Research Article - (2023) Volume 8, Issue 3
Received: 08-Aug-2023, Manuscript No. IPJTAC-23-17892; Editor assigned: 11-Aug-2023, Pre QC No. IPJTAC-23-17892 (PQ); Reviewed: 25-Aug-2023, QC No. IPJTAC-23-17892; Revised: 28-Sep-2023, Manuscript No. IPJTAC-23-17892 (R); Published: 26-Oct-2023, DOI: 10.36648/2476-2105-8.03.22
Background: This study aims to establish the benefits of using chest tubes with negative pleural suction against trapped water in patients with penetrating or blunt chest trauma who underwent tube thoracostomy, in terms of the incidence of complications, such as persistent air leak, clotted hemothorax and duration of stay.
Methods: Patients who underwent tube thoracostomy because of traumatic pneumothorax, hemothorax or hemopneumothorax were randomly assigned into one of two groups: In group A, the chest tube was connected to a negative suction; in group B, no suction was connected.
Results: About 80 patients were included, 40 in the group with suction and 40 in the group without suction. There were some differences in the demographic characteristics of each group. There were some differences between the groups in terms of hospital stay (p=0.410), duration of airleak (p=0.502) and complications (p=0.607). However, the probability of air leak presence in time was greater for the group A patients with negative suction versus the group B patients.
Conclusion: The use of negative pleural suction did not demonstrate advantages over the chest drainage system without suction in patients with uncomplicated traumatic pneumothorax, hemothorax or hemopneumothorax, but the risk of surgical emphysema decrease with the use of negative pleural suction.
Thoracostomy; Traumatic pneumothorax; Hemopneumothorax; Hemothorax
Trauma is the leading cause of death in the first four decades of life and are mostly caused by traffic accidents. Thoracic trauma might lead to severe consequences, even though less than 50% of them required a surgical revision. Thoracic trauma can be divided in blunt or penetrating, according to the presence of open wound in the chest. Blunt trauma is the most frequent type of chest trauma with or without rib fractures that might be associated with haemothorax, pneumothorax or haemopneumothorax that are the most typical lesions or laceration [1].
Chest tubes are used to reestablish negative intrathoracic pressure after disruption of the pleural space. Chest tube positioning is considered necessary in case of a pleural disruption with pneumothorax; intrapleural bleeding causing haemothorax; or in case of pneumo-haemothorax.
All of the previous made us interesting to examine the effect of water seal alone of chest tube in one groups of trauma patients and the effect of both water seal and suction in other group. We think that power of suction will give the patient better results with less complications and excellent immediate relief with rapid return to normal life [2].
This work was conducted in cardiothoracic surgery department, Assiut university heart hospital. It represents a prospective cohort study of patients admitted to our hospital from 1st Oct 2020 to 31th Dec 2022 who had chest trauma that need a chest tube insertion they were divided into two groups.
• Group A: Chest tube with connection to suction
• Group B: Chest tube only
About 80 patients were included, 40 in the group with suction and 40 in the group without suction. There were some differences in the demographic characteristics of each group. There were some differences between the groups in terms of hospital stay (p=0.410), duration of airleak (p=0.502) and complications (p=0.607). However, the probability of air leak presence in time was greater for the group A patients with negative suction versus the group B patients [3].
Patients present with pneumothorax, hemothorax, pneumohemothorax all including in this study and all ages available with no restriction. Patients who required mechanical ventilation or emergency surgery (thoracotomy or thoracoscopy) either at the time of admission to the institution or immediately after the tube thoracostomy, patients who had histories of thoracic procedures or chronic pulmonary diseases (chronic obstructive pulmonary disease, diffuse interstitial lung disease) and patients with multiple injuries with severe Traumatic Brain Injury (TBI) and glasgow coma scale score less than 8 of 15 were excluded [4].
Preoperative Management
All patients who underwent negative pleural suction gave written informed consent for performing the procedure and those refused were excluded from the study.
Intervention
Positioning:
• Bump under the back with arm over the head and out of the procedural field.
• The chest should be as flat as possible or gently flexed to allow for maximum opening of the spaces between the ribs.
The group of surgeons on shift performed the procedure, which was conducted under local anesthesia infused with 2% lidocaine in the fourth or fifth intercostal space on the medial axillary line. Subsequently, a 1.5 cm incision was made and was dissected until access to the pleural space was achieved.
During the study, the collection system for group A patients was connected to a 20 cm H2O wall continuous negative suction system, which was interrupted only by the change of system or the movement of the patient to the bathroom.
All patients received scheduled opioid analgesia and reinforcement analgesia was administered as necessary. A respiratory incentive was provided to patients for performing exercises each hour and the nursing staff was instructed to prompteach patient to use the device. A confirmatory chest xray was taken within 24 hours after the tube thoracostomy to evaluatethe hemothorax evacuation and pulmonary reexpansion. Radiologic checks, ultrasound study or tomographic study was conducted according to the criteria of the surgical group in charge of the patient [5].
Information related to the patient’s diagnosis, the nature of the trauma, associated pathologies and personal history was collected. The presence or absence of an alveolopleural fistula and the type of fistula according to the qualitative scale (continuous, inspiratory, expiratory, forced expiratory or without fistula) and the liquid drainage and its characteristics (blood, serohematic, watery, other) were recorded on a daily basis.
Postprocedural complications and the additional need for interventions, such as a new tube thoracostomy, thoracoscopy or thoracotomy, were documented. An external evaluator not related to the patient’s management collected the data concurrently.
The chest tube remained for a minimum of 24 hours. For his or her withdrawal, the patient had to be without dyspnea or respiratory symptoms had to show resolution of the pneumothorax and/or hemothorax upon x-ray evaluation, had to have a serohematic drainage smaller than 50 mL per 24 hrs.
Outcomes: The main study outcome was length of hospitalization. The secondary outcomes measured were persistence of alveolopleural fistula, coagulated hemothorax, empyema, recurrent pneumothorax and need for additional surgeries (new chest tube, thoracostomy or thoracotomy) [6].
Statistical analysis: The sample size calculation was conducted based on the difference between average lengths of hospitalization. Assuming an average difference of 2 days of hospitalization in the two groups with an SD of 3 days and about 40 patients were required for each group. Data were collected in master sheath then entered in excel sheath (MSEXCEL 2016). All analyses were performed with sigma stat statistical software (version 3.5, Systat software inc.).
Data were presented as frequencies, medians with ranges or means ± Standard Deviation (SD) as appropriate.
About 80 patients were included, 40 in the group with suction and 40 in the group without suction. There were some differences in the demographic characteristics of each group. There were some differences between the groups in terms of hospital stay (p=0.410), duration of airleak (p=0.502) and complications (p=0.607). However, the probability of air leak presence in time was greater for the group A patients with negative suction versus the group B patients (Tables 1 and 2) [7].
| Variables | Group A | Group B | |||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Sex | Male | 35 | 87.5 | 32 | 80 |
| Female | 5 | 12.5 | 8 | 20 | |
| Age | (18-20 years) | 9 | 22.5 | 11 | 27.5 |
| (21-60 years) | 27 | 67.5 | 27 | 67.5 | |
| (more than 60 years) | 4 | 10 | 2 | 5 | |
Table 1: Comparison between group A and B as regard demographic data.
| Variables | Group A (n=40) | Group B (n=40) | P-value |
|---|---|---|---|
| Mean ± SD | 35.87 ± 15.13 | 34.35 ± 13.67 | 0.638 |
| Range | 18.0-63.0 | 18.0-64.0 |
Table 2: Mean age of the studied patients.
Mean age of patients in the group A was 35.87, while that of the group B was 34.35. Both groups showed a male dominance by 87.8% in group A, while group B had 80%. The age range (21-60 years) is the most common in both groups that represent about (67.5%), but the patients of age range more than 60 years are the lowest number in our study. We find, in this study, that smoking is one of the risk factor that presents in most of patients, in group A about (57.7%) and in group B about (52.5%) [8]. Even though the risk of complications and long hospital stay are more with patients in active smoking (Figure 1).
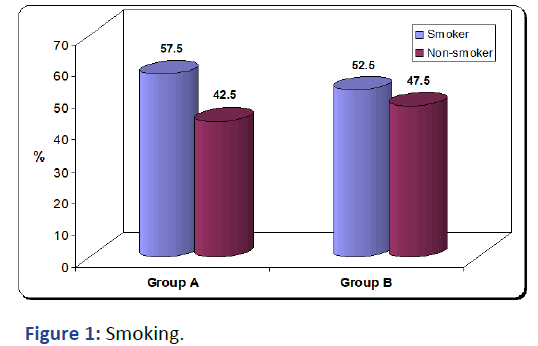
Figure 1: Smoking.
In group A patients, we use additive force presenting in negative pleural suction with under water seal of chest tube, we hope to provide rapid improvement and reduce hospital stay.
At the end of the study, we find that the period of hospital stay is more in group A about (3.85 days) in comparison to group B about (3 days). So, the use of negative pleural suction did not add advantage and so on not reduce the period of hospital stay (Table 3).
| Hospital stay (days) | Group A (n=40) | Group B (n=40) | P-value |
|---|---|---|---|
| Mean ± SD | 3.85 ± 0.83 | 3.00 ± 0.75 | 0.41 |
| Range | 3.0-6.0 | 2.0-4.0 |
Table 3: Hospital stay.
One of the most presentation of chest trauma patients is pneumothorax or hemopneumothorax and after chest tube is inserted, we can observe degree and duration of airleak. Number of patients that has airleak is more in group B about (22 persons) but, in group A about (19 persons). After we used negative suction as in group A, the duration of airleak was longer in group A about (2.11 days), but in group B with no suction about (1.27 days) (Table 4) [9].
| Duration of air leak (days) | Group A (n=40) | Group B (n=40) | P-value |
|---|---|---|---|
| Mean ± SD | 2.11 ± 0.32 | 1.27 ± 0.46 | 0.000* |
| Range | 2.0-3.0 | 1.0-2.0 |
Table 4: Duration of air leak.
Some patients after chest trauma that causing pneumothorax or hemopneumothorax, they may get surgical emphysema as one of common complication after chest tube insertion. With using negative pleural suction as in group A, we find an advantage as this lead to reduce risk of surgical emphysema in group A about (25% of cases) as signi icant value (P-value 0.607) but, this risk is more occurance in group B about (30%of cases) (Table 5) [10].
| Complications | Group A (n=40) | Group B (n=40) | P-value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Yes | 10 | 25% | 12 | 30% | 0.607 |
| No | 30 | 75% | 28 | 70% | |
Table 5: Complications.
Thoracic trauma represents one of the greatest challenges in the comprehensive management of the multi trauma patient for the trauma surgeon owing to the high morbidity and mortality generated by its complications and high health care costs. Tube thoracostomy plays a fundamental role in the management of the majority of these types of patients. The utility of adding pleural negative suction to the collection system that is being used according to each surgeon’s criterion is still unclear. The theory is that pleural negative suction promotes faster air leak closure and hemothorax drainage.
In our study, the use of negative pleural suction did not show any advantage over the chest tube with under water seal only, in terms of decreased hospital stay. We find that the period of hospital stay is more in group A about (3.85 days) in comparison to group B about (3 days) [11].
So, the use of negative pleural suction did not add advantage and so on not reduce the period of hospital stay. In group A, we find an advantage as this lead to reduce risk of surgical emphysema in group A about (75% of cases) but, this risk is more occurance in group B about (30% of cases). After we used negative suction as in group A, the duration of airleak was longer in group A about (2.11 days), but in group B with no suction about (1.27 days) and this is a significant value (Pvalue 0.000*) in our study [12].
Other authors reported similar results including Ayed et al., who showed that the incidence of prolonged air leak was greater in patients with negative suction (p=0.03), as were the average chest tube duration and hospital stay. In another randomized controlled trial conducted by Marshall et al., the use of suction led to an earlier resolution of air fistulas and a shorter chest tube duration and hospital stay. In our study, the use of negative suction was not shown to diminish air leak closure time. We believe that this occurrence is primarily caused by air leaks in trauma patients being particularly low and the air absorption rate using the chest tube with under water seal only was sufficient for evacuating the pneumothorax.
We decided to use the prolonged air leak definition of 7 days proposed by Brunelli et al. It is indisputable that the type of patients included in these studies is different from the trauma patient chiefly because of age, pulmonary reserve, comorbidities and the type of surgery to which they were submitted. In our study, no patients experienced a persistent air leak. However, because of the nature of the trauma, a large majority of our cases presented with pulmonary parenchymal wounds as opposed to patients with pulmonary resections, which include bronchial leaks. This difference likely explains why our patients are also prone to more rapid closure of the leak.
In a study conducted by Davis et al., in 80 patients with tube thoracostomy secondary to chest trauma, the use of negative pleural suction reduced chest tube use time (72.2 hours vs. 92.5 hours, p=0.013) and reduced the time between the resolution of the air leak and the tube withdrawal (25.2 hours vs. 35.6 hours, p=0.034) [13].
The use of negative pleural suction did not demonstrate advantages over the chest drainage system without suction in patients with uncomplicated traumatic pneumothorax, hemothorax or hemopneumothorax, but the risk of surgical emphysema decrease with the use of negative pleural suction. The conclusions of this study are only applicable to patients whose only trauma treatment is the application of a tube thoracostomy. Most subjects in this study had penetrating trauma; more trials with blunt trauma patients are required to generate further conclusions.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Nabil AM, Abdelatef MK, Abdalrazik MH, Alassal YA, Mekkawy AMA (2023) Chest Tube Drainage with under Water Seal versus Addition of Negative Pleural Suction in Chest Trauma Patients. Trauma Acute Care. 8:22.
Copyright: © 2023 Nabil AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.