%) of the patients were females while
69 (24.2%) were males.
The overall mean age was 41 ± 11 years, within the range of
20-75 years. Furthermore, 172 (60.4%) of our study participants
were on regimen D(TDF/3TC/EFV), followed by 51 (17.9%) on
regimen A(AZT/3TC/NVP), 48 (16.8%) on regimen C(TDF/3TC
+NVP), 8 (2.8%) on regimen B(AZT/3TC+EFV), and lastly 5 (1.8%)
on regimen 2C(TDF/3TC+LPV/r) (Table 1). The mean CD4+ T-Cell
and CD8+ T Cells with respect to duration on HAART are
illustrated in Table 1.
| Variables |
ARV patients |
DURATION |
| (n = 285) |
6 months - 1year |
> 1 year - 3 years |
> 3 years - 5 years |
> 5 years |
| (n = 71) |
(n = 72) |
(n = 71) |
(n= 71) |
| Age |
| 20-35 |
93 (32.6%) |
36 (50.7%) |
27 (37.5%) |
19 (26.8%) |
11 (15.5%) |
| 36-45 |
106 (37.2%) |
25 (35.2%) |
31 (43.1%) |
26 (36.6%) |
24 (33.8%) |
| >45 |
86 (30.2%) |
10 (14.1%) |
14 (19.4%) |
26 (36.6%) |
36 (50.7%) |
| Sex |
| Male |
69 (24.2%) |
22 (31.0%) |
17 (23.6%) |
13 (18.3%) |
17 (23.9%) |
| Female |
216 (75.8%) |
49(69.0%) |
55 (76.4%) |
58 (81.7%) |
54 (76.1%) |
| Regimen |
| A(AZT/3TC/NVP) |
51 (17.9%) |
6 (8.5%) |
8 (11.1%) |
16 (22.5%) |
21(29.6%) |
| B(AZT/3TC+EFV) |
8 (2.8%) |
0(0%) |
4 (5.6%) |
1 (1.4%) |
3 (4.2%) |
| C(TDF/3TC+NVP) |
48 (17.2%) |
16 (22.5%) |
15 (20.8%) |
9 (12.7%) |
9 (12.7%) |
| D(TDF/3TC/EFV) |
172 (60.4%) |
47 (66.2%) |
45 (62.5%) |
44 (62.0%) |
36 (50.7%) |
| 2C(TDF/3TC+LPV/r) |
5 (1.8%) |
2 (2.8%) |
0 (0%) |
1 (1.4%) |
2 (2.8%) |
| Mean |
| CD4+ T CELL (cell/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
- |
391.2 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 83.4 |
477.3 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 121.9 |
655.3 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 232.8 |
649.1 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 370 |
| CD8+ T CELL (cell/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
- |
901.3 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 342.4 |
884.9 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 331.2 |
920.2 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 370 |
900.7 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 274.9 |
Table 1 Demographic characteristics of study participants.
Hematological monitory parameters for HIV follow-up can be
ascertain from the following hematological related disorders:
Anemia
After analysing our data, we observed that anemia occurred
in 167 (58.6%) of the 285 HIV patients (Figure 1). We also noted
that the prevalence of anemia decreased steadily with longer
time spent on the ART, from 18.2% in group one to 16.1% in
group two; 13.3% in group three and, 10.5% in group four.
Finally, the mean hemogloblin concentration was significant in
the various durations on HAART (P<0.001).
Figure 1: Prevalence of hematological abnormalities in patients on HAART in the south west region of Cameroon.
Eosinophilia
We equally found out that eosinophilia was the second most
common abnormality experienced by our subjects. Our findings
showed 115 of the 285 patients with an overall prevalence of
39.7% (Figure 1). The prevalence of eosinophilia decreased from
11.6% in group one to 10.2% in group two; and it increased back to 10.9% in group three, before decreasing finally to 7.7% in
group four patients on HAART (Table 2). In all the various
durations on HAART, mean eosinophilia was significant
(P<0.001) when compared to normal eosinophils count in our
study (Table 3).
| Parameters |
Group one (71)
6 months- 1 year |
Group two (72)
>1 year ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 3 years |
Group three (71)
>3 years ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 5 years |
Group four(71)
>5 years |
| Hemoglobin Hgb (g/dL) |
| Normal |
19 (26.8%) |
27 (37.5%) |
33 (46.5%) |
41 (57.7%) |
| Mild |
41 (57.7%) |
37 (51.4%) |
34 (47.9%) |
26 (36.6%) |
| Moderate |
11 (15.5%) |
8 (11.1%) |
3 (4.2%) |
4 (5.6%) |
| Severe |
- |
- |
1 (1.4%) |
- |
| Platelets PLT (cells/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
| Normal |
60 (84.5%) |
57 (79.2%) |
54 (76.1%) |
59 (83.1%) |
| Thrombocytopenia |
10 (14.1%) |
9 (12.5%) |
14 (19.7%) |
7 (9.9%) |
| Thrombocytosis |
1 (1.4%) |
6 (8.3%) |
3 (4.2%) |
5 (7%) |
| Eosinophils Eos (cells/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
| Normal |
38 (53.5%) |
43 (59.7%) |
40 (56.3%) |
49 (69%) |
| Eosinophilia |
33 (46.5%) |
29 (40.3%) |
31 (43.7%) |
22 (31%) |
| Neutrophils NEUT (%) |
| Normal |
51 (71.8%) |
51 (70.8%) |
52 (73.2%) |
45 (63.4%) |
| Neutropenia |
19 (26.8%) |
20 (27.8%) |
19 (26.8%) |
25 (35.2%) |
| Neutrophilia |
1 (1.4%) |
1 (1.4%) |
- |
1 (1.4%) |
| Total white blood cell count WBC (cells/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
| Normal |
54 (76.1%) |
58 (80.6%) |
54 (76.1%) |
58 (81.7%) |
| Leukopenia |
16 (22.5%) |
14 (19.4%) |
16 (22.5%) |
11 (15.5%) |
| Leukocytosis |
1 (1.4%) |
- |
1 (1.4%) |
2 (2.8%) |
Table 2 Hematological manifestations of HIV patients on HAART in the South West Region of Cameroon according to duration on ARV.
Neutropenia
We further observed in our study that neutropenia had an
overall prevalence of 28.8%, with 83 cases out of the 285
patients. In fact, neutropenia was more common among group
four patients on HAART, with a prevalence of 8.8%; while the
prevalence in group one, two and three were almost the same
with 6.7%, 7% and 6.7% respectively (Table 2). The mean
neutropenia was significant when compared to normal
neutrophil count in all the groups (P<0.001) (Table 3).
| Disorder |
NO |
Duration on HAART |
F |
P-value |
| Group one |
Group two |
Group three |
Group four |
| (mean ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ SD) |
(mean ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ SD) |
(mean ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ SD) |
(mean ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ SD) |
| Anemia (Hgb(g/dL)) |
| Mild |
138 |
10.71 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.57 |
10.96 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.68 |
11.11 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.61 |
11.17 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.61 |
3.905 |
0.01 |
| Moderate |
26 |
8.93 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.34 |
8.69 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.48 |
9.07 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.25 |
8.93 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0.62 |
0.717 |
0.552 |
| Severe |
1 |
- |
- |
7.2 |
- |
- |
- |
| Platelets (cells/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
| Thrombocytopenia |
40 |
114.50 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 23.26 |
128.33 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 17.56 |
134.36 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 16.84 |
126.14 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 20.64 |
2.064 |
0.122 |
| Thrombocytosis |
15 |
435 |
428.50 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 45.35 |
419.67 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 13.28 |
521.40 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 13.88 |
0.503 |
0.685 |
| Eosinophils (cells/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
| Eosinophilia |
115 |
6.30 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 2.82 |
6.31 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 2.11 |
5.71 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 1.67 |
5.86 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 1.98 |
0.57 |
0.636 |
| Neutrophils (%) |
| Neutropenia |
83 |
30.67 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 12.98 |
29.58 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 6.62 |
31.41 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 6.37 |
29.08 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 6.68 |
0.327 |
0.806 |
| Neutrophilia |
3 |
78 |
- |
76 |
78 |
- |
- |
| WBC (cells/ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâõL) |
| Leukopenia |
57 |
3,381 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0,47 |
3,157 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0,54 |
3,250 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0,55 |
3,473 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0,54 |
0.924 |
0.05 |
| Leukocytosis |
4 |
12,100 |
- |
11,600 |
15,100 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 3,54 |
0.427 |
0.734 |
Table 3 Comparing hematological disorders with respect to duration on HAART.
Neutrophilia
We also realised that neutrophilia was found in 3 cases of the
285 patients, with an overall prevalence of 1.1%. To be specific neutrophilia was found among groups one, two and four, with
equal prevalence of 0.4% respectively. Unlike the others
neutrophilia was not recorded among group three patients
(Table 2).
Leukopenia
Of the 285 patients, we noticed that 57 (20%) had leukopenia.
Leukopenia was recorded among groups one, two and three
patients with a prevalence of 5.6%, 4.9% and 5.6%, respectively;
while the least findings were seen among group four patients
with 3.9% (Table 2). It was also observed that duration on
HAART had a significant influence on mean normal WBC and abnormal WBC among groups one, two and three patients only
(P<0.005, P<0.001 and P<0.002, respectively) (Table 3).
Leukocytosis
We also found out that 4(1.4%) of the 285 patients had
leukocytosis. This was more prevalent among group four
patients with 0.7%; compare to groups one and three with the
same prevalence of 0.4% (Table 2). However Leukocytosis was
not observed among group two patients in our study.
Thrombocytopenia
Thrombocytopenia occurred in 40 (14%) of the 285 HIV
patients. The prevalence increased among group three patients
(4.9%); compared to groups one and two (3.5% and 3.2%
respectively). Group four patients had the least occurrence with
2.5% prevalence (Table 2). In addition the mean normal platelets
count of patients in group one on HAART had a significantly
higher level (P<0.017) than the abnormal platelets count, while
there were no significant differences from all the other groups
on HAART (Table 3).
Thrombocytosis
of the thrombocytosis cases were observed among group two
patients, with a prevalence of 2.1%; followed by group four with
1.8%; and the least was observed in group one with 0.4%
prevalence rate (Table 2).
Transfusion
Of the total number of study participants, 22 (7.7%) had
undergone transfusion after commencement of HAART. Also, we
noticed that transfusion occurrence was more common among
group two patients (8%), when compared to groups one (7%),
three (7%) and four (6%) (Table 4). Moreover, among the
participants, females had the highest record of transfusion (6%),
when compared to the males (1.6%). In addition, transfusion
was more prevalent among the age group 20-35 years (4.6 %),
followed by 36-45 years (1.6%), and lastly 1.4% in >45 years
(Table 4). From the HIV patients receiving different regimens
across the region, transfusion was mostly recorded from
regimen A (3.2%), followed by B (2.8%), C (1.4%); and lastly
regimen D (0.5%) with the least occurrence (Table 4).
| Demography |
Total |
Transfusion |
Group one (71) |
Group two (72) |
Group 3 (71) |
Group four (71) |
| 285 |
22 (7.7%) |
5 (7%) |
8 (11%) |
5 (7%) |
4 (6%) |
| Age |
| 20-35 |
93 |
13 (4.6%) |
4 |
5 |
3 |
1 |
| 36-45 |
106 |
5 (1.6%) |
1 |
2 |
1 |
1 |
| >45 |
86 |
4 (1.4%) |
- |
1 |
1 |
2 |
| Gender |
| Male |
69 |
5 (1.6%) |
1 |
2 |
2 |
0 |
| Female |
216 |
17 (6%) |
4 |
6 |
3 |
4 |
| Regimens |
| A(AZT/3TC/NVP) |
51 |
9 (3.2%) |
3 |
4 |
2 |
0 |
| B (AZT/3TC+EFV) |
8 |
8 (2.8%) |
1 |
3 |
2 |
2 |
| C(TDF/3TC+NVP) |
48 |
4 (1.4%) |
1 |
1 |
1 |
1 |
| D(TDF/3TC/EFV) |
173 |
1 (0.5%) |
- |
- |
- |
1 |
| 2C(TDF/3TC+LPV/r) |
5 |
- |
- |
- |
- |
- |
Table 4 Transfusion among HIV Patients on HAART in the South West Region of Cameroon.
The study’s results show that there is a significant association
between gender (P<0.001), age (P<0.020) and type of HAART regimen (P<0.001) with transfusion occurrence. But there was
no significant association in transfusion between the different
durations on HAART (P>0.05) (Table 5).
| Variables |
Transfusion |
X2 - Value |
P- Value |
| Yes |
No |
| Gender |
| Male |
13 |
58 |
15.807 |
< 0.001 |
| Female |
9 |
207 |
| Age |
| 20-35 |
13 |
79 |
7.839 |
0.02 |
| 36-45 |
5 |
102 |
| >45 |
4 |
82 |
| Regimen |
| A |
13 |
38 |
28.194 |
<0.001 |
| B |
0 |
8 |
| C |
1 |
47 |
| D |
8 |
165 |
| 2C |
0 |
5 |
| Duration |
| I |
5 |
66 |
1.603 |
0.64 |
| II |
8 |
64 |
| III |
5 |
66 |
| IV |
4 |
67 |
Table 5 Relationship between gender, age, regimen and duration on HAART with transfusion of HIV patients in the South West Region of Cameroon.
Discussion
The most common hematological abnormality observed in
this study was anemia with 58.6%. While 38 (13%) had
moderate anemia, 128 (44.9%) had mild anemia and 1 (0.4%)
had severe anemia, This might be as a result of the numerous
drugs used for the treatment of HIV patients in these treatment
centres; frequent changing of regimens for the patients without
any prior testing and other prophylaxis medications used for
opportunistic infections that might cause anemia from bone
marrow suppression. Drugs like ziduvodine and stavudine have
been associated with these abnormalities [2,4,5]. Also, both
mild and moderate anemia was found to be more prevalent in
patients on 6 months to 1 year on antiretroviral therapy, with 52
(18.2%) patients. The prevalence of anemia was equally found to
be lower as the duration on antiretroviral therapy increased. It is
worth pointing out that these findings are in accordance with
other studies carried out by Pandav et al. [17], Henry et al. [18];
and Sullivan et al. [19], who found out that anemia was more
prevalent in patients who have been on antiretroviral treatment
for less than 12 months; and that HAART reduces the prevalence
of anemia in patients with HIV/AIDS when taken for more than
12 months. Biological mechanisms may explain the variation in
anemia status during ARV therapy, given the high occurrence of
chronic disease and opportunistic infections that occur during
the early stages of HIV infections [20], and promote
inflammatory cytokines.
In addition the prevalence of neutropenia in this study was
29.1%; among which 25 (8.8%) were from group four. This may
be due to prolonged usage of zidovudine-based regimens among
these patients. There was no significant difference between the various durations of patients on HAART and neutropenia. These
findings are consistent with those of Enawgaw et al. [21], who
reported 28.3%. However, it is contrary to Pandav et al. [17]
findings that show a lower prevalence of neutropenia (2.4%).
Several mechanisms have been associated with neutropenia
which include the usage of several medications that are
commonly prescribed for HIV infected patients [5], decreased
colony growth of CFU-GM [22], the secretion of soluble
inhibitory substances by HIV infected cells [23], and decrease
serum levels of G-CSF [24].
On its part, the prevalence of thrombocytopenia in our study
participants was 14%. Thrombocytopenia was more prevalent in
group three with 4.9%, but it occurred in all the other durations
in an irregular pattern. The prevalence of thrombocytopenia in
this study was higher than that of Ballah et al. [25], Pandav et al.
[17], and Enawgaw et al. [21]. Duration on HAART was not
associated with reduced prevalence of thrombocytopenia. This
was in line with similar findings carried out by Ballah et al. [25]
that showed that there was no significant change in the level of
platelets throughout 30 month duration on HAART; while our
study was in contrast with that of Pandav et al. [17] that
reported HAART was associated with reduced prevalence of
thrombocytopenia. Mechanisms associated with
thrombocytopenia include an infection of the megakaryocytes
by HIV [26].
Thrombocytosis was seen in 5.3% of our patients, among
whom 6 (2.1%) were from group two. This is contrary to that
observed by Mathews et al. [13] that recorded 0.99%.
The overall prevalence of leukopenia in our study was 20%,
among which 16 (5.6%) were both from groups one and three.
Leukopenia was also prevalent with all duration on HAART, and
these findings are consistent with different studies such as those
carried out by Enawgaw et al. [21], (26.6%), Akinbami et al.
(26.8%) [10]. The findings of our study were contrary to those of
Pandav et al. [17], who recorded a 5% prevalence.
Leukocytosis had an overall prevalence of 1.4%. This might
illiterate the effective adherence of patients on their chemoprophylactic
therapy and ART. This finding is much lower than
that observed by Mathews et al. [13] who recorded 6.93%. It
probably reflects the effective usage of prophylaxis like
cotrimoxazole among our study participants against various
opportunistic infections that are more commonly associated
with leukocytosis in HIV patients.
Also the prevalence of eosinophilia among our study
participants was 39.7%. This high prevalence might be due to
parasitic infections that are mostly common in this region, and
different findings were reported by Mayar et al. [27] and
Mathews et al. [13], who reported a lower prevalence of 9.7%
and 1.6%, respectively in their studies.
Last but not the least, transfusion cases recorded in our study
was 25 (8.8%), from the total number of participants. Among
them, 8 (7.7%) were from group two and among participants on
regimen A (2.3%). A higher number in transfusion (30%) was
recorded in another study carried out by Walker et al. [28]. The
possible mechanisms might be due to severe adverse effects of lamivudine in combination with Zidovudine [2] and
hematopoietic failure [3].
Conclusion
The frequent transfusion and other abnormal hematological
manifestations of patients on highly active antiretroviral therapy
in most of the 5 HIV treatment centres in the south west region
of Cameroon clinically signify poor treatment response. Larger
sample sizes may be needed for confident conclusions to be
drawn. Pretesting of HAART regimen should be initiated in most
treatment centres for better management of the patients and
health personnel should be sensitive on the risk of changing
regimens without proper assessment of the patients. Further
studies on hematological manifestations and the rate of whole
blood transfusion in all the HIV treatment centres are needed in
order to develop effective measures, in preventing adverse
outcome in these patients on HAART.
Ethical Approval
This study was approved by the Faculty of Health Sciences
Institutional Review Board, University of Buea, Cameroon.
Availability of data and materials: At the University of Buea
main library
Competing interests: The authors declare that they have no
competing interests
Author Contributions
Simon Eyongabane Ako: was accountable for all aspects of
the work, in ensuring that questions related to the accuracy or
integrity of any part of the work were appropriately investigated
and resolved.
Longdoh Anna Njunda: gave the final approval of the version
to be published.
Eric Achidi Akum: made substantial contributions to the
conception and design of the work.
Jules Clement N. Assob and Pokam Thumamo Benjamin: critically studied the work for
important intellectual content.
Enoh Jude Eteneneng; Wabo Bernard
and Njouminie Fabrice : were involved in data collection,
analysis and drafting of the manuscript.
Acknowledgement
The authors would like to thank the directors, laboratory and
UPEC staff of the Buea Regional Hospital, the Limbe Regional
Hospital, the Mamfe District Hospital, the Kumba District
Hospital and the Muyuka District Hospital, for their permission
and help in the collection, processing and analysis of the
laboratory test.Also we thank the delegate at the Ministry of public Health South west region Cameroon , for clearance to effectuate this study and all the participants for their kind support and cooperation.
References
- https://files.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2014countries/CMR_narrative_report_2014.pdf
- Agarwal MB (2005) HIV HAART Related Haematological Disorders: Diagnosis and Management. Medicine Update 143: 705-708.
- Bain BJ (1997) The haematological features of HIV infection. Br J Haematol 99: 1-8.
- Akam AJ (2005) Prevalence of hepatotoxicity and numbers of CD4 cells in HIV/AIDS infected adult patients an antiretroviral therapy. A multi-centric study carried out in some major HIV treatment centers in Cameroon: HCY/CHU/PH. Bachelor of Medical laboratory Science, Department of Medical Laboratory Science, Faculty of health Sciences, University of Buea, Buea, Cameroon, dissertation 56.
- Koffi K, Gershy-Damet GM, Peeters M, Soro B, Rey JL, et al. (1992) Rapid spread of HIV infections in Abidjan, Ivory Coast, 1987-1990. Eur J Clin Microbiol Infect Dis 11: 271-273.
- https://www.who.int/hiv/data/en/
- https://www.healthpolicyinitiative.com/Publications/Documents/1250_1_Cameroon_EN_Singles_Reduced_acc.pdf
- Cameroon National Strategic Plan to Fight Against HIV, AIDS and STIs (2014-2017) Plan Strategique National de lutte Contre le VIH, le SIDA et les IST 2014-2017.
- Tripathi AK, Kalra P, Misra R, Kumar A, Gupta N (2005) Study of bone marrow abnormalities in patients with HIV Disease. J Assoc Physicians India 53: 105-110.
- Akinbami A, Oshinaike O, Adeyemo T, Adediran A, Dosunmu O, et al. (2010) Hematologic Abnormalities in Treatment-NaÃÆÃâÃâ ââ¬â¢ÃÆââ¬Å¡Ãâïve HIV Patients. Infect Dis: Research and Treatment 3: 45-49.
- Coyle TE (1997) Hematologic complications of human immunodeficiency virus infection and the acquired immunodeficiency syndrome. Med Clin North America 81: 449-470.
- Cameroon National Integrated HIV Guidelines (2014) Directives Nationales de Prevention et de Prise en Charge du VIH au Cameroun.
- Mathews SE, Srivastava D, Balayadav R, Sharma A (2013) Association of hematological profile of human immunodeficiency virus-positive patients with clinicoimmunologic stages of the disease. J Lab Physicians 5: 34-37.
- Sloand E, Kumar P, Klein HG, Merritt S, Sacher R (1994) Transfusion of blood components to persons infected with human immunodeficiency virus type 1: relationship to opportunistic infection. Transfusion 34: 48-53.
- Vamvakas E, Kaplan HS (1993) Early transfusion and length of survival in acquired immune deficiency syndrome: experience with a population receiving medical care at a public hospital. Transfusion 33: 111-118.
- https://www.who.int/vmnis/indicators/haemoglobin/en/
- Pandav AB, Nilkanth SP, Lanjewar DN, Bhagwat RV (2013) Haematological profile HIV positive patients in relation to immune status and stage of the disease ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â A hospital-based cohort from Western India. J Pharm Biomed Sci 36: 1877- 1886.
- Henry DM, Kukwah AT, Mbunkah HA, Bernard AN, Pascal NA, et al. (2014) Immunohaematologic and virologic responses and predictors of virologic failure in HIV-1 infected adults on firstline antiretroviral therapy in Cameroon. Infect Dis Poverty 3: 5.
- Sullivan PS, Hanson DI, Chu SY, Jones JL, Ward JW (1998) Epidemiology of anemia in human immunodeficiency virus infected persons: Results from the multistate Adult and Adolescent spectrum of HIV Disease Surveillance Project. Blood 91: 301-308.
- Semba RD, Shah N, Vlahov D (2001) Improvement of Anemia among HIV infected injection drug users receiving Highly Active Antiretroviral Therapy. J Acquir Immune Defic Syndr 26: 315-319.
- Enawgaw B, Alem M, Addis Z, Melku M (2014) Determination of hematological and immunological parameters among HIV positive patients taking highly active antiretroviral treatment and treatment naÃÆÃâÃâ ââ¬â¢ÃÆââ¬Å¡Ãâïve in the antiretroviral therapy clinic of Gondar University Hospital, Gondar, Northwest Ethiopia: a comparative cross-sectional study. BMC Hematol 14: 8.
- Bagnara GP, Zauli G, Glovannini M, Re MC, Furlini G, et al. (1990) Early loss of circulating hematopoietic progenitor cells in HIV-1 infected subjects. Exp Hematol 18: 426-430.
- Leiderman IZ, Greenberg ML, Adelsberg BR, Siegel FP (1987) A glycoprotein inhibitor of in vitro granulopoiesis associated with AIDS. Blood 70: 1267-1272.
- Mauss S, Steinmetz HT, Willers R, Manegold C, Kochanek M, et al. (1997) Induction of granulocyte colony-stimulating factor by acute febrile infection but not by neutropenia in HIV seropositive individuals. J Acquir Immune Defic Syndromes 14: 430-434.
- Ballah AD, Ibrahim Y, Hauwa SB, Ali UA, Abdullahi AB (2013) Changes in blood profile of human immunodeficiency virus (HIV)- infected patients on highly active antiretroviral therapy (HAART) in North Eastern Nigeria. J AIDS HIV Res 5: 284-291.
- Kouri YH, Borkowsky W, Nardi M, Karpatkin S, Basch RS (1993) Human megakaryocytes have a CD4 molecule capable of binding human immunodeficiency virus-1. Blood 81: 2664-2670.
- Mayar AM, Erick VW, Roberto A, Thomas G, Jose S (2014) Eosinophilia in HIV-infected patients. Baylor College of Medicine.
- Walker RE, Parker RI, Kovacs JA, Masur H, Lane HC, et al. (1988) Anemia and erythropoiesis in patients with the acquired immunodeficiency syndrome (AIDS) and Kaposi sarcoma treated with zidovudine. Ann Intern Med 108: 372-376.