Research Article - (2023) Volume 8, Issue 5
Deaf Dentists Diversifying Healthcare: Stories of Struggle and Success through a Comparative Case Report
Grace Phelan* and
Elizabeth Ayers
Deaf Health Care and Biomedical Sciences Hub, National Technical Institute for the Deaf, Rochester Institute of Technology, United States
*Correspondence:
Grace Phelan,
Deaf Health Care and Biomedical Sciences Hub, National Technical Institute for the Deaf, Rochester Institute of Technology,
United States,
Email:
Received: 04-Oct-2023, Manuscript No. IPJHCC-23-17862;
Editor assigned: 06-Oct-2023, Pre QC No. IPJHCC-23-17862 (PQ);
Reviewed: 20-Oct-2023, QC No. IPJHCC-23-17862;
Revised: 25-Oct-2023, Manuscript No. IPJHCC-23-17862 (R);
Published:
01-Nov-2023, DOI: 10.36846/2472-1654-8.5.8047
Abstract
Context: Deaf and hard of hearing (DHH) dentists are well suited to provide quality care for many diverse patients including those in the deaf community. However, DHH dentists face unique challenges in dental school, and as practicing medical professionals. Past research has focused only on hardships experienced by DHH dental patients. This
comparative case study aims to be the 1st formal effort to learn more about DHH dentists’ experiences and investigate strategic tools that could guide future DHH individuals pursuing dentistry.
Case report: This comparative case study was performed through observations and semi-structured interviews with two deaf dentists, and an interview with one hearing coworker each (n=4). Field notes were taken during each observation, and interviews were recorded and transcribed into English text. Thematic analysis identified three
common themes among participants:
1. Challenges faced and adaptations used by DHH dental professionals
2. Hearing peers’ support of, and learning experiences from deaf dentists and
3. Unique qualities deaf dentists possess.
Conclusion: Findings from this case study show minimal need for accommodations in most aspects of dentistry. The largest areas of concern regarded missing informal office communication, difficulty explaining complex terms, and challenges with captioning or interpreting in dental school/clinical. Hearing coworkers made small adjustments to support communication, and encouraged positive attitudes among patients. Both DHH dentists reported that their deafness contributed to their unique motivation to become a dentist, elevated skills in dentistry, and additional sense of responsibility for teaching oral health education to their DHH patients.
Keywords
Attitude; Communication; Delivery of health care; Dentistry; Hearing loss; Oral health; Sign language
Introduction
Background on Deafness
430 million people worldwide experience hearing loss that
impacts communication access [1]. In addition to communication
challenges, many deaf and Hard of Hearing (DHH) people
also experience lower socioeconomic status and lower health
literacy due to various struggles and systemic biases they face
[2,3]. Statistics show that the deaf community experiences
lower rates of postsecondary education completion and higher
rates of enrollment in community colleges or trade schools
than their hearing peers [4]. Hearing dentists will very likely
encounter DHH patients during their careers, and may not be
aware of the challenges involved, or familiar with methods to
provide adequate communication and treatment.
Challenges Faced in Dental Offices
Countless medical professionals and much of society, view
deafness as a malady that must be ‘fixed’ as opposed to a
diverse culture that should be embraced [5]. The persistent misconception that hearing aids and cochlear implants ‘cure’
deafness combined with lack of cultural competence knowledge
and unfamiliarity of non-verbal communication modes
contribute to a significant communication gap between dental
providers and their DHH patients [6]. The recurring nature of
dental appointments and the process of oral health education
can be especially challenging for both parties.
Common concerns DHH patients have regarding dental visits
include miscommunication, poor understanding, facial obstruction
due to masks, and background noise [7,8]. Negative
attitudes towards individuals with hearing loss by the auditory-
dominant society are another challenge [9,10]. Health
personnel tend to lack training on how to communicate and
interact with DHH patients which contributes to not only patient
dissatisfaction but also induces fear and anxiety for many,
resulting in less frequent dental visits [11-13]. In many cases,
these patients seek treatment only in dental emergencies [6].
When patients do not receive regular dental care, they typically
have limited oral health knowledge and worsened dental conditions.
Studies have shown that there exists a large knowledge
gap between hearing and DHH adolescents on proper tooth
brushing and a higher prevalence of dental caries and gingivitis
in DHH children [14-16]. It is evident that DHH patients don’t
typically receive adequate health care from hearing clinicians.
Prior Efforts towards Solutions and Accommodations
Challenges experienced by DHH patients in healthcare have
been well-documented as well as the advent of various strategies
to mitigate barriers, one being clinician use of introductory
American Sign Language (ASL). Jones and Cumberbatch reported
that Case Western Reserve University School of Dentistry
in the United States designed an ‘Introduction to Deafness’
course in the 1980s, though it was never actually offered [17].
The University of the West Indies in Jamaica was the 1st to actually
implement and sustain a sign language course; however
it is unknown whether their graduates continue using sign language
in their practice. The advantage behind sign language
training is that not only does it enhance dentists’ communication
ability with their DHH patients; it also develops a more
empathetic and culturally aware dentist. There is no record of
hearing dentists fluent in sign language of their nationality.
Kumar described an experiment with DHH adolescents using
Visual Performance Reinforcement (VPR) approach as an alternative
to extensive sign language training, or reliance on interpreters
in India [18]. The VPR technique included a video of
cartoon characters providing oral health education in sign language
with captions in English text. Following this, the provider
gave tooth brushing instructions on a model, and the patient
practiced on the model. This VPR technique showed statistically
significant success in lowering gingival and plaque scores in
DHH adolescents, and similar success was also observed with
DHH Saudi Arabian adults [19].
Additional accommodations may also need to be considered,
such as lowering or removing one’s face mask to allow for lip
reading during basic conversation. While lip reading is not completely
accurate, it continues to be a communication preference
for many DHH people as this mode is the most accepted
norm by mainstream society [20]. This practice was compromised
during facial mask mandations in light of the COVID-19
pandemic, placing additional stress on DHH patients and their
healthcare providers, hearing and DHH [21]. A wide spectrum
of communication preferences among people with hearing
loss arises from a combination of their educational and familial
backgrounds, and 1st language of acquisition [22]. Therefore,
accommodations are best developed through direct, individual
consultation with each patient to ensure their unique preferences
are most accurately adopted.
Limitations of Hearing Dentists
While many communication tools and accommodations may
seem like simple adjustments, they appear to be met with a
great deal of reluctance. It is ironic that healthcare professionals
learn about the etiology and biomechanics behind hearing
loss, yet common misconceptions about issues involving DHH
persist–their communication ability, intelligence level, literacy,
and sociocultural norms [23]. Today, many hearing dentists
continue to rely heavily on the lip reading abilities of their DHH
patients-which is known to be inaccurate and inadequate unto
itself [7,24,25]. Yet 62% of dental providers expect their adult
DHH patients to understand their articulation while using face
masks that cover their lips [11], which seems to be contradictory
to their medical training regarding hearing loss. Others use
written notes-which are time consuming and dependent on
individual literacy levels [7,12,24]. For ASL users, the medical
terminology and syntax differences between ASL and written
English may also impede full comprehension of what is being
explained [13]. Şuhani found that 68% of hearing dentists interviewed
believed they were not qualified to provide adequate
dental care to deaf patients due to communication barriers,
necessity of extended appointment times, and cost of interpreters,
with 16% outright refusing to provide care to DHH people
[26]. Hearing dentists may feel uncomfortable giving proper
care to DHH patients due to the absence of dental school curriculums
teaching necessary communication skills [22]. Barriers
to accessing dental care still exist, regardless of legislation
requiring effective communication among physicians and patients,
as outlined by the Americans with Disabilities Act (ADA)
passed in 1990 [22].
Benefits Deaf Dentists Offer
DHH healthcare providers are more willing to care for deaf people,
some reporting that 1/3rd of their caseload consists of DHH
patients [27]. Many deaf professionals redefine their career
success by serving others, which drives them to take on broader
roles where they can help more people in their communities
[28]. For example, many DHH physicians and dentists do not
specialize, but choose general paths where they can treat more
of their community members.
Deaf medical professionals are also more likely to provide
quality care by using effective communication strategies and
exhibiting cultural competency [29]. Examples of communication
strategies that deaf clinicians may be more aware of are
opening doors slowly when knocking is not an option, minimizing
background noise, facing the patient, ensuring adequate
lighting, and refraining from obscuring their face [22]. Due to
shared experiences, DHH medical providers are also more empathetic with their patients’ complex feelings surrounding their
deafness: Denial of hearing loss, mourning loss of communication,
sense of isolation, and feeling blamed for needing support
[22].
Not only can DHH healthcare professionals provide superior
care to their own patients, they often elevate their colleagues’
expertise and tolerance for treating DHH patients [30]. Similarly,
DHH healthcare students often educate their classmates
on communication and care strategies for the DHH population
[31]. Therefore, considering DHH dentists provide better care
and accessibility for DHH patients, it would be beneficial to
learn what tools can help support their success.
Existing Literature on DHH Medical Professionals
As we have seen throughout this review, supporting deaf dentists
is an effective way to augment patient care. However,
most existing literature focuses on DHH as patients and examines
what strategies could be utilized to accommodate them.
There is a research gap on challenges faced and adaptations
used by DHH professionals practicing dentistry and dental
school students. To date, we have not identified any prior research
specifically focused on DHH dentists; however, we have
found limited research that has been conducted concentrating
on DHH medical professionals in general.
One research study involving DHH medical professionals reported
high satisfaction rates regarding their accommodations,
which include modified stethoscopes, auditory equipment,
note-taking, Computer-Assisted Real-Time Captioning (CART),
signed interpretation, oral interpretation, and telephone adjustments
[30]. The biggest hindrance described in this study
was the significant amount of time each professional spent
arranging their own accommodations towards equal access
as their hearing counterparts. DHH dentists have their own
unique experiences and therefore may use different accommodations
than other medical professionals, or than previously
used in academic training. This needs to be investigated and
recorded to share among aspiring DHH dentists, so they can
have a greater chance to succeed and go on to serve the DHH
patient population.
DHH Students
In addition to supporting DHH dentists, DHH dental students
also need advocacy. Students with impairments, including
DHH students, are severely underrepresented in medicine and
dentistry [32]. One reason for under-representation is that
many teachers and parents do not encourage DHH students to
pursue advanced careers in science, technology, engineering,
and math (STEM) as they do for hearing students, leading to
discouragement and lack of belief that careers in any occupation
are achievable [33]. In addition, there is a paucity of deaf
role models in medical professions and in scientific fields. One
study reported that there are no deaf science teachers in any
schools for the deaf in New York State [31].
A significant barrier towards DHH matriculation into medical
training programs is technical standards. These standards list
traits or actions that medical students must have or be able
to perform without aid, rather than outcomes that could be
reached with reasonable accommodations [34]. These harsh
regulations prevent many students from applying to medical
and dental schools, and discourage others from disclosing their
disability [35]. However, many physicians experience hearing
loss later in life and continue practicing medicine, proving that
technical standards do not outline necessary attributes for
practicing medicine [31]. In fact, it is well-known that dental
professionals experience noise-induced hearing loss due to
high noise levels in the operatory [36], and yet they continue
practicing. Arguably, DHH students have more experience living
with hearing loss and therefore have more tools for success
than those that became deaf later in life. With this in consideration,
DHH students may actually be able to teach strategies
to hearing students and those who acquire deafness later in
age [31].
Accessing accommodations can also be challenging for DHH
students, because they often do not know what is available, or
what current technological advancements there are, such as in
amplified electronic stethoscopes [37,38]. Disability resource
providers are meant to assist in these situations, but most are
not trained in medical fields, and cannot provide adequate
advising [39]. Therefore, many DHH medical students struggle
to request appropriate accommodations. Some students
were more successful in developing strategies for overcoming
their hearing loss or requesting accommodations if they had
previous work experience [10]. However, students also must
disclose their disability if they request accommodations, thus
risking a shift in their teachers’ opinions of them [40]. Even if a
student had the knowledge, ability, and support to request access
services, 31% were denied those accommodations [38]. As
a result, it is often implied that using accommodations in medical
training or residencies is discouraged-a significant problem,
as studies have shown that DHH people who have inadequate
access to accommodations in school exhibit a higher prevalence
of depression [27].
Institutional Preparedness
Despite the countless struggles students encounter during
postsecondary schooling and medical training, most institutions
place the responsibility of being prepared for success
on the students themselves, many who do not know what resources
are available to them. Universities are responsible for
providing accommodations that assist DHH students in social
environments as well as in the classroom as mandated by ADA
and section 504 [40]. However, they insinuate that it is the student’s
responsibility to possess not only academic knowledge,
but also self-advocacy, leadership, and social skills for success
[41]. Some universities do not provide intersectional training in
cultural awareness and acceptance to ensure their faculties are
able to offer appropriate accommodations without bias. DHH
and other disabled students frequently experience identity
erasure, and seek homes where they fit in on their campuses
[42]. Most universities do not have the resources to support
intersectional students. Some institutions have tried to address
this by shifting their disability service offices to Disability Cultural
Centers, which aim to celebrate those students’ intersectional
identities [43].
Transition from School to Work
DHH students may struggle even more after postsecondary
school due to lack of preparation, additional challenges, and
identity changes. One study described a student as being
“shocked” to find out how difficult it was to fight for workplace
accommodations after graduation [38]. This study revealed
that institutions may need to take steps towards better student
preparation for the reality of the workforce. In other situations,
universities with strong social justice standards shelter
their students from discrimination, thus students are not well
prepared to handle prejudice encountered in their professions
[33]. Many DHH students feel that lack of understanding about
hearing loss will be the biggest barrier in their career success
due to negative attitudes and incidents of frustration from their
coworkers or employers [10,38]. Due to new challenges in a
post-graduation environment, many students will alter their
identity when they leave university and stop identifying as disabled,
for fear of others’ reactions [32]. A DHH person should
not have to hide parts of their identity, but it is often the result
of surviving in an ableist society.
On the other hand, academic curricula do not adequately expose
hearing healthcare students to caring for patients with
diverse abilities, which contributes to insufficient preparation
to meet their needs, such as the unique communication needs
of the DHH population [12]. Gilmore described an effort to expose
medical school students through an optional deaf awareness
and basic sign language module during their 2nd year [44].
Greene and Scott designed a Deaf Culture session during the
ear anatomy unit for medical school students in their 1st two
years, also with optional attendance [45]. A similar educational
workshop designed by Lock was also offered electively to 1st and 2nd year medical school students [23]. These short-term,
elective programs do not have lasting effects in the long term,
as evidenced by continued disparities in healthcare access for
DHH patients. Even more, these efforts do not benefit the rare
DHH healthcare student. The dental field needs to support not
only hearing professionals but also DHH individuals who can
succeed in their endeavors while celebrating their identities.
Goals of this Study
This study aims to learn the experiences of two practicing DHH
dentists, including their challenges and type of accommodations
used in dental school and in a dental practice. In addition
to the DHH dentists, two hearing coworkers will be included to
give their insights into what it is like to work with a DHH healthcare
professional, highlight where accommodations are most
needed, and what lessons can be learned from DHH dentists.
This information will be the 1st step towards building a knowledge
base that can support DHH dentists, dental students, and
hearing stakeholders. Culturally competent dentists trained in
ASL will provide a higher standard of care for DHH patients,
increasing their oral health literacy and overall dental hygiene.
Methods
Comparative Case Report
Ethical considerations: Ethical clearance was obtained from
our Institutional Research Board. This study strictly adhered to
the ethical standards of human experimentation and the Helsinki
Declaration of 1964, as amended in 2013.
Methods: Data was collected through observation and semi
structured interviews with two deaf dentists. At the time of
this research, there are 6 known DHH dentists (four in the United
States, One in the United Kingdom, and one in Egypt). Due
to the small sample population, two participants in the United
States were directly recruited. Prior to interviews, verbal and
written consent were obtained from each participant. Each interview
was video recorded and transcribed into English text
by a team of ASL interpreters and the interviewer. The observations
were performed over two full work days with each dentist.
A hearing coworker was recommended by each DHH dentist
and interviewed to learn their unique perspectives gained
by working with a deaf person as a healthcare professional, not
as a patient. Identifying information was removed or altered.
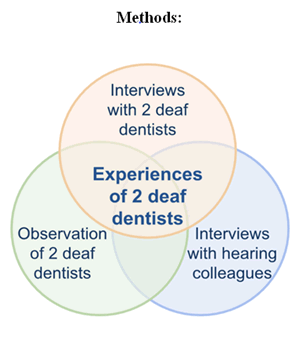
Study methods are illustrated in Figure 1.
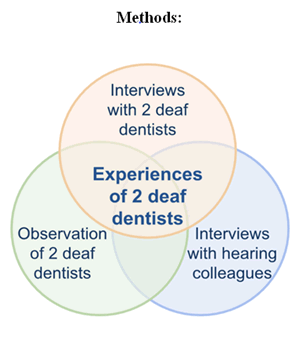
Figure 1: Diagram depicting study methods
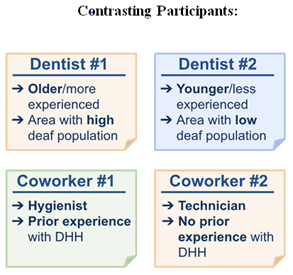
Participants: In an effort to gain a more holistic sense of how
DHH dentists function in their clinical environments, two participants
with contrasting features were recruited. Dentist #1 is
older, more experienced, and practices in an area with a large
DHH community. Dentist #2 is younger, less experienced, and
practices in an area with a smaller DHH community. Dentist #1
works in a large group practice while Dentist #2 practices as
an associate in a clinic (with hopes of branching out into their
own practice someday). Their hearing coworkers also brought
contrasting experiences, one being familiar with DHH in general
while the other had no prior experience with DHH. Figure 2 compares and contrasts the DHH dentist and hearing coworker
participants.
Interview structure: Interview questions focused on three
main themes:
• Challenges and adaptations used in a dental practice and
how those compared to dental school
• How a hearing dentist or coworker may offer support to, or
learn from a DHH dentist and
• What DHH dentists do differently than hearing dentists,
and how that might contribute to the larger DHH community
or their own sense of identity as a person with hearing
loss.
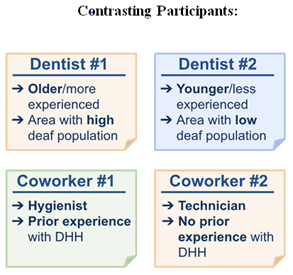
Figure 2: List of the main characteristics setting the participants apart
Participants were observed before their interviews, allowing
the interviewer to expand on the initial questionnaire to
include their unique individual experiences. Despite the differences
in these dental professionals’ backgrounds, there
were many clear similarities. The initial themes were strongly
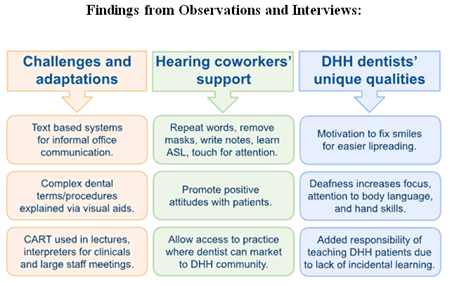
evident in their responses as well. Figure 3 summarizes each
theme and their associated findings.
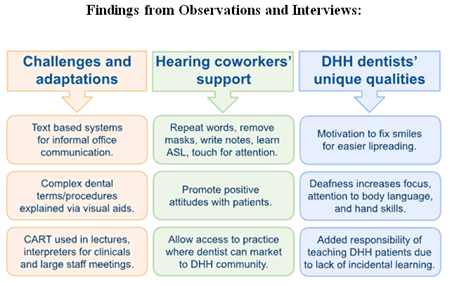
Figure 3: Model showing the main findings across the three themes
Theme 1: Challenges and adaptations: The 1st theme focused
on challenges faced by DHH professionals in dentistry and what
adaptations were used to overcome those challenges, as well
as how those experiences compared to dental school. Observations
revealed that dental appointments typically involve a
one-on-one interaction which eases communication challenges
during appointments. Indirect communication in the office still
posed challenges though. Dentist #1 uses a “text-based communication”
system in their office to communicate informal information
among coworkers, and email or text to communicate
with patients (personal communication, July 14, 2023). This
eliminates the use of phones, which was seen as the biggest
barrier in Dentist #1’s early career since there was no adaptive
technology such as teletypewriters, relay services, computers,
or cell phones. Technological advancement is largely responsible
for mitigating communication barriers. Dentist #1 explained
that their text-based system also benefits hearing colleagues,
as text messages can be “more efficient” and less “disrespectful
to the patient” (personal communication, July 14, 2023).
When asked about accommodations used in dental school,
Dentist #2 stated a preference for Communication Access
Real-time Translation (CART) during lectures to help with understanding
“big words and terminology.” However, during
clinicals, an interpreter was preferred due to challenges with
the additional delay in translation with captioning (personal
communication, July 27, 2023). Dentist #1 had no access to accommodations
during dental school, as ADA had not yet been
passed. Dentist #1 shared an example of self-advocacy used
instead. During an interview with a dental program, the room
was backlit making it hard to lipread the interviewers. Dentist
#1 asked the interviewers to relocate to the other side of the
room. This self-advocacy was recognized by the interviewers,
and they immediately accepted Dentist #1 into their program.
After ADA was passed, Dentist #1 was able to request interpreters
for work-related large-group interactions such as monthly
staff meetings and holiday parties held at their dental practice
(personal communication, July 14, 2023).
Theme 2: Hearing coworkers’ support: The 2nd theme investigated
how hearing coworkers can support or learn from a DHH
dentist. Observations revealed several strategies employed by
various hearing coworkers to make communication smoother.
When both dentists used their voice, their technician repeated
what was said for better patient understanding whenever
needed. The technician also repeated anything said by the patient
while the dentist’s back was turned. This was efficient because
the technician had prior knowledge and experience with
the terms being used and the procedures being performed.
During oral communication, coworkers removed their mask
temporarily so the DHH dentist could lip read. When this was
not possible in the operatory during the COVID-19 pandemic,
they wrote notes on paper. All coworkers were also careful to
obtain the DHH dentist’s attention via touch, light flashing, or
throwing a small object. This allowed for optimal face to face
communication and lipreading. Only a few of the hearing hygienists
or coworkers had any prior knowledge of ASL, but
one did learn a few signs such as “test” and “ready” to let the
DHH dentist know the patient was ready for an exam. Both
coworkers felt that there were no difficulties in making these
adjustments. Coworker #1 thought there were more challenges
in interacting with their DHH patients than with the DHH
dentist because “they’ve worked together so long” (personal
communication, July 19, 2023). Both coworkers spoke highly of
the DHH dentists, and feel that they have learned to be more patient while communicating with their own patients.
Hearing coworkers also support DHH dentists in their practice
by advocating for the DHH provider. Dentist #2 shared an anecdote
about a patient who had a negative reaction and did
not want to be seen by a DHH provider. The hearing colleagues
in that situation (a clinical setting in dental school) refused to
treat that patient, sending the patient to a different clinic in the
area (personal communication, July 27, 2023). This is a strong
demonstration of advocacy for the DHH dentist, and even more
powerful because another colleague could have offered to
treat the patient instead. Alternatively, they showed zero tolerance
for any discriminatory attitude.
Another way hearing coworkers can support DHH dentists is
helping them have access to a practice that allows them to embrace
their Deaf identity and market themselves to the DHH
community. Dentist #1 has years of experience, and works at a
large group practice located within a large deaf community, allowing
him to treat many DHH patients. Dentist #1 recalls feeling
very overwhelmed doing a residency in a hospital system
and feels much more supported in this group practice setting.
Contrarily, Dentist #2 is younger, and works as an associate at
a small practice where the patient pool is limited to prior existing
patients. Dentist #2 feels they must hide their Deaf identity
in their profession until they can open their own practice and
promote themself to the DHH community (personal communication,
July 27, 2023).
Dentist #1 recounts a time when he was discouraged from pursuing
dentistry by his teachers due to his deafness, but later
found encouragement from a DHH orthodontist during a shadowing
experience.
Well-meaning teachers would ask me what I wanted to do after
graduation. When I replied that I wanted to be a dentist, they
were adamant that I couldn’t be one. When I asked “why”, they
said, “Because you’re deaf”... I saw that the orthodontist was
deaf like me. He used lipreading with patients. He was a good
communicator, and he had a team of people to assist and help
with communication for him. There were no barriers to using
phones because his office workers were responsible for the
phones. He was focused on his patients, and he was friendly
and sociable with them. I thought, “If he could do it, I could
do it too.” I was even more determined to become a dentist.
(Personal communication, July 14, 2023).
DHH people pursuing a professional career face discouragement
from many hearing people, which makes support from
those in their field that much more important. It is also crucial
that DHH students have access to shadowing experiences with
DHH professionals, so they can observe and learn methods to
overcome the challenges they will face, and gain confidence in
themselves.
Theme 3: Deaf and hard of hearing Dentists’ unique qualities:
The final theme examined the unique qualities DHH dentists
possess that allow them to be well suited for the dental profession
and serve the DHH community. The 1st unique quality both
DHH dentists share is their motivation for becoming a dentist.
Both expressed a strong desire to fix teeth and improve peoples’
smiles to allow for easier lipreading.
Both DHH dentists also believe that their deafness gives them
additional skills that help them to succeed in dentistry professionally.
They reported that they have better focus, peripheral
vision, and attention to body language. An example described
by Dentist #1 was the ability to “see when the patient is clenching
their hands” and inquire whether they are in pain and need
more novocaine (personal communication, July 14, 2023).
Dentist #2 stated that growing up using sign language can help
DHH dentists be more “skilled with our hands” which in turn
enhances dexterous manipulation of tools in dentistry (personal
communication, July 27, 2023).
The last unique characteristic that both DHH dentists in this
study share is their sense of added responsibility for serving
and teaching DHH patients. Deaf people miss out on incidental
learning opportunities and therefore often have knowledge
gaps regarding many things, including their health. Dentist #1
takes this responsibility very seriously and always performs the
1st cleaning for every new DHH patient. Such appointments are
scheduled for an hour, which allows the time to “explain what’s
happening [and] fill in those gaps of dental information” (personal
communication, July 27, 2023). Dentist #2 does not treat
many DHH patients in their current practice, but still strives to
teach DHH patients by creating educational oral health videos
in ASL.
Results and Discussion
These findings describe important insights to two DHH dentists’
experiences. Through observation and interviews, we
learned their preferred accommodations in dental school and
in dental practice. In dental practice, fewer accommodations
were needed as most interactions were one-on-one. Support
from the hearing hygienists and technicians were seamless, as
the technicians and hygienists were well versed in the terminology
and procedure protocols. The ease of communication
in their dental practices is an encouraging sign for aspiring DHH
dentists.
In dental school, obtaining accommodations were successful,
but required individual proactivity and knowledge of their ADA
rights. Disclosing disability and showing competency in self-advocacy
are likely to help a student succeed in matriculating in
dental school. With recent social reform movements, dental
schools are looking to increase diversity in their incoming classes,
bolstered by studies demonstrating that a diverse healthcare
workforce contributes to increased quality of care given to
marginalized and underserved patients.
Technology has removed many barriers as well, enhancing text
and visual based communication. The development and widespread
use of intra-oral cameras, scanning systems, and better
X-rays allows the patient to see what is happening in their
mouth, and eases communication struggles for all dentists,
DHH included.
One challenge noted in this report is that for DHH dentists to
be able to market their services to the DHH population, they
must have access to a practice where that is a possibility, and
have the support from their coworkers to make that happen.
This is an additional challenge many young DHH professionals
face, as they may not have those resources when getting started
in their career. It is important for the dental community to
find a way to support DHH individuals in setting up their practice. These findings show that DHH dentists experience challenges,
but are well suited for careers in dentistry for a number
of reasons.
In addition, accommodations used by these professionals can
act as an example for aspiring DHH dentists to better prepare
for their own professional journeys. If these challenges can be
shared with stakeholders in the dentistry and deaf communities,
students can come prepared with solutions and resources
for dental school and have a better sense of what to expect
in their careers. Hearing instructors and coworkers can also be
better informed about working with DHH individuals. Many triumphs
were exemplified from the DHH dentists, and it is important
to share their successful strategies with the broader
community.
Conclusion
This study revealed that the two DHH dentists had unique motivations
in pursuing dentistry, exceptional skills to contribute,
and felt a responsibility to teach their marginalized patients.
It is our hope that this research is a 1st step towards building a
knowledge base for members of the deaf and dental communities
to draw from in supporting DHH dental professionals. Future
steps could include obtaining narratives from other DHH
dentists, DHH hygienists, and more hearing coworkers. Our
research uncovered a deaf-owned dental clinic run by a DHH
dentist with DHH technicians and staff. Their experiences warrant
further research. Considering recent efforts to implement
short-term modules in various medical training facilities, it is
worthwhile to investigate dental school curriculum for cultural
competence training, deaf awareness, or other content related
to care of minority patients that is mandatory, instead of optional
and long-term. It is our goal to continue learning more
about experiences of DHH dentists and their hearing coworkers
and consolidate their narratives into a repository that can be
shared amongst dental school students and instructors, as well
as those in the field.
Acknowledgement
We wish to thank each participant that took part in this project.
We also give our gratitude to Dr. Tiffany Panko, Jenna Stewardson,
and Deaf Healthcare and Biomedical Sciences Hub for
their support of this project. In addition, we appreciate the ASL
interpreters that helped transcribe our interviews: Kat Womack,
Emily Young, and Sydney Roy.
Conflict Of Interest
There are no conflicts of interest.
References
- World Health Organization (WHO) Deafness and hearing loss.
- Blanchfield BB, Feldman JJ, Dunbar JL, Gardner EN (2001) The severely to profoundly hearing-impaired population in the United States: Prevalence estimates and demographics. J Am Acad Audiol. 12(4):183-189.
[Crossref] [Google Scholar]
- McKee MM, Paasche-Orlow MK, Winters PC, Fiscella K, Zazove P, et al. (2015) Assessing health literacy in deaf American sign language users. J Health Commun. 20(sup2):92-100.
[Crossref] [Google Scholar]
- Newman L, Wagner M, Knokey AM, Marder C, Nagle K, et al. (2011) The post-high school outcomes of young adults with disabilities up to 8 years after high school: A report from the National Longitudinal Transition Study-2 (NLTS2). (NCSER 2011-3005). Menlo Park, CA: SRI International.
[Crossref] [Google Scholar]
- Katwe A, Santarossa S, Beaver S, Frydrych A, Kujan O (2023) Dental and oral health students' preparedness for the management of deaf patients: A cross-sectional survey. J Dent Sci. 18(4):1581-1587.
[Crossref] [Google Scholar]
- Gupta L, Jain P, Mora LN, Mujho T (2018) Evaluation of different visual method used to enhance communication skills between dental care providers and speech and hearing impaired patients. Indian J Dent Res. 29(4):418-422.
[Crossref] [Google Scholar]
- Masuku KP, Moroe N, van der Merwe D (2021) 'The world is not only for hearing people-It's for all people': The experiences of women who are deaf or hard of hearing in accessing healthcare services in Johannesburg, South Africa. Afr J Disabil. 10:1-8.
[Crossref] [Google Scholar]
- Samnieng P (2014) Dental cares for patients who have a hearing impairment. Int J Clin Prev Dent. 10(4):215-218.
[Crossref] [Google Scholar]
- Hauser PC, O'Hearn A, McKee M, Steider A, Thew D (2010) Deaf epistemology: Deafhood and deafness. Am Ann Deaf. 154(5):486-492.
[Crossref] [Google Scholar]
- Punch R, Creed PA, Hyde MB (2006) Career barriers perceived by hard-of-hearing adolescents: Implications for practice from a mixed-methods study. J Deaf Stud Deaf Educ. 11(2):224-237.
[Crossref] [Google Scholar]
- Campos V, Cartes-Velasquez R, McKee M (2020) Oral health and dental care in deaf and hard of hearing population: A scoping review. Oral Health Prev Dent. 18(1):417-426.
[Crossref] [Google Scholar]
- Chaveiro N, Porto CC, Barbosa MA (2009) The relation between deaf patients and the doctor. Braz J Otorhinolaryngol. 75(1):147-150.
[Crossref] [Google Scholar]
- Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P (2006) Health care system accessibility: Experiences and perceptions of deaf people. J Gen Intern medicine. 21(3):260-266.
[Crossref] [Google Scholar]
- Wei H, Wang YL, Cong XN, Tang WQ, Wei PM (2012) Survey and analysis of dental caries in students at a deaf-mute high school. Res Dev Disabil. 33(4):1279-1286.
[Crossref] [Google Scholar]
- Kalaivani S, Shavi GR, Shanmugam S, Sanga R, Gunasekaran L, et al. (2021) Oral health status of hearing and speech-impaired schoolchildren in Erode district, Tamil Nadu-A cross-sectional study. J Res Dental Sciences. 12:198-203.
[Google Scholar]
- Vignehsa H, Soh G, Lo G, Chellappah NK (1991) Dental health of disabled children in Singapore. Aust Dent J. 36(2):151156.
[Crossref] [Google Scholar]
- Jones T, Cumberbatch K (2018) Sign language in dental education-A new nexus. Eur J Dent Educ. 22(3):143-150.
[Crossref] [Google Scholar]
- Kumar RS, Deshpande AP, Ankola AV, Sankeshwari RM, Hampiholi V, et al. (2022) Impact of the visual performance reinforcement technique on oral hygiene knowledge and practices, gingival health, and plaque control in hearing-and speech-impaired adolescents: A randomized controlled trial. Children. 9(12):1905.
[Crossref] [Google Scholar]
- Fageeh HN, Mansoor MA (2020) The effectiveness of oral hygiene instructions in sign language among hearing impaired adults in Saudi Arabia. Spec Care Dent. 40(1):41-48.
[Crossref] [Google Scholar]
- Lees A, Rock WP (2000) A comparison between written, verbal, and videotape oral hygiene instruction for patients with fixed appliances. J Orthod. 27(4):323-328.
[Crossref] [Google Scholar]
- Moreland CJ, Ruffin CV, Morris MA, McKee M (2021) Unmasked: How the COVID-19 pandemic exacerbates disparities for people with communication-based disabilities. J Hosp Med. 16(3):185-188.
[Crossref] [Google Scholar]
- Barnett S (2002) Communication with deaf and hard-of-hearing people: A guide for medical education. Acad Med. 77(7):694-700.
[Crossref] [Google Scholar]
- Lock E (2003) A workshop for medical students on deafness and hearing impairments. Acad Med. 7(12):1229-1234.
[Crossref] [Google Scholar]
- Orrie S, Motsohi T (2018) Challenges experienced by healthcare workers in managing patients with hearing impairment at a primary health care setting: A descriptive case study. S Afr Fam Pract. 60(6):207-211.
[Crossref] [Google Scholar]
- Richardson KJ (2014) Deaf culture: Competencies and best practices. Nurse Pract. 39(5):20-28.
[Crossref] [Google Scholar]
- Suhani, RD, Suhani MF, Muntean A, Mesaros M, Badea ME (2015) Ethical dilemmas concerning the dental treatment of patients with hearing impairment. Rev Rom Bioet 13(3):1-12.
[Google Scholar]
- Moreland CJ, Meeks LM, Nahid M, Panzer K, Fancher TL (2022) Exploring accommodations along the education to employment pathway for deaf and hard of hearing healthcare professionals. BMC Med Educ. 22(1):1-9.
[Crossref] [Google Scholar]
- Baldridge DC, Kulkarni M (2017) The shaping of sustainable careers post hearing loss: Toward greater understanding of adult onset disability, disability identity, and career transitions. Hum Relat. 70(10):1217-1236.
[Crossref] [Google Scholar]
- Cardoso AHA, Rodrigues KG, Bachion MM (2006) Perception of persons with severe or profound deafness about the communication process during health care. Rev Lat Am Enferm. 14(4):553-560.
[Crossref] [Google Scholar]
- Moreland CJ, Latimore D, Sen A, Arato N, Zazove P (2013) Deafness among physicians and trainees: A national survey. Acad Med. 88(2):224-232.
[Crossref] [Google Scholar]
- McKee MM, Smith S, Barnett S, Pearson TA (2013) Commentary: What are the benefits of training deaf and hard-of-hearing doctors? Acad Med. 88(2):158-161.
[Crossref] [Google Scholar]
- Riddell S, Weedon E (2014) Disabled students in higher education: Discourses of disability and the negotiation of identity. Int J Educ Res. 63:38-46.
[Crossref] [Google Scholar]
- Punch R, Hyde M, Creed PA (2004) Issues in the school-to-work transition of hard of hearing adolescents. Am Ann Deaf. 149(1):28-38.
[Crossref] [Google Scholar]
- Curry RH, Meeks LM, Iezzoni LI (2020) Beyond technical standards: A competency-based framework for access and inclusion in medical education. Acad Med. 95:S109-S112.
[Crossref] [Google Scholar]
- Argenyi M (2016) Technical standards and deaf and hard of hearing medical school applicants and students: Interrogating sensory capacity and practice capacity. AMA J Ethics. 18(10):1050-1059.
[Crossref] [Google Scholar]
- Myers J, John AB, Kimball S, Fruits T (2016) Prevalence of tinnitus and noise-induced hearing loss in dentists. Noise Health 18(85):347-354.
[Crossref] [Google Scholar]
- Maheady D (2004) Positions Wanted: Nurses with Disabilities: Barriers to employment remain despite the nursing shortage. Am J Nurs. 104:13.
[Google Scholar]
- Punch R, Hyde M, Power D (2007) Career and workplace experiences of Australian university graduates who are deaf or hard of hearing. J Deaf Stud Deaf Edu. 12(4):504-517.
[Crossref] [Google Scholar]
- Meeks LM, Plegue M, Swenor BK, Moreland CJ, Jain S, et al. (2021) The performance and trajectory of medical students with disabilities: Results from the pathways project. Acad Med. 96(11S):S209-S210.
[Crossref] [Google Scholar]
- Cawthon SW, Schoffstall SJ, Garberoglio CL (2014) How ready are postsecondary institutions for students who are d/Deaf or hard-of-hearing? Educ Policy Anal Arch. 22:1-21.
[Crossref] [Google Scholar]
- Sternberg RJ, Bonney CR, Gabora L, Merrifield M (2012) WICS: A model for college and university admissions. Educ Psychol. 47(1):30-41.
[Crossref] [Google Scholar]
- Abes ES, Wallace MM (2018) "People see me, but they don't see me": An intersectional study of college students with physical disabilities. J Coll Student Dev. 59(5):545-562.
[Crossref] [Google Scholar]
- Evans NJ, Broido EM, Brown KR, Wilke AK (2017) Disability in higher education: A social justice approach. San Francisco: Jossey-Bass. ISBN:978-1118018224.
- Gilmore M, Sturgeon A, Thomson C, Bell D, Ryan S, et al. (2019) Changing medical students' attitudes to and knowledge of deafness: A mixed methods study. BMC Med Educ. 19(1):1-7.
[Crossref] [Google Scholar]
- Greene SJ, Scott JA (2021) Promoting cultural awareness, professionalism, and communication skills in medicine through anatomy: The Deaf culture session. Clin Anat. 34(6):899-909.
[Crossref] [Google Scholar]
Citation: Phelan G, Ayers E (2023) Deaf Dentists Diversifying Healthcare: Stories of Struggle and Success through a Comparative Case Report. J Healthc Commun. 8:8047.
Copyright: © 2023 Phelan G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.