Talal Abdulrahman Althomali*
Department of Surgery, College of Medicine, Taif University, Taif, Saudi Arabia
*Corresponding Author:
Althomali AT
Department of Surgery
College of Medicine
Taif University, Taif
Saudi Arabia
Tel: 056-688-9983
E-mail: tthomali@hotmail.com
Received date: April 9, 2016; Accepted date: June 2, 2016; Published date: June 8, 2015
Citation: Althomali AT (2016) Diplopia after General Anesthesia a Post-Operative Complication or Mere Coincidence? Case Report. J Eye Cataract Surg 2:11. doi: 10.21767/2471-8300.100011
Copyright: © 2016 Althomali AT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Anesthesia; Nerve; Diplopia
Introduction
Diplopia or extra-ocular muscle paralysis is a rare complication after surgery that has been mentioned in the context of literature as a possibility after spinal anesthesia [1]. The first case of diplopia after spinal anesthesia was reported by Koeppen more than a hundred years ago [2]. On the other hand diplopia after general anesthesia has been reported only once to our knowledge in 1972 in case of a child who had Hirschsprung's disease for which three major surgical procedures, requiring halothane anesthesia, had been performed. The unilateral sixth nerve palsy assumed to be related to prolonged general anaesthesia, after third procedure that lasted for almost seven hours [3]. Nonetheless, the latest major anesthesia textbooks describe little, if any, of this complication.
Case report
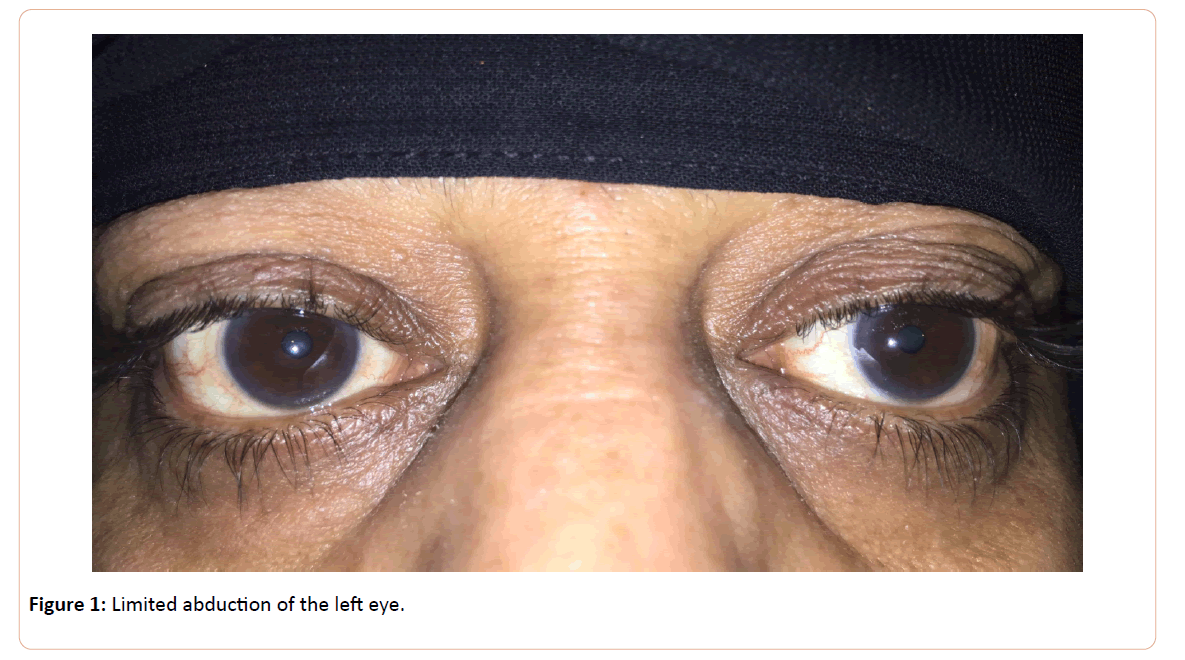
A 50 years old lady presented to our center seeking for medical advice about her recent onset of sudden painless double vision since two days [Figure 1]. Careful analysis of patient's history revealed recurrent episodes of headaches and facial numbness since three years associated sometimes with blurred vision especially on standing up from recombinant position but never diplopia. Chronic abdominal pain and recurrent attacks of diarrhoea since one year had been diagnosed as chronic calculus cholecystitis and she was scheduled for laparoscopic cholecystectomy that went fine two weeks before the onset of diplopia. On examination, visual acuity was 20/20 in both eyes, pupillary reflexes were intact and no ptosis or lid retraction was found. Ocular movement examination revealed limited abduction of left eye with incomitant esotropia measured 20 prism diopters in primary position. This esotropia is increased to 45 prism diopters in left gaze and disappeared in right gaze, is consistent with sixth nerve paresis of left eye. Ocular motility in all other directions was normal. Her intra-ocular pressure in both eyes was 14 mmHg. Both anterior and posterior segment examinations were unremarkable and she was diagnosed with acquired unilateral sixth nerve paresis recommended for further investigations.
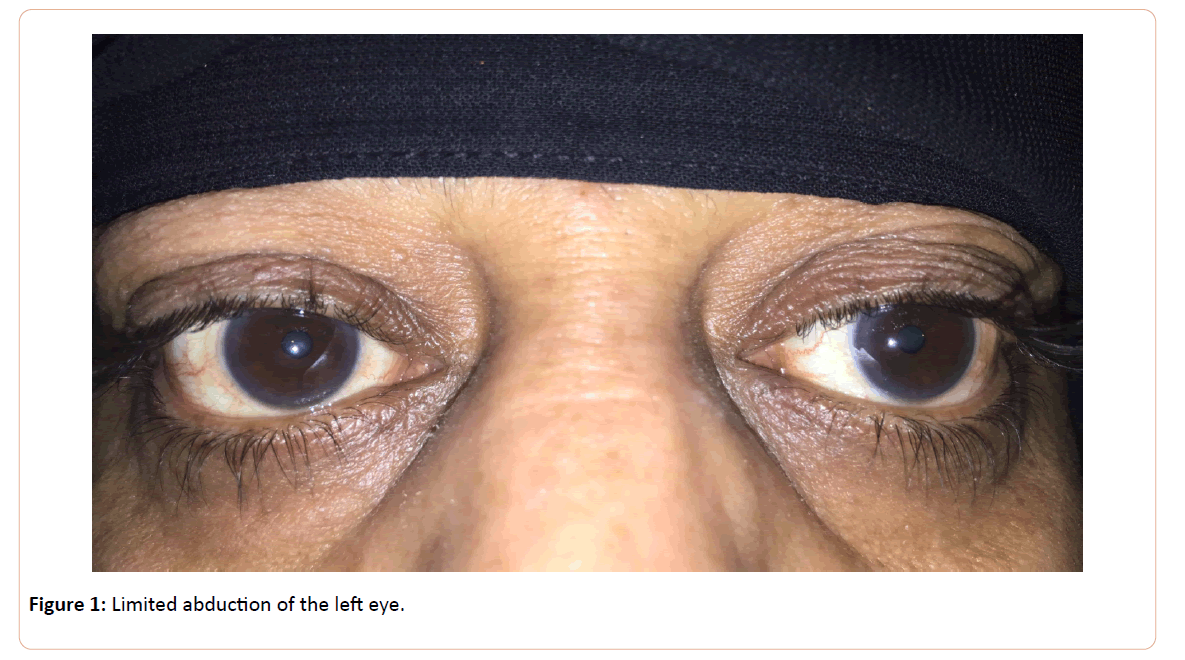
Figure 1: Limited abduction of the left eye.
Neurology consultation revealed with the aid of Magnetic resonance imaging MRI of brain, orbit and spinal cord that she had diffuse pachymeningeal gadolinium enhancement with imaging evidence of subdural fluid collection and engorged cerebral venous sinuses. She was diagnosed as a rare case of Spontaneous intracranial hypotension (SIH) and treated as so by epidural blood patch procedure. The patient was followed up closely with serial physical examinations without performing any additional treatment. The lateral movement restriction of both eyes were found to be considerably reduced after two weeks (post-operative fourth week) and spontaneous complete resolution of the symptom were noticed at the fourth week of the follow-up period (postoperative sixth week). No further management from our side were necessary and patient was informed to follow up only if there are any subsequent complaints.
Discussion
Although other cranial nerve palsies can occur after nonophthalmic surgeries done under different types of anesthesia, the abducens nerve (cranial nerve VI) is affected in the majority of cases (92–95%) [4]. Unilateral abducens nerve paresis were nearly as common as bilateral cases, Cerebrospinal fluid abnormalities were more frequent among the bilateral cases, but generally the same causes produced unilateral and bilateral sixth nerve palsy [5]. Although patient was insisting on that there is connection between her complaint and her surgery, late onset of diplopia and preoperative episodes of headache and facial numbness made us suspect that other causative pathologies might be present. Myasthenia, orbital muscle entrapment, convergence spasm and divergence palsy were entered into the differential diagnosis, but were not difficult to exclude. Spontaneous intracranial hypotension is typically encountered in middle age (30-50 years of age) and has a predilection for women (Female to Male ratio is 2:1) [6]. An epidural blood patch is highly effective method for treatment of SIH, with the reported success rate being as high as 93% for the first attempt [7]. Conservative treatment (such as an eye patch or prism glasses) is generally adequate to minimize the patient’s discomfort if delayed recovery were encountered. Fortunately there was no need for such manoeuvres. Surgical intervention should be postponed for at least 6-8 months in favor of spontaneous resolution.
Conclusions:
Although there was a logical assumption that there is connection between surgical procedure or anesthesia and the patient complaint but the late onset of the palsy, pre-operative symptoms, MRI findings and rapid recovery made the diagnosis and make the presented case unique compared with the other reports published before. This case is a good example for simultaneous pathologies independent from the surgery that may be encountered after performing surgical procedures, and multidisciplinary management is usually essential for the evaluation, diagnosis, and treatment of this kind of rare and unexpected problems.
References
- Day CJ, Shutt LE (1996) Auditory, ocular, and facial complications of central neural block: A review of possible mechanisms. RegAnesth.21: 197–201.
- Koeppen AH (1967) Abducens palsy after lumbar puncture. ProcWklySemin Neurol. 17: 68–76.
- BirndorfLA, Levy NS (1974) Isolated sixth nerve palsy following prolonged general anesthesia. J PedOphthalmol. 11:59–61.
- Hayman IR, Wood PM (1942) Abducens nerve paralysis following spinal anesthesia. Ann Surg.115: 864–8.
- Keane J R (1976) Bilateral sixth nerve palsy. Analysis of 125 cases. Arch. Neurol. 33: 681-3.
- Paldino M, Mogilner AY, Tenner MS (2003) Intracranial hypotension syndrome: a comprehensive review. Neurosurg Focus. 15 (6): ECP2.
- Rai A, Rosen C, Carpenter, Miele V (2005) Epidural blood patch at C2: diagnosis and treatment of spontaneous intracranial hypotension. AJNR Am J Neuroradiol. 26 (10): 2663-6.