Keywords
Bone Mineral Density; Osteoporosis; HIV; PLHA
Introduction
Anti-Retroviral Therapy (ART) has significantly decreased the mortality and morbidity associated with HIV/AIDS. Now the attention has shifted to previously less inadvertent conditions such as increased cardiovascular risk, osteoporosis and malignancy. The awareness of bone health in India is lacking among the physicians and perhaps is not a priority for doctors those who are treating People Living with HIV/AIDS (PLHA).
Osteoporosis is disease of bone where compositional and architectural changes occur in the bone tissue arrangement leading to weakening of the skeleton resulting in increased probabilities of fragility fracture [1]. World Health Organization (WHO) has classified this low density of bone as osteoporosis or osteopenia based on bone densitometry. Osteoporosis is defined when density is below -2.5 times the standard deviation and osteopenia when the result is between -1 and -2.5 times the standard deviation [2].
Vitamin-D deficiency is rampant in India and is a major risk factor contributing towards low bone density even in people living with HIV/AIDS. This study was conducted at tertiary care referral center to assess the bone health in PLHA. As osteopenia/osteoporosis can lead to the fracture, there may be further increase the morbidity and cost of treatment. Thus it is imperative that physicians take care of HIV should aware of its effect on bone health.
Aims and Objectives
To study the bone mineral density and assess the risk factors of developing osteopenia/osteoporosis in patients of HIV/AIDS.
Materials and Methods
The study design was case control study conducted in a tertiary care center in heart of Delhi, India. The hospital caters to all sectors of society hence the study population is reflecting of society. The study was conducted over a period of 15 months (March 2013 to June 2014). People living with HIV/AIDS, aged above 18 years, diagnosed by two different ELISA according to WHO strategy-II [3], were included in the study after obtaining an informed consent. Patients were excluded if they were: pregnant, known cases of bone diseases, or on calcium supplements/bisphosphonates/tereparatide/denosumab for >3 months, diagnosed with psychiatric illness, diagnosed to have hypothyroidism, pregnant. Healthy consenting subjects who did not give any significant medical history were taken as control. For control population vitamin D (25(OH) Vitamin D) and bone densitometry were done beside other relevant history.
Consent was taken from all patients and also from control group for the study. Detailed history was taken regarding HIV related and traditional risk factors for developing osteopenia/osteoporosis.
Risk factors related to HIV infection are duration of HIV infection, previous CD4+ count and viral load (in already diagnosed cases) and tenofovir based anti-retroviral regimen.
Traditional risk factors are inadequate sun exposure, insufficient physical activity, diet regarding calcium intake, presence of previous fractures (fragile/traumatic), smoking and alcoholism.
All subjects were examined and weights were recorded by electronic weighing machine and height was measured by stadiometer. Body mass index was calculated by using formula (Quetlet’s index): weight (kg)/height(m)2. Musculoskeletal examination was done which includes examination of spine (kyphoscoliosis, ankylosis, etc.), gait and stance.
We investigated the subjects with CD4+ T lymphocyte count, HIV viral load, vitamin D levels in the serum in the form of 25(OH) Vitamin D and Bone Mineral Density (BMD) with DEXA scan. We measured the fracture risk in both groups with FRAX tool [4].
Vitamin D level (25 (OH)D) was classified as given in Table 1.
| Vitamin D (25(OH)) level (ng/mL) |
Interpretation |
| < 20 |
Deficient |
| 21-29 |
Insufficient |
| >30 |
Sufficient |
| >150 |
Toxic |
Table 1: Reference range values for 25(OH) Vitamin D [5].
WHO classification of BMD was done as given in Table 2.
| BMD-T score |
Classification |
| >-1 |
Normal |
| -1 to -2.5 |
Osteopenia |
| At or below -2.5 |
Osteoporosis |
| Below -2.5 plus fragility fractures |
Severe osteoporosis |
Table 2: WHO classification of BMD according to the T-score [2].
Definitions used in our study:
1) Hypovitaminosis D: If the level of 25 (OH) vitamin D is <20 ng/mL it is defined as deficient and 21-29 ng/mL is defined as insufficient state [5].
2) Adequate exercise: Moderate activity of at least 150 h per week [6].
3) Adequate sun exposure: Early morning exposure to sun light for 30 min daily [7].
Statistical Analysis
Statistical testing was conducted with the Statistical Package for the Social Science system (SPSS) version 17.0. Continuous variables were expressed as mean ± SD while categorical variables as frequencies and percentages. Unpaired t-test and Mann-Whitney U-test were used for continuous while either Chi-squared test or Fisher’s exact test was used for categorical variables. For all statistical tests, p value less than 0.05 was taken to indicate a significant difference.
Observation and Results
We had 60 participants each in case and control group after applying inclusion criteria. Both the groups were matched for age. Similarly, no statistical difference in sex distribution, height, weight or (Body Mass Index) BMI was observed between both groups (Tables 3a and 3b).
| |
Patients |
Control |
| Age |
39.82 ± 11.68 years |
41.08 ± 11.52 years |
| Height |
165 ± 6.766 cms |
162.98 ± 6.207 cms |
| Weight |
67.897 ± 15.799 Kg |
64.072 ± 11.508 Kg |
| BMI |
24.62 ± 4.72 Kg/m2 |
24.03 ± 3.98 Kg/m2 |
| Sex |
Male-61.7%, |
Male-48.3%, |
| Female-38.3% |
Female-51.7% |
Table 3a: Demographic details of the population.
| Age (yr) |
Cases: n(%) |
Controls: n(%) |
P value |
| Normal |
Osteopenia |
Osteoporosis |
Normal |
Osteopenia |
Osteoporosis |
| 18-30 |
2 (14.3%) |
6 (42.9%) |
6 (42.9%) |
7 (77.8%) |
1 (11.1%) |
1 (11.1%) |
0.01 |
| 31-50 |
4 (12.5%) |
17 (53.1%) |
11 (34.4%) |
22 (64.7%) |
12 (35.3%) |
0 (0%) |
0 |
| ≥51 |
1 (7.1%) |
6 (42.9%) |
7 (50%) |
12 (70.6%) |
5 (29.4%) |
0 (0%) |
0 |
| Mean |
39.82±11.68 yr |
41.08±11.52 yr |
0.89 |
Table 3b: Age distribution among cases and control group.
Classification according to Bone Mineral Density (BMD)
Among cases 53 (88.3%) persons had low bone mineral density. In that 29 patients (48.3%) had osteopenia, 24 subjects (40%) had osteoporosis and 7 (11.7%) had normal BMD. Among control group 19 cases (31.7%) had low BMD, in which 18 had osteopenia and 1 had osteoporosis. Low bone mineral density was more prevalent in PLHA than control (P value: 0.000). Patients with HIV/ AIDS had a 16.26 times higher risk of having low bone density than that of normal population (Odds ratio).
Evaluation of traditional risk factors
There was no statistical difference found between the two groups in terms of physical activity (p=0.098), sun exposure (p=0.196), calcium intake (p=0.273), history of alcohol consumption (p=0.853), history of smoking (p=0.852). BMD among nonsmokers (p=0.00) in both the groups and history of fractures (p=0.013) were statistically significant between both the groups (Tables 4 and 5).
| |
Case |
Control |
P value |
| Inadequate |
Adequate |
Inadequate |
Adequate |
| Physical activity |
63.30% |
36.70% |
48.30% |
51.70% |
0.098 |
| Sun exposure |
48.30% |
51.70% |
36.70% |
63.30% |
0.196 |
| Calcium intake |
45% |
55% |
55% |
45% |
0.273 |
Table 4: Evaluation of traditional risk factors.
| |
Case |
Control |
P value |
| History of smoking |
40% |
38.30% |
0.852 |
| History of alcohol |
41.70% |
43.30% |
0.853 |
| History of fracture |
11.70% |
NIL |
0.013 |
| Vitamin D |
21.363±17.7826 U/µL |
26.238±20.1647 U/µL |
0.163 |
| FRAX score |
2.387±3.5805% |
0.902±2.3709% |
0 |
| (Range 0-19%) |
(Range 0-16%) |
Table 5: Evaluation of traditional risk factors.
Evaluation of risk factors related to HIV infection
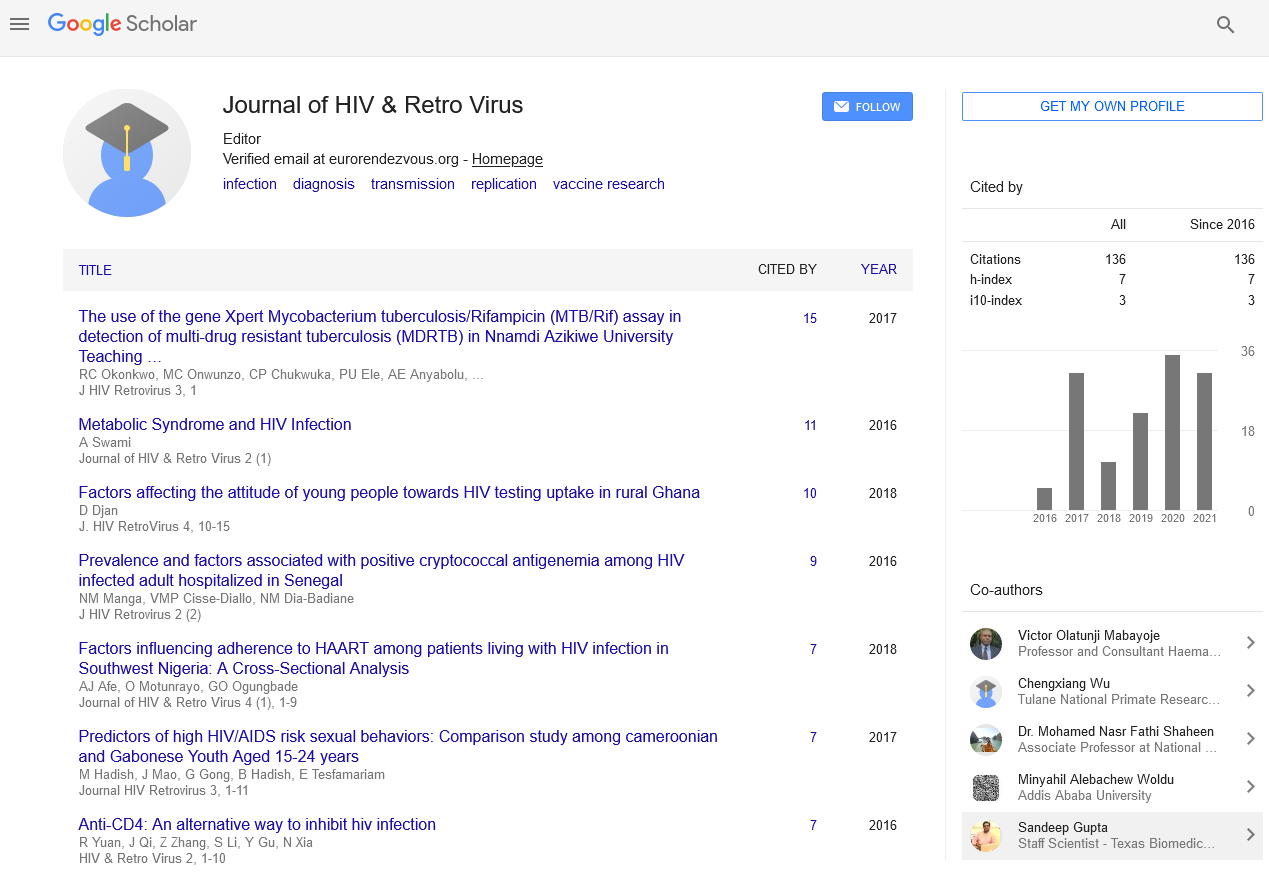
No HIV associated risk factor was found to be statistically significant. Duration of HIV infection (p=0.553), median absolute CD4 count (p=0.128) and the median viral load (p=0.743) were not significantly related to bone density. Similarly tenofovir based ART regimen (Figure 1) was also not associated significantly with bone mineral density in our study (p=0.417) (Table 6).
Figure 1: Flow diagram of the study.
| |
Normal BMD |
Osteopenia |
Osteoporosis |
P value |
| Duration of HIV |
3 months |
2 months |
3 months |
0.553 |
| HIV viral load |
115467 copies/Ml |
89100 copies/Ml |
110676.5 copies/ml |
0.743 |
| CD4 cell count |
347 cells/Ml |
194 cells/mL |
187.5 cells/Ml |
0.128 |
| Tenofovir exposure |
5 participants |
19 participants |
12 participants |
0.417 |
Table 6: Evaluation of risk factors related to HIV infection.
Vitamin D [25 (OH)] level in study and control groups
The mean vitamin D [25 (OH)] level in control population was 21.363 ± 17.7826 U/μL and in disease group it was 26.238 ± 20.1647 U/μL. The difference between both disease and control population was not statistically significant (p=0.163). Association of vitamin D deficiency with low BMD in between both case and control groups was statistically significant (p=0.00).
The FRAX score
The mean of FRAX score in study group was 2.387( ± 3.5805)%, range from 0-19%, and control population, 0% and 16% were the minimum and maximum FRAX scores respectively and 0.902( ± 2.3709)% was the mean. The difference of FRAX score between both groups was statistically significant (p=0.00).
Correlation analysis of factors influence low BMD in cases group
In our study no correlation found between traditional risk factors like age, BMI, smoking, sex, alcohol consumption, and viral load, level of CD4+ and HIV-RNA levels to low BMD in people living with HIV/AIDS (Table 7).
| Variables |
r |
p |
| Age |
0.042 |
0.75 |
| Male vs female |
-0.01 |
0.94 |
| History of smoking |
0.01 |
0.94 |
| History of alcohol use |
-0 |
0.97 |
| Vitamin D (25(OH)) level |
-0.16 |
0.22 |
| Adequate sun exposure |
0.17 |
0.19 |
| Adequate calcium intake |
-0.02 |
0.9 |
| BMI |
-0.18 |
0.18 |
| Adequate physical activity |
0.122 |
0.35 |
| Absolute CD4+ (<200 vs >200) |
-0.22 |
0.09 |
| HIV viral load (<1 lakh and >1 lakh) |
-0.06 |
0.63 |
Table 7: Correlation analysis of factors influences low BMD in HIV
patients.
Discussion
Our study has recorded a prevalence of 83.3% bone disease in HIV infected population as compared to 31.7% prevalence in healthy controls. By calculating odds ratio we could state that our HIV population had a 16.26 times more risk of developing a low BMD as compared to control population. Thus, HIV is rightly considered as a risk factor for low BMD. Several other studies have confirmed the same [8,9]. Brown et al. in a meta-analysis study estimated reduced BMD in 67% of HIV-infected individuals and 15% had osteoporosis [10]. The results were almost similar to our study. In a study conducted at Jakarta, the prevalence of reduced BMD in ARV naïve HIV-infected patients was 26.2% [7]. In another study Arnsten et al. studied middle age women with HIV infection and identified an increased prevalence of low bone density in them [11]. In a cross sectional study done by Masyeni et al., found a significant correlation between HIV infection and low bone mineral density [12]. In Pune, 536 HIV patients were observed for bone density and found that prevalence of low BMD was compared between ART naive and ART experienced patients. They found that low BMD was prevalent in 67% of ART naïve (osteopenia: 70.4%, osteoporosis: 29.6%) and in 80.4% of ART experienced patients (osteopenia: 63.4%, osteoporosis: 36.6%) (p=0.05) [13]. These results were also similar to our study, but there was no control population to compare the BMD in that study. The study also suggested a possible role played by ART in osteoporosis. Osteoporosis in a HIV infected individual is likely multifactorial. Individual risk factors like height, weight, lean body weight, dietary habits, physical activity, smoking habit, alcohol consumption, vitamin D levels, calcium levels in blood are common to the entire population irrespective of HIV status. HIV related immune activation, direct viral effects on bone, ART regime used may play a role in HIV induced BMD reduction.
Several mechanisms come into play for the development of osteoporosis in PLHA. Successful bone formation or remodeling requires a coupled osteoblast and osteoclast function. In HIV infection there is uncoupling of these two processes. This can be attributed to both direct and immune-mediated mechanisms. Direct viral effect results in osteoclast activation mediated by viral proteins like gp120, vpr and osteoblast apoptosis mediated by p55-gag. Also, high viral load has a positive correlation with RANKL (Receptor Activator of Nuclear Factor Kappa-B) which induces osteoclast formation and in turn resorption of bone. Indirectly, proinflammatory cytokines are upregulated and regulatory molecules are downregulated. Cytokines like Tumor Necrosis Factor (TNF)-α, (Interleukin) IL-6 promote osteoclastogenesis and HIV infection favours their upregulation through the PTH (Parathyroid Hormone) pathway. Interferon-γ is a physiological inhibitor of RANKL (Receptor Activator of Nuclear Factor kappa-Β ligand) signaling pathway and osteopontin is a regulator of osteoclast activity. Studies have shown decline in the levels of both the molecules in HIV infection [14-23].
ART also has a role to play in bone health. There is a generalized concept that HAART (Highly Active Anti-retroviral Therapy) decreases BMD initially, followed by stabilizing it and later on increasing BMD as a long term effect. There are several studies including some meta-analysis and the ASSERT (Adrenaline Stress Strategic Emergency Response Training) study, which support this statement [24-32]. It is hypothesized that the nephrotoxicity of Tenofovir Disoproxil Fumarate (TDF) may increase the levels of PTH and favour bone resorption. TDF causes mitochondrial dysfunction in proximal convoluted tubules by inhibiting mitochondrial DNA polymerase ϒ. This effect is not seen with Tenofovir Alafenamide (TAF). Similar arguments hold good for protease inhibitors also. But these are still hypothesis and the credibility behind these proposed mechanisms are yet to be confirmed. Several questions still remain unanswered, like role of Tenofovir Alafenamide (TAF) and newer agents like entry inhibitors and integrase inhibitors, reason for an acute fall in BMD before it stabilizes and so on. A potential role of immune reconstitution may be suggested.
Out of 60 subjects with HIV/AIDS there were 37 (61.7%) males and 23 (38.3%) females. In control group out of 60 participants there were 29 (48.3%) males and 31 (51.7%) females. In our study there was no significant difference in the prevalence of bone disease between males and females of either case or control group. Usually the rate of bone loss in men is less than that in women hence low prevalence of bone disease in men. But in a study conducted by Dravid et al. in western India also found no significant association of gender with bone disease [13]. As our study group included more males than females the results were not similar to previous studies.
The mean age in study group was 39.82 ± 11.68 years and in control group it was 41.08 ± 11.52 years. There was no difference in mean age of our study and control population. Although osteoporosis/osteopenia is usually a disease of old age, in our population this was seen in young age group (30-50 years). Thus people with HIV/AIDS were facing problem of bone disease at earlier age. Previous Indian study also reported almost similar (median age of low BMD in HIV/AIDS=38-49 year) finding [13].
Body Mass Index (BMI) was classified as underweight, normal, over weight and obesity if the values are <18.5 kg/m2, 18.5-22.9 kg/m2, 23-24.9 kg/m2 and ≥ 25 kg/m2 respectively [33]. The mean BMI was 24.62±4.72 kg/m2 in HIV patients and 24.03±3.98 kg/ m2 control population. In study group 24 out of 29 subjects and in control group 7 out of 14 subjects with high BMI were found to have osteoporosis/osteopenia. In a Korean study, a significant association was found with low BMI and low BMD in HIV patients. Similarly a recent study from India showed that lean body mass, BMI and albumin/globulin ratio were predictors of osteoporosis in HIV infected women [34]. Usually chronic HIV infection leads to poor nutrition and weight loss but in our study there was no significant difference in BMI of case and control subjects, hence the results were not similar [35].
Kujala et al. studied relation between physical activity hip osteoporosis and their results were contradictory to our findings. They observed that the baseline physical activity and future hip fracture risk were inversely related [36]. Physical activity is important modifiable risk factor for osteoporosis. In our study, 34 members in study group and 8 members in control group were found to have low BMD in association with inadequate physical activity but it was statistically insignificant. Similarly, Perazzo et al. showed that moderate to high intensity physical activity should mitigate excessive bone loss in People living with HIV/AIDS [37]. Meta-analysis has proved that physical exercise improves BMD and decreases the risk of osteoporosis [38]. This discrepancy between literature and our study might be because of our small sample size.
Smoking is also a risk factor for osteoporosis. In an Irish study by Cummins et al. found that smoking was the strongest behavioral predictor of lumbar and femoral BMD [39]. However in our study we found that positive history of smoking was present in 24 (40%) of study population and 23 (38.3%) of control population. The difference was statistically insignificant. Alcohol consumption was also not significant risk factor for osteoporosis in our study. A similar result was shown by Saitz et al. where alcohol consumption was not significantly related to osteoporosis [40].
The mean 25 (OH) vitamin D level in disease group was 21.36 ± 17.78 U/μL and in control population it was 26.238 ± 20.16 U/μL. The difference was statistically insignificant. This might be because of high prevalence of vitamin deficiency in normal Indian population. The prevalence of Vitamin D deficiency in Indian population is estimated to be 80% [41]. In contrast to our results, a study in Chille showed that Vitamin D deficiency was prevalent more on HIV infected individuals compared to healthy controls and the results were significant (p=0.04%) [42]. Vitamin D deficiency may lead to a secondary increase in parathormone levels resulting in increased bone resorption.
Out of 60 subjects of PLHA group in our study the median duration of HIV infection was 3 months, 2 months and 3 months in normal, osteopenia and osteoporosis groups respectively. And this was statistically not significant (p=0.553). Previously a study was done by Aydin et al. among 126 HIV patients, and they found significant correlation between HIV duration and prevalence of low bone mineral density [43]. This was not comparable in our study. This might be because of small sample size.
In our study, among disease group 7 out of 60 subjects with normal BMD had median absolute CD4+ count of 347 cells/μL, 29 out of 60 subjects with osteopenia had 194 cells/μL and 24 subjects with osteoporosis had 187.5 cells/μL. This difference was not significant statistically. The relationship between CD4 cell count and BMD loss is quite variable [44]. Aydin et al. found no association between CD4 cell count and osteoporosis in people living with HIV/AIDS [43]. Whereas, in a multivariable analysis, Grant et al. found that baseline CD4+ cell count had a significant association with 96-week BMD loss. Patients with baseline CD4+ <50 cells/μL suffered significant loss in BMD compared to those with CD4+ ≥ 500 cells/μL (p=0.001) [45]. Grant et al., however, could not explain the mechanism of this relationship between low CD4 count and low BMD. Dutta et al. did not find any correlation between the baseline CD4 count and osteoporosis in pre-menopausal women; however, in their study they have found that change in CD4 count is an independent predictor of osteoporosis [34]. These results were not comparable with our study. The difference might be because of variation in selection of subjects and type of study.
There was no significant association between HIV viral load and prevalence of low bone mineral density in our study. Contradicting our results, Aydin et al. and Grant et al. showed significant relation between high viral load and prevalence of low bone mineral density [43,45]. In our study in we couldn’t get the initial viral load of few subjects who were previously diagnosed and on treatment. The variation in the point of time of getting viral load among all subjects might be the reason for the lacking of significant association in our study.
In disease group 36 out of 60 subjects with HIV/AIDS were on tenofovir based regimen. Among those 27 subjects had low bone mineral density of which osteopenia was present in 19 subjects and osteoporosis was found in 12 subjects. But the difference in prevalence of low BMD between tenofovir using and not using groups was not found as significant. On the other hand role of tenofovir in osteoporosis have been evaluated and confirmed through randomized control trials which show consistent results of tenofovir increasing the chances of osteoporosis, especially in hip and spine [31,32]. A study of the Veteran Affairs Clinical Case Registry showed that cumulative exposure to tenofovir was associated with an increased risk of low bone density and incident fracture (Hazard Ratio) (HR, 1.16; 95% CI, 1.08–1.24; P=0.0001) [46]. Negredo et al. also showed role of Protease Inhibitors (PIs) in development of osteoporosis. According to his study PIs and PIs in combination with TDF had higher incidences of osteoporosis. Darunavir was significantly associated with osteoporosis in both men (HR 3.9; 95% CI 2-7.5) and women (HR 4.5; 95% CI 1.4-14.7) while atazanavir in only women population (HR 4.2; 95% CI 1.3- 14) [47]. In our study we could not retrieve the data regarding previous ART regimens they used in few subjects, hence the results were not similar to previous studies.
Gallant et al. [48] concluded that earlier initiation of ART may result in a better outcome in terms of ART associated osteoporosis. In our study we could not get the pre ART initiation CD4+ count in all patients hence the results were not significant.
In our study while history of fractures was given by 7 (11.7%) subjects (six were osteoporotic and one was osteopenic) in cases group, no one in control group had history of fracture and the difference was statistically significant. Among those seven fractures, two were fragility fractures and rest all traumatic. Osteoporotic fractures are usually fragile. Our finding i.e. more traumatic fractures might be incidental. In the HIV Outpatient Study (HOPS), age-adjusted fracture rates for HIV-infected adults were higher than rates in the general population. Fracture rate per 10000 population in HOPS was 83.2% and 35.9% in general population [49]. A Canadian case control study showed increased probability of fragility fracture in a HIV positive woman compared to HIV negative individual [50]. A Swiss cohort study showed the fracture incidence to be 1.64 per 1000 person years in HIV infected individuals. The median duration of HIV in their study was 15.4 years [51]. Similar conclusion was obtained in a systematic literature review conducted by Llha et al. where the incidence of vertebral fracture was found to be higher in HIV positive individuals [52]. All above results were similar to the findings in our study. In contrast, some data suggest a similar risk of fracture in HIV-infected and HIV-uninfected persons [53].
The mean of FRAX score in cases group was 2.387 and 0.902 in control population. The difference was statistically significant. FRAX score, exclusively based on femur neck BMD, may underestimate the fracture risk. Moreover WHO algorithm does not validate the use of spine BMD. So, it’s imperative that clinicians should make decisions based on suspicions and clinical judgment.
No correlation found between traditional risk factors like age, BMI, smoking, sex, alcohol consumption, and viral load, level of CD4+ and HIV-RNA levels to low BMD. However, our result shows a trend in CD4+ and HIV-RNA levels and low BMD. The reason of this finding might be explained by small sample size, and uneven sample distribution. Masyeni et al. [54] conducted a cross sectional study in Sanglah Hospital, Bali and found low bone density in 43.8% HIV patients and as in our study there was also no correlation between traditional risk factors and osteoporosis/ osteopenia in PLHA.
In summary, people living with HIV/AIDS are at risk of osteoporosis, osteopenia and fracture more than normal population and the risk of developing bone disease is more with young age group. Neither the traditional risk factors nor the virus related risk factors have a correlation with the lesser BMD found in PLHA. Vitamin D deficiency was not significantly associated with low BMD among HIV population in our study but considering its magnitude in Indian population, it should be regarded as an important risk factor for bone diseases in both HIV positive and negative population. Tenofovir is one of the front line drugs in majority of guidelines in ART. In view of widely prevalent vitamin D deficiency and osteoporotic effect of tenofovir we would suggest substitution of TDF with TAF. This may benefit the patient both in terms of renal and bone health.
Our study had some contradictory results compared to previous studies in the literature. This may be because of differences in the selected population, selection criteria and also the limitations of our study like small sample size, lack of follow up, inability to calculate risk ratio. However, we have applied strict inclusion and exclusion criteria in our study and it is one of its kinds in the Indian scenario. Awareness of bone health in HIV is still lacking among the physicians dealing with HIV/AIDS patients. Our study emphasizes the need for regular screening of these patients for bone diseases and also for empirical vitamin D and calcium supplementation for these patients. We recommend largerpopulation based multi-centric, longitudinal studies for better conclusions.
References
- Peck WA (1993) Consensus Development Conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94: 646-50.
- Bruera D, Luna N, David DO, Bergoglio LM, Zamudio J (2003) Decreased bone mineral density in HIV-infected patients is independent of antiretroviral therapy. AIDS 17: 1917-23.
- https://www.who.int/hiv/pub/surveillance/hiv_testing_technologies_surveilla e.pdf.
- https://www.shef.ac.uk/FRAX/tool.jsp.
- Chel V, Wijnhoven HA, Smit JH, Ooms M, Lips P (2008) Efficacy of different doses and time intervals of oral vitamin D supplementation with or without calcium in elderly nursing home residents. Osteoporosis Int 19: 663-71.
- Tendon N, Marwaha RK, Kalra S, Gupta N, Dudha A (2003) Bone mineral parameters in healthy young Indian adults with optimal vitamin D availability. Natl Med J India 16: 298-302.
- Setyohadi B, Mulansari NA, Sukamana N (2009) Reduced bone mineral density and serum C-telopeptide concentration in Cipto Mangunkusumo Hospital. Acta Med Indones - Indones J Intern Med 41: 191-4.
- Corcoran C, Grinspoon S (1999) Treatments for wasting in patients with the acquired immunodeficiency syndrome. N Engl J Med 340: 1740-50.
- Brown T, Grace A, McComsey (2006) Osteopenia and osteoporosis in patients with HIV: A review of current concepts. Curr Inf Dis Rep 8: 162-70.
- Brown TT, Qaqish RB (2006) Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 20: 2165-74.
- Arnsten JH, Freeman R, Howard AA, Floris-Moore M, Santoro N (2006) HIV infection and bone mineral density in middle-aged women. Clin Infect Dis 42: 1014-20.
- Masyeni S, Utama S, Somia A, Widiana R, Merati TP (2013) Factors influencing bone mineral density in ARV-naive patients at Sanglah Hospital, Bali. Acta Med Indones 45: 175-9.
- Dravid A, Kulkarni M, Borkar A, Dhande S (2014) Prevalence of low bone mineral density among HIV patients on long-term suppressive antiretroviral therapy in resource limited setting of western India. J Int AIDS Soc 17: 19567.
- Yin M (2012) Vitamin D, bone, and HIV infection. Top Antivir Med 20: 168-72.
- Huang JC, Sakata T, Pfleger LL, Bencsik M, Halloran BP, et al. (2004) PTH differentially regulates expression of RANKL and OPG. J Bone Miner Res 19: 235-44.
- Fakruddin JM, Laurence J (2003) HIV envelope gp120 mediated regulation of osteoclastogenesis via receptor activator of nuclear factor kappa B ligand (RANKL) secretion and its modulation by certain HIV protease inhibitors through interferon-gamma/RANKL cross-talk. J Biol Chem 278: 48251-58.
- Fakruddin JM, Laurence J (2004) Interactions among human immunodeficiency virus (HIV)-1, interferon-gamma and receptor of activated NF-kappa B ligand (RANKL): implications for HIV pathogenesis. Clin Exp Immunol 137: 538-45.
- Gibellini D, Borderi M, DE Crignis E, Cicola R, Vescini F, et al. (2007) RANKL/OPG/TRAIL plasma levels and bone mass loss evaluation in antiretroviral naïve HIV-1 positive men. J Med Virol 79: 1446-54.
- Gazzola L, Bellistri GM, Tincati C, Ierardi V, Savoldi A, et al. (2013) Association between peripheral T-Lymphocyte activation and impaired bone mineral density in HIV-infected patients. J Transl Med 11: 51.
- Josien R, Wong BR, LI HL, Steinman RM, Choi YT (1999) A TNF family member is differentially expressed on T cell subsets and induces cytokine production in dendritic cells. J Immunol 162: 2562-68.
- Barkhordarian A, Ajaj R, Ramchandani MH, Demerjian G, Cayabyab R, et al. (2011) Osteoimmunopathology in HIV/AIDS: a translational evidence-based perspective. Patholog Res Int 2011: 359242.
- Malizia AP, Cotter E, Chew N, Powderly WG, Doran PP (2007) HIV protease inhibitors selectively induce gene expression alterations associated with reduced calcium deposition in primary human osteoblasts. AIDS Res Hum Retroviruses 23: 243-50.
- Vikulina T, Fan X, Yamaguchi M, Roser-Page S, Zayzafoon M, et al. (2010) Alterations in the immuno-skeletal interface drive bone destruction in HIV-1 transgenic rats. Proc Natl Acad Sci USA 107: 13848-53.
- Brown TT, Qaqish RB (2006) Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 20: 2165-74.
- Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P (2012) Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviralvagents. AIDS 26: 825-31.
- Madeddu G, Spanu A, Solinas P, Calia GM, Lovigu C, et al. (2004) Bone mass loss and vitamin D metabolism impairment in HIV patients receiving highly active antiretroviral therapy. Q J Nucl Med Mol Imaging 48: 39-48.
- Heath KV, Montaner JS, Bondy G, Singer J, O’Shaughnessy MV, et al. (2003) Emerging drug toxicities of highly active antiretroviral therapy for human immunodeficiency virus (HIV) infection. Curr Drug Targets 4: 13-22.
- Schafer JJ, Manlangit K, Squires KE (2013) Bone health and human immunodeficiency virus infection. Pharmacotherapy 33: 665-82.
- Dornadula G, Nunnari G, Vanella M, Roman J, Babinchak T, et al. (2001) Human immunodeficiency virus type 1-infected persons with residual disease and virus reservoirs on suppressive highly active antiretroviral therapy can be stratified into relevant virologic and immunologic subgroups. J Infect Dis 183: 1682-87.
- Horizon AA, Joseph RJ, Liao Q, Ross ST, Pakes GE (2011) Characteristics of foot fractures in HIV-infected patients previously treated with tenofovir versus non-tenofovir-containing highly active antiretroviral therapy. HIV AIDS (Auckl) 3: 53-9.
- Stellbrink HJ, Orkin C, Arribas JR, Compston J, Gerstoft J, et al. (2010) Comparison of changes in bone density and turnover with abacavir-lamivudine versus tenofovir-emtricitabine in HIV-infected adults: 48 week results from the ASSERT study. Clin Infect Dis 51: 963-72.
- McComsey GA, Kitch D, Daar ES, Tierney C, Jahed NC, et al. (2011) Bone mineral density and fractures in antiretroviral-naive persons randomized to receive abacavirlamivudine or tenofovir disoproxil fumarate-emtricitabine along with efavirenz or atazanavir-ritonavir: Aids Clinical Trials Group A5224s, a substudy of ACTG A5202. J Infect Dis 203: 1791-801.
- Raatikainen K, Heiskanen N, Heinonen S (2006) Transition from overweight to obesity worsens pregnancy outcome in a BMI-dependent manner. Obesity (Silver Spring) 14: 165-71.
- Dutta D, Garga UC, Gadpayle AK, Bansal R, Anand A, et al. (2018) Occurrence and predictors of osteoporosis and impact of body composition alteration on bone mineral health in asymptomatic pre-menopausal women with HIV infection. Indian J Med Res 147: 484-95.
- Choe PG, Choi HJ, Kim NH, Park WB, Song KH, et al. (2014) High prevalence of low bone mass and associated factors in Korean HIV-positive male patients undergoing antiretroviral therapy. J Int AIDS Soc 17: 18773.
- Kujala UM, Kaprio J, Kannus P, Sarna S, Koskenvuo M (2000) Physical activity and osteoporotic hip fracture risk in men. Arch Intern Med 160: 705-8.
- Perazzo JD, Webel AR, Alam SMK, Sattar A, McComsey GA (2018) Relationships Between Physical Activity and Bone Density in People Living with HIV: Results from the SATURN-HIV Study. J Assoc Nurses AIDS Care 29: 528-37.
- Howe TE, Shea B, Dawson LJ, Downie F, Murray A, et al. (2011) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev 7: 21-5.
- Cummins NM, Jakeman PM, Sestak I, Murphy N, Carroll P (2013) The effect of behavioral risk factors on osteoporosis in Irish women. Ir J Med Sci 182: 97-105.
- Saitz R, Mesic A, Ventura AS, Winter MR, Heeren TC, et al. (2018) Alcohol Consumption and Bone Mineral Density in People with HIV and Substance Use Disorder: A Prospective Cohort Study. Alcohol Clin Exp Res 42: 1518-29.
- Beloyartseva M, Mithal A, Kaur P, Kalra S, Baruah MP, et al. (2012) Widespread vitamin D deficiency among Indian health care professionals. Arch Osteoporos 7: 187-92.
- Ceballos ME, Carvajal C, Jaramillo J, Dominguez A, González G (2018) Vitamin D and Bone Mineral Density in HIV Newly Diagnosed Therapy-Naive Patients Without Any Secondary Causes of Osteoporosis. Calcif Tissue Int pp: 1-8.
- Aydın OA, Karaosmanoglu HK, Karahasanoglu R, Tahmaz M, Nazlıcan O (2013) Prevalence and risk factors of osteopenia/osteoporosis in Turkish HIV/AIDS patients. Braz J Infect Dis 17: 707-11.
- Jacobson DL, Spiegelman D, Knox TK, Wilson IB (2008) Evolution and predictors of change in total bone mineral density over time in HIV infected men and women in the nutrition for healthy living study. J Acquir Immune Defic Syndr 49: 298-308.
- Grant PM, Kitch D, McComsey GA, Dube MP, Haubrich R, et al. (2013) Low baseline CD4+ count is associated with greater bone mineral density loss after antiretroviral therapy initiation. Clin Infect Dis 57: 1483-8.
- Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P (2012) Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. AIDS 26: 825-31.
- Negredo E, Langohr K, Bonjoch A, Pérez-Alvárez N, Estany C, et al. (2018) High risk and probability of progression to osteoporosis at 10 years in HIV-infected individuals: the role of PIs. J Antimicrob Chemother 73: 2452-9.
- Gallant JE, Staszewski S, Pozniak AL, DeJesus E, Suleiman JM, et al. (2004) Efficacy and safety of tenofovir DF vs stavudine in combination therapy in antiretroviralnaive patients: a 3-year randomized trial. JAMA 292: 191-201.
- Young B, Dao CN, Buchacz K, Baker R, Brooks JT (2011) Increased rates of bone fracture among HIV-infected persons in the HIV Outpatient Study (HOPS) compared with the US general population, 2000-2006. Clin Infect Dis 52: 1061-8.
- Prior J, Burdge D, Maan E, Milner R, Hankins C, et al. (2007) Fragility fractures and bone mineral density in HIV positive women: a case-control population-based study. Osteoporos Int 18: 1345-53.
- Hasse B, Ledergerber B, Furrer H, Battegay M, Hirschel B, et al. (2011) Morbidity and aging in HIV-infected persons: the Swiss HIV cohort study. Clin Infect Dis 10: 1093.
- Ilha TASH, Comim FV, Copes RM, Compston JE, Premaor MO (2018) HIV and Vertebral Fractures: a Systematic Review and Metanalysis. Sci Rep 8: 7838.
- Yin MT, Shi Q, Hoover DR, Anastos K, Sharma A, et al. (2010) Fracture incidence in HIV-infected women: results from the Women’s interagency HIV study. AIDS 24: 2679-86.
- Masyeni S, Utama S, Somia A, Widiana R, Merati TP (2013) Factors influencing bone mineral density in ARV-naive patients at Sanglah Hospital, Bali. Acta Med Indones 45: 175-9.