Prerna Babbar1*, Manisha Biswal2, Behera Digamber3 and Anil Gupta1
1Department of Hospital Administration, Post Graduate Institute of Medical Education and Research, Chandigarh, India
2Department of Microbiology, Post Graduate Institute of Medical Education and Research, Chandigarh, India
3Department of Pulmonary Medicine, Post Graduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author:
Prerna Babbbar
Department of Hospital Administration
Post Graduate Institute of Medical Education and Research
Chandigarh, India
Tel: +919780281790
E-mail: dr.prerna.babbar@gmail.com
Received date: January 10, 2019; Accepted date: February 05, 2019; Published date: February 18, 2019
Citation: Babbar P, Biswal M, Behera D, Gupta A (2019) Healthcare Associated Infections in Intensive Care Units: A Pilot Study in a Tertiary Care Public Hospital in India J Prev Infec Contr Vol.5 No.1:1
Copyright: ©2019 Babbar P et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Healthcare associated infection; ICU; Average length of stay; Nosocomial infection
Background
A healthcare-associated infection (HAI) is a localized or systemic condition resulting from an adverse reaction to the presence of an infectious agent(s) or its toxin(s) that was not present on admission to the acute care facility. According to definition given by WHO, Healthcare associated infection is an infection acquired in hospital by a patient who was admitted for a reason other than that infection. This includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff of the facility. Data included in a report given by WHO [1] showed that pooled HAI prevalence in mixed patient populations was 7.6% in highincome countries. The European Centre for Disease Prevention and Control (ECDC) estimated that 41,31,000 patients are affected by approximately 45,44,100 episodes of HAI every year in Europe [1]. The estimated HAI incidence rate in the USA was 4.5% in 2002, corresponding to 9.3 infections per 1000 patientdays and 17 million affected patients. However, the report revealed an extremely fragmented picture of the endemic burden of HAI in developing world. Only very scanty information was available from some regions and no data at all for several countries (66%). Many studies conducted in health-care settings with limited resources reported HAI rates higher than in developed countries. Hospital-wide prevalence of HAI varied from 5.7% to 19.1% with a pooled prevalence of 10.1%. The risk of acquiring HAI is significantly higher in intensive care units (ICUs), with approximately 30% of patients affected by at least one episode of HAI with substantial associated morbidity and mortality.
HAIs occur worldwide and infections acquired in health care settings are among the major causes of death and increased morbidity among hospitalized patients. The economic costs of HAI are considerable. The impact of HAI implies prolonged hospital stay, long-term disability, increased resistance of microorganisms to antimicrobials, a massive additional financial burden for health systems, high costs for patients and their families, and excess deaths. In Europe, HAIs cause 16 million extra-days of hospital stay and 37,000 attributable deaths. Annual financial losses are estimated at approximately € 7 billion, including direct costs only. In the USA, approximately 99,000 deaths were attributed to HAI in 2002 and the annual economic impact was estimated at approximately US$ 6.5 billion in 2004 [2]. HAI surveillance is complex and requires the use of standardized criteria, availability of diagnostic facilities and expertise to conduct it and interpret the results. Surveillance systems for HAI exist in several high-income countries but are virtually non-existent in most low- and middle-income countries.
As evident from the WHO fact sheet, although HAI global estimates are not yet available, there is clear evidence that hundreds of millions of patients are affected every year worldwide, with the burden of disease much higher in low- and middle-income countries. The WHO report clearly suggested that there was an urgent need to establish reliable systems to gather data on the actual burden of HAI on a regular basis. It has been established that intensive care units (ICUs) consume a large proportion of hospital resources and that more than 20% of all healthcare associated infections occur in ICUs [3-5]. A study evaluating the impact of HAIs on average length of stay of patients in ICUs is necessary to provide a useful reference data for policy makers to formulate appropriate policies for controlling this menace and ensuring efficient utilization of scarce hospital beds.
This study was conducted with the aim of evaluating the impact of healthcare associated infections on average length of stay of patients in Respiratory ICU of a tertiary care teaching hospital.
Materials and Methods
This prospective matched cohort study was conducted in an 8-bed Respiratory ICU (RICU) of a 2000 bedded tertiary care teaching hospital of North India with a bed occupancy rate of 84%.
Patients who were admitted in Respiratory ICU of the study institute for 3 or more days during the study period of May 2014 to Oct 2014 were included in this study after due consent from patients or their relatives. The primary diagnosis, presenting signs, vitals and lab parameters of every patient at the time of admission was evaluated to calculate the severity of illness as per APACHE II score. The patients who met the inclusion criteria were followed up till they were transferred out of the RICU i.e., till they were discharged, they expired, or they left against medical advice. The records, lab reports /X-Rays and treating clinician’s opinion were utilized to look for development of HAI in every patient. In case a patient developed clinical signs and symptoms suggestive of a HAI, as felt by the clinician, necessary investigations were done to arrive at a definite diagnosis of HAI.
Cases were defined as those that were diagnosed to develop HAI in RICU as per CDC criteria [6]. Ventilator Associated Pneumonia (VAP), Central Line associated Bloodstream infection (CLABSI), Catheter associated Urinary Tract Infection (CAUTI), Surgical Site Infection (SSI), Clostridium difficile Infection (CDI) were the HAIs studied. These were diagnosed using CDC- NNIS and CDC-NHSN definitions for HAI following the methodology proposed by INICC. Patients admitted in RICU other than these were taken up as controls. Patients diagnosed to have a HAI prior to admission to RICU were not included in the study. However, if such a patient, during his stay in RICU developed an HAI that was different from that HAI which was present on admission, the patient was labelled as a case of HAI cases were matched to the controls based on age (in years+ 5 years), sex and average severity of illness using Acute Physiological and Chronic Health Evaluation (APACHE) II Score to avoid confounding of results.
All observations were entered in Microsoft Excel 2007. Normality of quantitative data was checked by measures of Kolmogorov Smirnov test of normality. Independent t-test and Chi square or Fisher's exact test, as applicable, was applied for comparison of 2 groups of normally distributed data. Mann- Whitney U-test was used as a test of significance for comparing matched cases and controls. All statistical tests were two-sided and performed at a significance level of α=0.05 using SPSS for Windows (version 17.0; SPSS Inc., Chicago, IL, USA).
This study was conducted with approval of Institute Ethics Committee of the hospital (Ref. No. NK/1248/MHA/21760-61) and informed consent was taken from study participants or their attendants.
Results
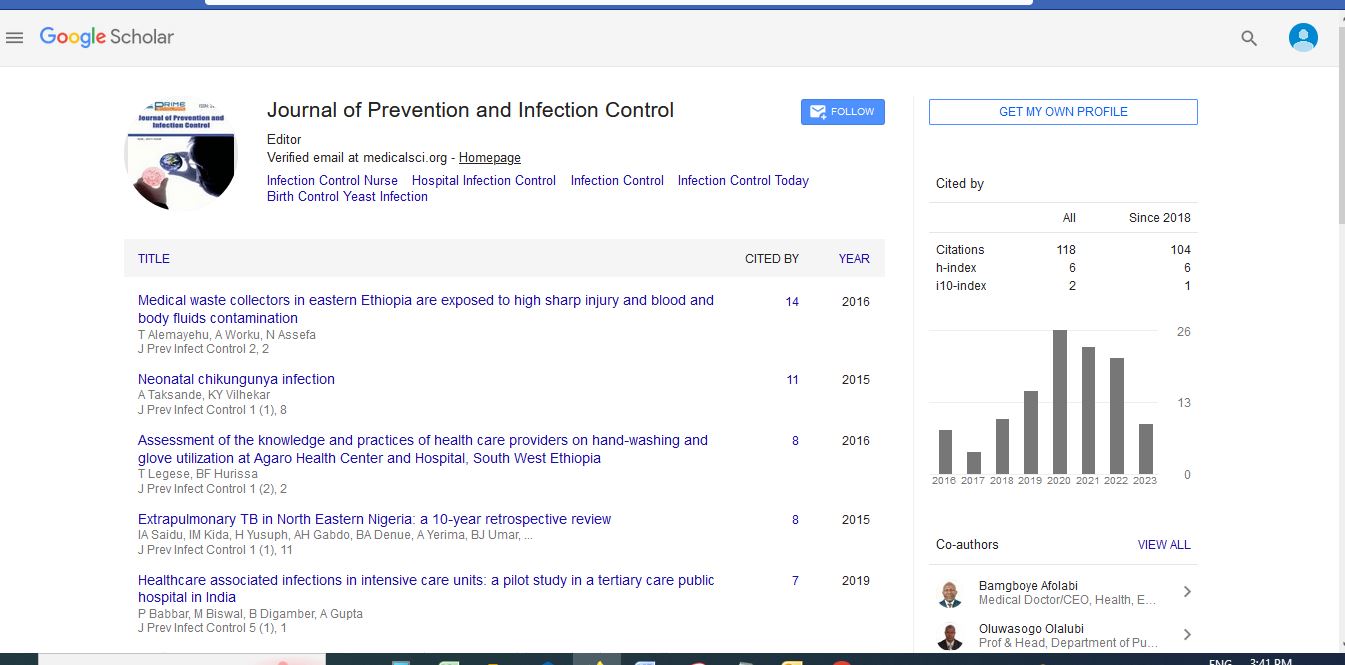
A cohort of 100 patients admitted in the Respiratory ICU of study institution during the period from May 2014 to Oct 2014 was observed. 47 of these study participants were males. The ages of the participants ranged from a minimum of 13 years to a maximum of 94 years a mean age of 42.92 years and SD of 20.424. Thirty (30) participants were below 25 years of age, thirty-two (32) patients between the ages of 26 years to 50 years, thirty-three (33) patients fell in the age group of 51-75 years and five (5) patients were more than 76 years old. The patients were followed up till they were transferred out of RICU, outcome as depicted in Figure 1. (LAMA: Left Against Medical Advice).

Figure 1: Outcome of stay of patients in RICU
On clinical evaluation 35 patients were found to have a single organ system affected, 40 patients had double organ system involvement and in 25 patients’ multiple systems (i.e. more than 2) were involved.
Twenty-nine (29) of these 100 patients developed a HAI as per criteria decided upon by the study team. These 29 patients developed 52 episodes of different types of HAI, but only the first episode of HAI was used for statistical procedures. 44.8% of the participants developed only a single episode of HAI. Ventilator associated pneumonia (VAP) was the most common HAI with 18 patients (62%) developing VAP, followed by Central line associated Bloodstream Infection (CLABSI) which was diagnosed in 6 patients (20.7%) and the least diagnosed HAI was CAUTI which was seen in 5 patients (17.2%), as in Figure 2.

Figure 2: Distribution chart of types of HAIs diagnosed in Cases.
The organisms that were isolated were Acinetobacter baumanii in 10 cases (34%), Pseudomonas aeruginosa in 8 cases (27.6%), Staphylococcus hemolyticus and Escherichia coli in 4 patients each (13.8% each), Klebsiella pneumonia in 2 cases (6.9%) and Enterobacter cloacae in 1 case (3.4%). The study population was followed up during their entire period of stay in the ICU. The patients were categorized as per the severity of their illness using the APACHE II scale (Table 1).
| APACHE II score categories |
Percent |
| <4 |
6 |
| 5-9 |
24 |
| 10-14 |
38 |
| 15-19 |
14 |
| 20-24 |
11 |
| 25-29 |
5 |
| 30-34 |
1 |
| >=35 |
1 |
| Total |
100 |
Table 1: Distribution of patients across APACHE II score categories.
The results clearly showed that patients admitted with more severe illness developed hospital acquired infection significantly more than patients admitted with a lower APACHE II score [X2 (7, N=100)=18.029, p=0.012] (Figure 1). This may be the result of a decreased immunity in patients admitted with a higher APACHE II score. Amongst the 29 cases, 31% expired and 69% were discharged while amongst the 71 controls, 11.3% of the patients expired, 85.9% were discharged and 2.8% took leave against medical advice. The results clearly showed a significantly higher mortality in patients who acquired hospital acquired infection vis’-a-vis’ the patients who did not [X2 (2, N=100)=6.280, p=0.043].
The mean length of stay for patients who did not develop any HAI during their stay in RICU was 8.56 days with SD of 6.725 days as compared to 23.45 days with SD of 16.862 days in patients who developed HAI.
Similarly, the median LOS for cases was found to be 22 days with IQR of 9.5 to 28.5 days while the median LOS for controls was found to be 6 days with IQR of 5 to 10 days.
The cases and controls were matched for age, gender and APACHE II scores to find any difference in the length of stay of cases and controls due to HAI. The results showed that patients who developed a HAI stayed in the hospital for an average of 11.96 days more than patients similar in age, gender and APACHE II score at the time of admission but who did not develop a HAI.
Median length of stay in two matched groups was 7 days for patients who did not develop HAI and 22 days for patients who developed HAI. The same are depicted in Figure 3.

Figure 3:Variation in the Average Length of Stay and Excess Length of Stay in matched Cases and Controls.
The average length of stay in two groups differed significantly (Mann Whitney U=101, n1=n2 =21, W=332, Z=-3.014, p=0.003).
Conclusion
Ventilator associated pneumonia was the commonest HAI diagnosed in this study which may be because patients in Respiratory Intensive Care Unit are predominantly admitted with compromised respiratory systems and are more frequently mechanically ventilated. Several other studies have also found VAP to be very common [7] while Graves et al. [8] found CAUTI and SSI to be the commonest infections. Although there were many instances of suspected cases of CDI, none of the patients developed a confirmed CDI or maybe they developed another HAI prior to the confirmation of the diagnosis of CDI and hence the diagnosis of CDI was not considered for statistical evaluation. Also, the reason for this could be inadequate surveillance practices and investigative laboratory procedures for diagnosis and confirmation of CDI. The most frequent causative organisms of HAI found in the study were A. baumanii and Pseudomonas aeruginosa which is consistent with the findings of Agarwal et al. [9].
The results showed a significant difference in the length of stay of patients who developed HAI. Patients who developed HAI stayed for an average of 14.9 days more than patients who did not develop HAI. Comparing similar patients by matching them for age, sex and severity of illness also showed that patients who developed HAI stayed for an average of 11.96 more days as compared to similar patients in the group who did not develop HAI. The difference in length of stay which corresponds with findings of several studies carried out in the West [10-17] as well those reported in India by Agarwal et al. [9]. However, Mahieu et al. [18] reported a much higher increase in length of stay due to HAI in a study conducted on neonatal population. This may be due to the varied population segment that was studied.
In a study that was conducted in a poly trauma and neurosurgery ICU at a 203-bedded Level IV trauma care facility in New Delhi, India, from May 1, 2012 to June 30, 2012 by Kumar et al. [19], total cost/bed/day for the multispecialty ICU was estimated to be INR 14,976.90. Considering that the patients who develop an HAI stayed for an average of extra 14.9 days, if development of an HAI is avoided whilst the patient’s stay in the ICU, there may be a saving of INR 2,23,155.81 per ICU bed per day. As this cost is borne both by the hospital and the patient in a varying degree of contribution, this added monetary benefit shall affect both the patient and the hospital, and by extension, the nation.
A challenge in quantifying the difference in length of stay between patients with and without infections is adequately adjusting for the severity of underlying illness, which may independently drive mortality as well as length and cost of hospitalization. Inadequate adjustment has been cited by investigators as a reason why HAIs may appear to have more adverse outcomes than in patients without any HAI. In this study, Acute Physiology and Chronic Health Evaluation score was used for categorizing ICU patients and the same may have improved the assessment of the true impact of HAI on length of stay. Nevertheless, hidden biases that were not adjusted for in this cohort may overestimate the true relationship between HAI and length of hospital stay. The development of more comprehensive validated methods for adjustment of underlying severity of illness and more stringent criteria for matching would improve strength of studies that examine outcomes of patients with HAI.
Nevertheless, the current study provides a window to the prevalence and impact of hospital acquired infection in the study institute which is a premier teaching hospital in the country. The only way developing countries can manage to meet the demand for hospital beds is by ensuring optimum utilization of available beds. Controlling hospital acquired infections is the most effective method to ensure this as these infections not only lead to avoidable morbidity and mortality but also prolong the length of stay of patients. This calls for a greater commitment from all stakeholders for implementing and more importantly monitoring infection control and surveillance policies. Similar large-scale studies may be conducted in all departments of the study institution for interdepartmental comparison on the impact on average LOS.
Limitations
This study has some important limitations, primarily the fact that only a single ICU in a tertiary care set up with modest number of admissions was examined. The length of the study was short, it being a pilot study in the Institute; hence number of cases was also limited. Also recognized was the challenge of reliably applying the CDC definitions to all the potential cases of various types of HAI, due to which, although minor, some data loss might have occurred.
Given the challenges of symptoms documentation and abstraction, some suspected cases of HAI, though were empirically treated with antibiotics, may have been missed from the actual categorization into the “case” group. Admittedly, matching or controlling for detailed individual characteristics could not be carried out. Adding too many parameters to the matching criteria would have resulted in too stringent criteria to pair a case and a control. This may mean that there is a residual confounding in the resulting estimates.
It is also possible that the total extra length of stay was not solely due to the HAI. For example, a patient’s stay increased due to the HAI initially, and then during this extra stay, another unrelated adverse event occurred, that in return added to the extra length of stay. Also, the follow up of the patient was carried out only till the patient was transferred out of RICU and not the entire patient journey and stay in the hospital.
Another significant concern is the management of timedependent bias. As has been established previously, the variables HAI and length of stay are interrelated by a reverse causality, i.e., HAI impacts the length of stay and a longer length of stay also increases the risk of development of a HAI. This might have led to biased estimates.
Recommendations
• Identifying local determinants of the HAI burden.
• Improving reporting and surveillance systems as standard procedures.
• Ensuring that core components for infection control are in place at the institute level.
• Implementing standard precautions, particularly best hand hygiene practices at the bedside.
• Improving staff education and accountability.
References
- World Health organization (2014) Health care-associated infections FACT SHEET.
- Graves N, Weinhold D, Tong E, Birrell F, Doidge S, et al. (2007) Effect of healthcare-acquired infection on length of hospital stay and cost Infect Control Hosp Epidemiol. 28: 280-92.
- National Nosocomial Infections Surveillance System report: data summary from January 1992-April 2000. Am J Infect Control 28: 449-453.
- Stone PW, Larson E, Kawar LN (2002) A systematic audit of economic evidence linking nosocomial infections and infection control interventions: 1990-2000. Am J Infect Control 30: 145-152.
- Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, et al. The prevalence of nosocomial infection in intensive care units in Europe: results of the European Prevalence of Infection in Intensive Care study. EPIC International Advisory Committee. JAMA 274: 639-644.
- (2014) CDC/NHSN Surveillance Definitions for Specific Types of Infections. Surveillance Definitions 17: 1-29.
- Spelman DW (2002) 2: Hospital-acquired infections. Med J Aust 176 :286-91.
- Graves N, Harbarth S, Beyersmann J, Barnett A, Halton K, et al. (2010) Estimating the cost of health care-associated infections: mind your p’s and q’s. Clin Infect Dis 50: 1017–1021.
- Agarwal R, Gupta D, Ray P, Aggarwal AN, Jindal SK (2006) Epidemiology, risk factors and outcomes of nosocomial infections in a respiratory intensive care unit in North India. J Infect. 53: 98-105.
- Abramczyk ML, Carvalho WB, Carvalho ES, Medeiros EAS (2003) Healthcare associated infection in a pediatric intensive care unit in a developing country. Brazilian J Infect Dis 7: 375-380.
- El-Nawawy AA, Abd El-Fattah MM, Abd El Raouf Metwally HA, El Din Barakat SS, Rehim Hassan IA (2005) One year study of bacterial and fungal healthcare associated infections among patients in pediatric intensive care unit (PICU) in Alexandria. J Trop Pediatr 52 :185-91.
- Raymond J, Aujard Y (2000). Healthcare associated infections in pediatric patients: a European, multi- center prospective study. Infect Control Hosp Epidemiol 21: 260-263.
- Urrea M, Pons M, Serra M, Latorre C, Palomeque A (2003) Prospective incidence study of healthcare associated infections in a pediatric intensive care unit. Pediatric Infect Dis J 22: 490-494.
- Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165: 867-903.
- American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator associated, and healthcare-associated pneumonia. Am J RespirCrit Care Med 171: 388–416.
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, et al. (2002) Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110: 285-291.
- Pittet D, Tarara D, Wenzel RP (1994) Nosocomial associated bloodstream infection in critically ill patients: excess length of stay, extra costs, and attributable mortality. JAMA 271: 1598-601.
- Mahieu LM, Buitenweg N, Beutels P, De Dooy JJ (2001) Additional hospital stay and charges due to hospital-acquired infections in a neonatal intensive care unit. J Hosp Infect 47: 223-229.
- Kumar P, Jithesh V, Gupta SK (2016) A comparative cost analysis of polytrauma and neurosurgery Intensive Care Units at an apex trauma care facility in India. Indian J Crit Care Med 20: 398-403.