Background: Adjunctive therapies are often combined with Scaling and Root
Planing (SRP) procedures to limit bacterial recolonization of periodontal pockets
and to modulate the wound healing environment. While local delivery antimicrobial
therapies are effective, they do not promote soft tissue repair at these sites.
BioXclude, a dehydrated human de-epithelialized amnion-chorion membrane
product (ddACM) sourced from donated human placental tissue, has been shown
to have antimicrobial properties, contain stimulatory growth factors known to
activate wound healing processes, and possess critical attachment substrates for
cellular adhesion and migration. Given this combination, it was hypothesized that
ddACM would be an effective adjunctive therapy for the treatment of periodontal
pockets following SRP procedures.
Methods: Sixteen non-smoking patients, compliant with a regular periodontal
maintenance program, were included in this study. A total of 30 sites showing a
≥ 2 mm increase in periodontal probing depth (PPD), with associated bleeding on
probing (BOP), were chosen for treatment. Following standard SRP procedures
with local anesthesia, ddACM was placed into the treated area. A six-week
periodontal re-evaluation was completed, with the primary outcome variable
being PD reduction and secondary outcomes that included resolution of bleeding
on probing (BOP).
Results: Mean PD reduction was 2.55 mm ± 0.34 mm, with three sites showing
≥ 4 mm ± 0.2 mm reduction in PD. BOP was resolved in 83% of the treated sites.
Conclusion: ddACM provides significant benefit as an adjunctive therapy to SRP
for the treatment of periodontal pockets in terms of PD reduction and resolution
of BOP.
Keywords
Periodontitis; Periodontal pocket; Root planing; Placental Allograft;
Amnion; Chorion
Introduction
According to a recent article published in the Journal of Clinical
Periodontology, severe periodontitis is the 6th most prevalent
disease worldwide, affecting nearly 743 million people globally
[1]. In the United States, it is estimated that roughly half of
adults over the age of 30 years old have periodontitis and that
the disease is the primary cause of tooth loss in this population
[2,3]. Periodontitis is a multifactorial disease of the oral cavity
with resident microorganisms playing a key role in its initiation
and pathogenesis [4] characterized as an inflammation of the periodontium, with the primary etiology being bacterial plaque,
periodontitis results when localized infection and inflammation
of the gingiva spread to the ligaments and bone that support
the teeth. If left untreated in a susceptible host, this results in
progressive break down of the supporting hard and soft tissues,
creating periodontal pockets acting as favorable environments
for continued destruction of the periodontium. Treatment
approaches for periodontitis will depend on the severity of the
disease. Interdental Clinical Attachment Level (CAL), Radiographic
Bone Loss (RBL), and tooth loss due to periodontitis are clinical/ radiographic parameters used to determine the severity of
periodontitis at specific sites. Non-surgical management of
periodontitis includes supra- and subgingival scaling and root
planing to remove diseased cementum and dentin to achieve
a biologically acceptable root surface, promoting a gain in
attachment. Scaling and Root Planing (SRP) procedures are often
combined with adjunctive therapies mainly aimed at preventing
the reestablishment of the bacterial infections [5,6].
The efficacy of adjunctive therapies to provide additional
benefit to SRP was reviewed by Smiley et al. in a 2015 article
published in the Journal of the American Dental Association
[7]. By systematically reviewing the results from clinical studies
published in peer reviewed journals and FDA filings, the authors
concluded that only systemic sub-antimicrobial dose doxycycline,
systemic antimicrobials, chlorhexidine chips, and photodynamic
therapy with a diode laser showed reliable, moderate benefit
over SRP alone. A low level of certainty was attributed to the
benefits of other adjunct therapies, including doxycycline
hyclate gel, minocycline microspheres, and other non-surgical
lasers. Of note, adjunctive therapies used with SRP procedures
are predominantly focused on the treatment and prevention
of persistent microbial infections that interfere with natural
tissue repair and regeneration processes. These treatments
do not, however, act to promote healing and the regeneration
of healthy connective tissue to repair the periodontal pockets.
Because of this, even the most efficacious adjunctive therapies
provide only a moderate benefit when compared to SRP alone
[7]. A product that provides anti-microbial properties to prevent
the recurrence of infection and factors to promote tissue repair
and regeneration would be of significant value to the treatment
of periodontal disease. BioXclude® (Snoasis Medical, Golden,
CO, USA), an emerging regenerative membrane product in the
field of dentistry and periodontics, has been shown to have
both antimicrobial and stimulatory properties, [8-14] suggesting
that it may be an ideal adjunctive product for the treatment of
periodontal pockets. Sourced from donated elective Caesarean
section placental tissues, BioXclude is a dehydrated human
de-epithelialized amnion-chorion membrane (ddACM) that is
cut into sheets of defined dimensions. ddACM has been used
successfully in a range of dental and periodontal procedures,
including maxillary sinus membrane repairs, [15] extraction site
management, [16] ridge augmentation procedures, [17] and
mandibular furcation repairs [18] Importantly, ddACM has been
shown to have both antimicrobial properties [8,9] and contain a
multitude of growth factors that stimulate wound healing and
tissue regeneration [19].
To evaluate the use of ddACM as an adjunctive treatment for
periodontal pockets, 16 non-smoking patients, compliant with
a regular periodontal maintenance program, with sites showing
a ≥ 2 mm increase in periodontal probing depth (PPDs) and
associated bleeding on probing (BOP) consented for inclusion
in this study. Following standard SRP procedures, ddACM was
placed into the periodontal pocket. A total of 30 sites were
treated, with an average initial PD of 6.98 mm ± 1.00 mm. All
patients underwent a comprehensive periodontal re-evaluation
after six weeks, where PD reduction and resolution of BOP were
measured. On average, PDs were improved by 2.55 mm ± 0.90 mm, with three sites showing ≥ 4 mm reduction in PD. In addition,
bleeding on probing (BOP) was resolved in 83% of the treated
sites. These data indicate that ddACM provides significant benefit
as an adjunct to SRP for the treatment of periodontal pockets in
terms of CAL gain and resolution of BOP.
Methods
Inclusion criteria
Non-smoking patients ≥ 18 years of age, currently compliant
in a regular periodontal maintenance program presenting with
periodontal pockets showing an increase in PPD of ≥ 2 mm and
associated BOP, were identified for inclusion in the study. Patients
with previous adjunctive or chemotherapeutic treatment in
addition to traditional maintenance procedures were excluded
from the study.
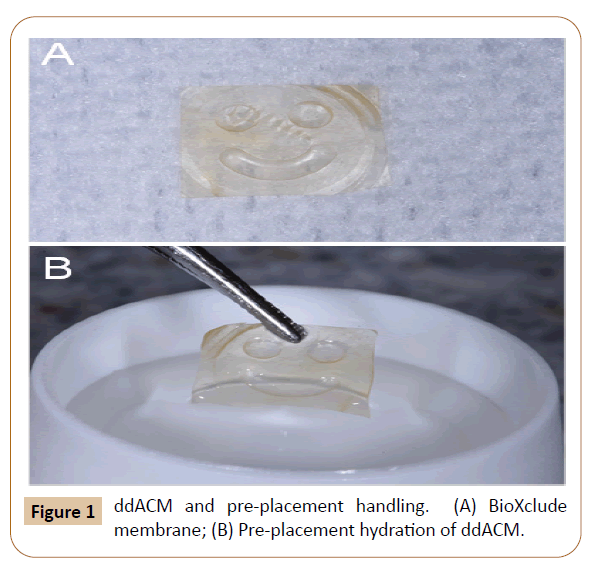
ddACM preparation
BioXclude membranes (Figure 1A) are individually packaged and
stored at room temperature for up to five years. At the time of
treatment, a membrane was removed from the sterile packaging
with a cotton forceps and hydrated (1-2 seconds) in sterile water
(Figure 1B). Longer hydration periods are not recommended by
the manufacturer to prevent a loss of soluble growth factors
stored in the membranes.
Figure 1: ddACM and pre-placement handling. (A) BioXclude membrane; (B) Pre-placement hydration of ddACM.
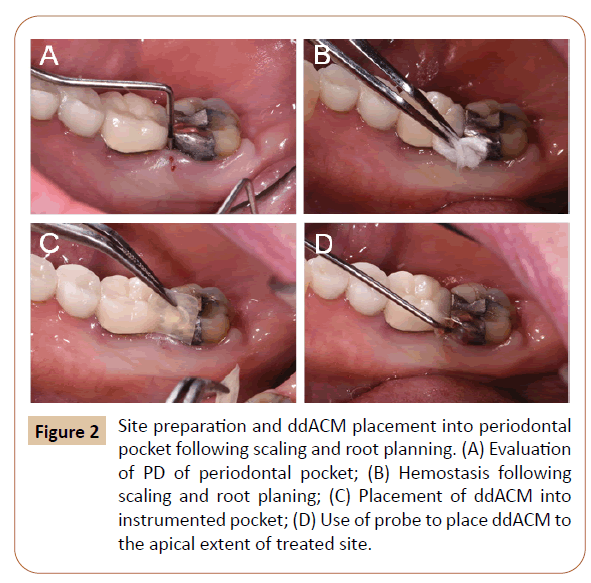
Procedure
Treatment sites (Figure 2A) were anesthetized with 4%
Articaine with 1:100,000 epinephrine. Teeth were then treated
with ultrasonic instrumentation followed by mechanical
instrumentation to diminish supragingival and subgingival plaque
and calculus via scaling and root planing. At each treatment site,
pressure was applied with gauze to achieve hemostasis (Figure
2B), and a pre-hydrated ddACM membrane (8 x 8 mm) was
introduced into the pocket with a cotton forceps (Figures 2C-2D).
A Hu-Friedy CP-12 periodontal probe was then used to place the membrane into the deepest extent of the periodontal pocket
achieving stability within the pocket and incorporation into the
forming fibrin clot created by localized bleeding following SRP.
No traditional antimicrobial agents (e.g. systemic antibiotics,
chlorohexidine washes, doxycycline hyclate gel, minocycline
microspheres, etc.) were used in these procedures.
Figure 2: Site preparation and ddACM placement into periodontal pocket following scaling and root planning. (A) Evaluation of PD of periodontal pocket; (B) Hemostasis following scaling and root planing; (C) Placement of ddACM into instrumented pocket; (D) Use of probe to place ddACM to the apical extent of treated site.
Post-operative instructions
Patients were provided post-operative instructions to continue
normal daily oral hygiene, implementing the modified Bass
brushing technique with gentle flossing; additionally, patients
were instructed to avoid any subgingival instrumentation,
including Perio-Aids, proxy brushes, and/or subgingival irrigation
for a period of six weeks.
Clinical evaluation
Measurements of PD, CAL, and presence of BOP were recorded at
the time of treatment by the doctor performing the procedure(s).
Six weeks after treatment, PD reduction and presence/absence of
BOP were recorded by a doctor who was blinded to the location
of sites treated with ddACM.
Results and Discussion
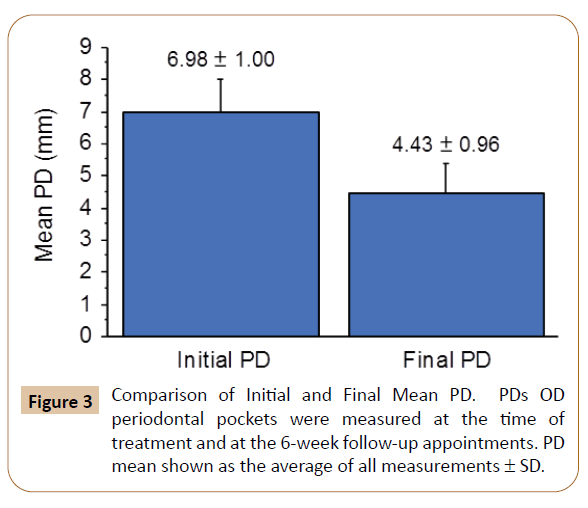
At the periodontal re-evaluation appointments, scheduled six
weeks after initial procedures, the average PD measurement
was 4.43 mm ± 0.96 mm, down from initial PD measures of 6.98
mm ± 1.00 mm. A nested plot showing PD measurements at the
time of treatment (“Initial PD”) and at the 6-week periodontal reevaluation
(“Final PD”) is shown in Figure 3. Mean PD reduction
was 2.55 mm ± 0.90 mm, with three sites showing ≥ 4 mm
reduction in PD. BOP was resolved in 83% of the treated sites.
These data are summarized in Table 1.
Figure 3: Comparison of Initial and Final Mean PD. PDs OD periodontal pockets were measured at the time of treatment and at the 6-week follow-up appointments. PD mean shown as the average of all measurements ± SD.
| Patients |
Sites |
Initial PD (mm) |
Final PD (mm) |
PD Reduction
(mm) |
Resolution
of BOP |
| Mean |
SD |
Mean |
SD |
Mean |
SD |
| 16 |
30 |
6.98 |
1 |
4.43 |
0.96 |
2.55 |
0.9 |
83% |
Table 1 Summary of PD, PD reduction, and resolution of BOP measurements.
Given the success of ddACM to promote rapid healing in a wide
range of periodontal procedures [15-18] it was hypothesized that it would also provide benefit in the treatment of periodontal
pockets. Adjunctive therapies are frequently combined with
SRP procedures to prevent the bacterial recolonization of the
pockets, but little is done to actively promote the healing of
damaged connective tissues and reattachment of at-risk teeth.
As a membrane product that possesses antimicrobial properties
to fight bacterial infections, stimulatory growth factors to activate
natural wound healing processes, and scaffolding matrix proteins
to support cellular attachment and migration, ddACM appeared
to have a potent combination of properties that would be of
use for the treatment of periodontal pockets. Historically, SRP
procedures lead to an average PD reduction of 0.49 mm (range:
0.36-0.62 mm), a number that is only improved by an additional
average reduction of ≤ 0.64 mm if adjunctive antimicrobial
therapies are included in the treatment regimen [19] As presented
in the results, periodontal pockets treated with ddACM following
standard SRP procedures had an average reduction in depth of
2.55 mm ± 0.34 mm after six weeks, suggesting that the use of
ddACM in these procedures is an effective adjunct to SRP and
that it may have additional benefit over therapies that are purely
antimicrobial in nature (SRP + antimicrobial adjuncts have a
combined effect of 1.13 mm average reduction in PD). The utility
of ddACM in a wide range of dental and periodontal procedures
is rapidly emerging. Originally considered a competitor in only
the membrane market, ddACM is proving to have a collection of
properties that makes it highly versatile and ideally suited for use
in a wide range of oral procedures.
In addition to the barrier function that is common to all membrane
products, ddACM’s ability to naturally prevent bacterial growth helps it to inhibit infections that are inherent to the oral cavity.
The innate growth factors and extracellular matrix contents
of ddACM, however, are what provide it with its additional
versatility. Growth factors and chemotactic signaling molecules in
ddACM activate wound healing responses while the extracellular
matrix proteins of ddACM scaffold critical cellular processes,
including attachment, migration, and new tissue deposition.
In the treatment of periodontal pockets, a procedure in which
barrier membranes are not traditionally used, the placement
of ddACM serves to prevent bacterial recolonization while
simultaneously activating would repair processes and providing
substrates for cellular migration and new tissue deposition. The
rationale for ddACM use in oral regenerative procedures arose
from documented use of placental tissues and ddACM specifically
in the medical arena. ddACM is proving to be an effective product in the treatment of chronic wounds, including diabetic foot
ulcers, venous ulcers, and burns [20-23].
Conclusion
Based on the same ddACM technology, MiMedx (Marietta, GA,
USA) offers a portfolio of dehydrated human amnion-chorion
membrane products that are quickly gaining market share due to
their efficacy in treating these hard-to-treat indications. Like dental
and periodontal indications, chronic wounds are characterized by
high bacterial loads that benefit from both the barrier function
and antimicrobial activity of the ddACM product. In addition,
chronic wounds are often accompanied by co-morbidities (i.e.,
diabetes, poor vascularity, etc.) that benefit from the active
stimulation and support of wound healing processes that ddACM
also provides.
References
- Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J (2017) Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol 44: 456-462.
- Palmer A (2013) Periodontitis among adults aged≥ 30 years—United States, 2009–2010. CDC Health Disparities and Inequalities Report— United States. MMWR Supplements 62: 129.
- Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, et al. (2015) Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 86: 611-622.
- Page RC, Kornman KS (1997) The pathogenesis of human periodontitis: An introduction. Periodontol 14: 9-11.
- Bonito AJ, Lux L, Lohr KN (2005) Impact of local adjuncts to scaling and root planing in periodontal disease therapy: a systematic review. J Periodontol 76: 1227-1236.
- Smiley CJ, Tracy SL, Abt E, Michalowicz BS, John MT, et al. (2015) Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc 146: 525-535.
- Smiley CJ, Tracy SL, Abt E, Michalowicz BS, John MT, et al. (2015) Systematic review and meta-analysis on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc 146: 508-524.
- Kjaergaard N, Hein M, Hyttel L, Helmig RB, Schønheyder HC, et al. (2001) Antibacterial properties of human amnion and chorion in vitro. Eur J Obstet Gynecol Reprod Biol 94: 224-229.
- Ashraf H, Font K, Powell C, Schurr M (2019) Antimicrobial activity of an amnion-chorion membrane to oral microbes. Int J Dent 2019:7.
- Koob TJ, Young CS, Lim JJ, Chinn K, Massee M, et al. (2016) A primer on amniotic membrane regenerative healing. MiMedx 170.
- Massee M, Chinn K, Lei J, Lim JJ, Young CS, et al. (2016) Dehydrated human amnion/chorion membrane regulates stem cell activity in vitro. J Biomed Mater Res 104: 1495-1503.
- Koob TJ, Lim JJ, Massee M, Zabek N, Rennert R, et al. (2014) Angiogenic properties of dehydrated human amnion/chorion allografts: therapeutic potential for soft tissue repair and regeneration. Vascul Cell 6: 1-10.
- Koob TJ, Rennert R, Zabek N, Massee M, Lim JJ, et al. (2013) Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J 10: 493-500.
- Maan ZN, Rennert RC, Koob TJ, Januszyk M, Li WW, et al. (2015) Cell recruitment by amnion chorion grafts promotes neovascularization. J Surg Res, 193: 953-962.
- Holtzclaw D (2015) Maxillary sinus membrane repair with amnion– chorion barriers: A retrospective case series. J periodontol 86: 936- 940.
- Cullum D, Lucas M (2019) Minimally invasive extraction site management with Dehydrated Amnion/Chorion Membrane (dHACM): Open-socket grafting. Compend Contin Educ Dent 40: 178-183.
- Rosen P, Yardley PA (2012) BioXclude Amnion Chorion Allograft in Combined Therapy for Ridge Augmentation with Immediate Implant Placement: A Case Report. Bioxclude/Snoasis Medical.
- Paul S, Stuart J, Cohen D (2015). Consecutive case series using a composite allograft containing mesenchymal cells with an amnion chorion barriers to treat mandibular class III/IV furcations. Int JPeriodon Restor Dent 35: 453-60.
- Koob TJ, Lim JJ, Zabek N, Massee M (2015) Cytokines in single layer amnion allografts compared to multilayer amnion/chorion allografts for wound healing. J Biomed Mater Res 103: 1133-1140.
- Zelen CM, Snyder RJ, Serena TE, Li WW (2015) The use of human amnion/chorion membrane in the clinical setting for lower extremity repair: A review. Clin Podiatr Med Surg 32: 135-146.
- Garoufalis M, Nagesh D, Sanchez PJ, Lenz R, Park SJ, et al. (2018) Use of dehydrated human amnion/chorion membrane allografts in more than 100 patients with six major types of refractory nonhealing wounds. J Am Podiatr Med Assoc 108: 84-89.
- Puyana S, Ruiz S, Elkbuli A, Bernal E, McKenney M, et al. (2020) The use of dehydrated human amniotic membrane versus amniotic/ chorionic membrane allografts to treat partial thickness facial burns. J Craniofac Surg 31: 201-203.
- Berhane CC, Brantley K, Williams S, Sutton E, Kappy C (2019) An evaluation of dehydrated human amnion/chorion membrane allografts for pressure ulcer treatment: A case series. J Wound Care 28: S4-S10.